Osteoblastoma was first described in 1956 by Lichenstein and Jaffe.1,2 It represents 0.8–1% of all bone tumors and affects young adults, with male preponderance.3 It predominantly affects the axial skeleton and vertebrae with only 14–20% of tumors affecting the skull. The most commonly affected sites are maxilla, temporal, sphenoid, occipital, ethmoid and frontal bones. Histologically it is a benign, vascular, osteoblastic tumor with variable osteoid mineralization and absent mitotic activity or atypia.4 It can however manifest aggressive behavior, invading the surrounding tissues.5
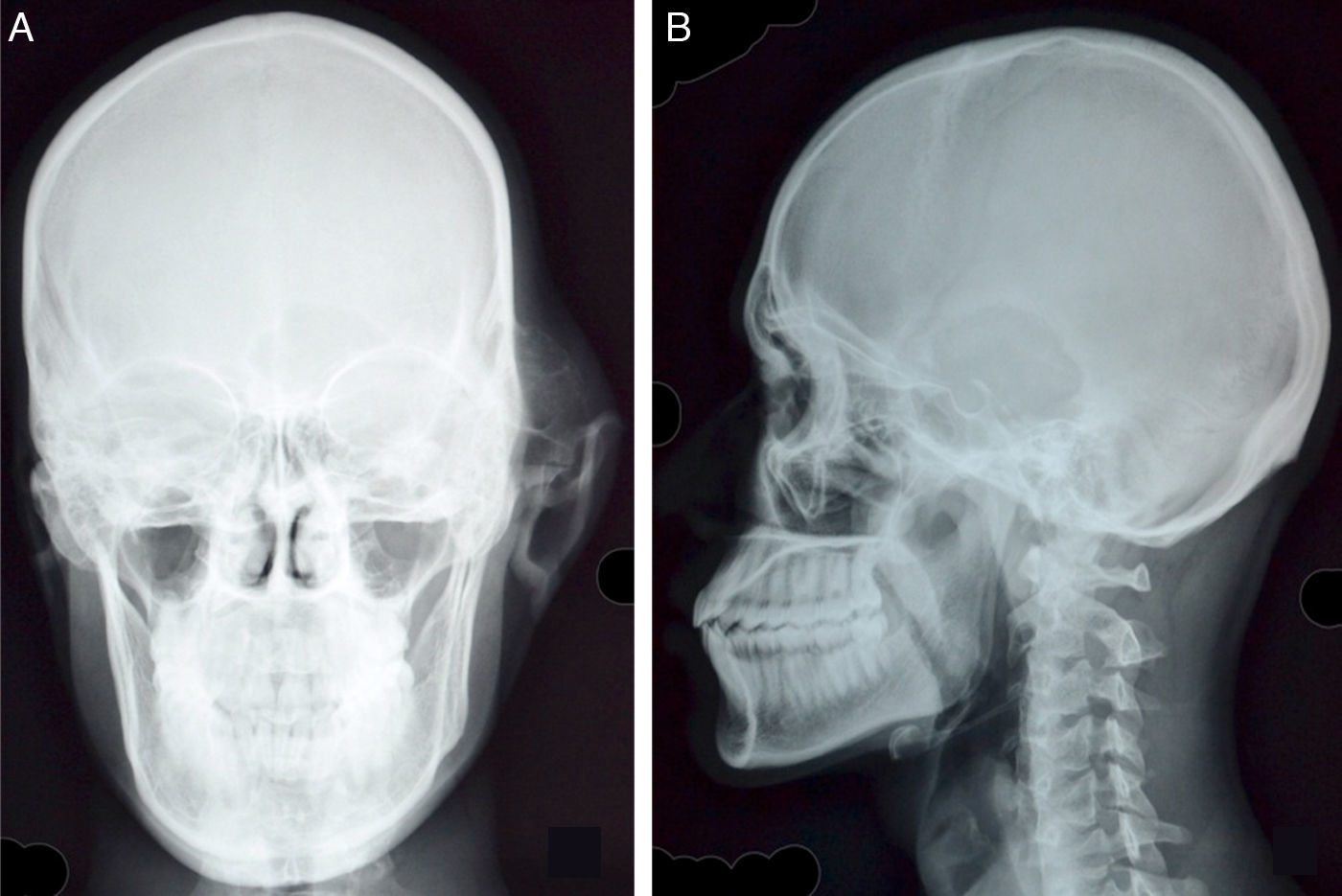
Case reportA 20 year old male presented with hearing loss, tinnitus in left ear, hard, tender swelling in the preauricular and temporal regions and deviation of mouth toward the right with duration of four years. The external auditory canal was occluded by a mass of similar hard consistency. Pure tone audiometry revealed conductive hearing loss. Plain radiograph skull PA and lateral view revealed a geographic, punched out lytic, expansile lesion involving the left temporal bone and left greater wing of sphenoid with markedly thinned-out outer cortex and lateral displacement of pinna. No evidence of matrix calcification was seen (Fig. 1A and B).
(A) Skull PA view reveals swelling of osseus origin overlying left temporal bone with thinned out cortex and interlacing septae. There is associated breach in the cortex of left greater wing of sphenoid and non-visualization of left petrous bone. Soft tissue swelling and lateral displacement of left pinna is seen. (B) Lytic, geographic lesion in left temporal bone with, narrow zone of transition and irregular, sclerotic margins is well appreciated on the lateral view.
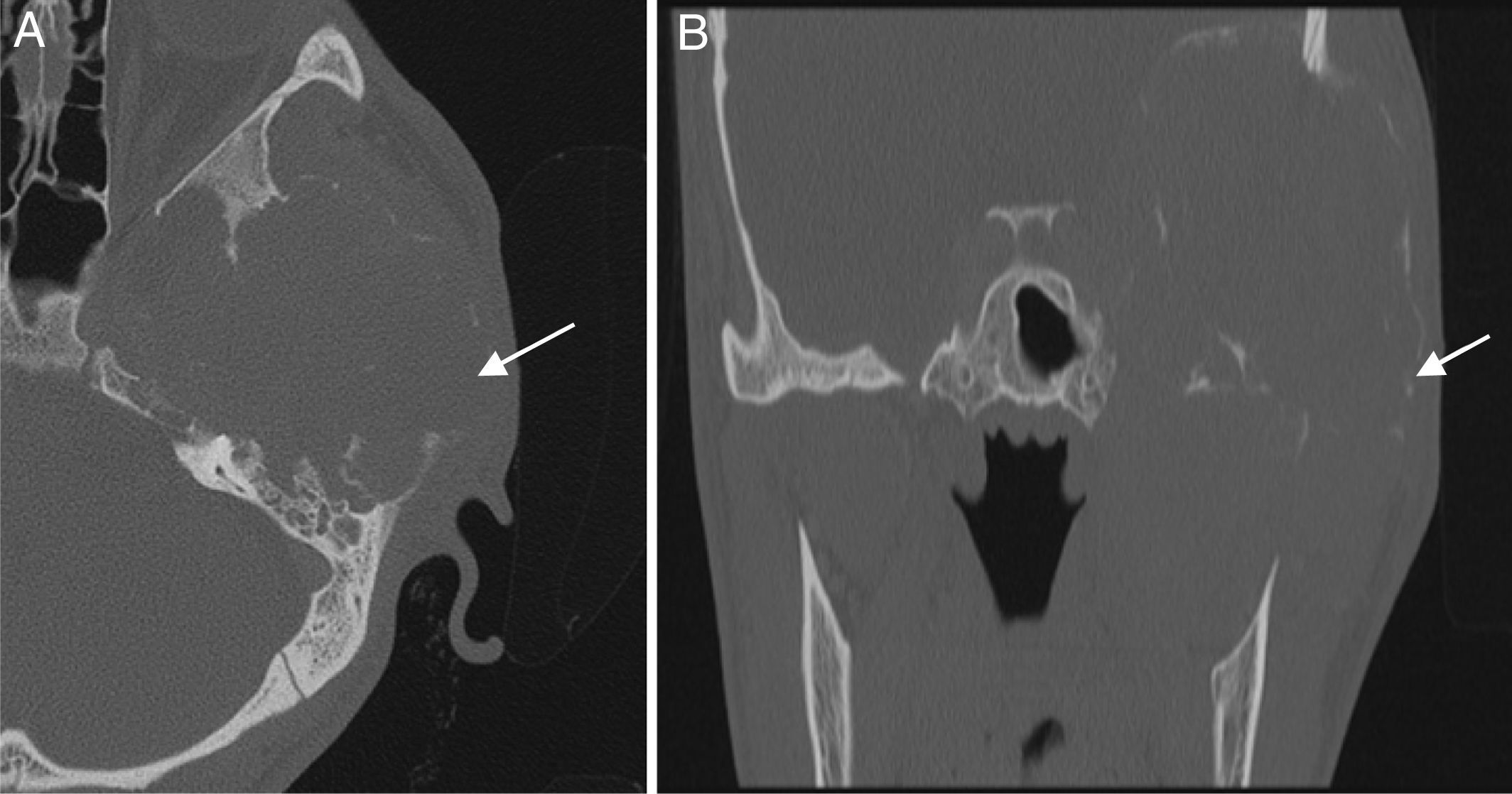
On contrast enhanced computed tomography and high resolution computed tomography, a large, expansile, lytic lesion measuring 5cm×6cm×5.5cm involving the left temporal bone with involvement of mastoid air cells, middle ear cavity and partial erosion of inner ear structures was seen. The lesion had also eroded the left greater wing of sphenoid, left petrous bone and petrous apex (Fig. 2A and B). Soft tissue window film showed enhancement of the soft tissue within the lesion (Fig. 3). In this case, the patient underwent partial resection and curettage of the lesion. The final diagnosis was based on histopathological findings, which revealed a giant cell lesion with osteoblast-like cells.
(A and B) High resolution axial and coronal CT image of left temporal bone reveals extensive cortical destruction involving left greater wing of sphenoid, squamous part and anterior margin of petrous part of left temporal bone. The mastoid air cells are eroded with opacification of mastoid air cells. The middle ear cavity and ossicles are completely destroyed by the mass. Note the extremely thin shell of bone outlining the lesion (arrows).
On soft tissue window settings, the lesion shows enhancing soft tissue with a large intracranial component causing mass effect and mild white matter edema in the adjacent temporal lobe and a small superficial component in the scalp. A few small specks of matrix mineralization are noted as well.
Osteoblastomas are rare bone tumors. They are histologically benign, osteoid-forming vascular neoplasms and constitute a small percentage of the primary bone tumors.
Clinically the symptoms are usually non-specific, including insidious, localized pain which is unresponsive to anti-inflammatory drugs.6 There may be erythema and soft tissue swelling over the area of growth.4 When the tumor affects the temporal bone and middle ear structures, it can lead to facial nerve palsy and progressive hearing loss due to compression of adjacent structures.7
Radiologic examination is necessary and helps in the characterization and definition of the extent of the lesion, though establishing a definitive diagnosis requires a histopathological exam.8
Pochaczevesky et al. in 1960 described osteoblastomas on roentgenograms as “osteolytic expanding lesions with evidence of some bone formation or varying degree of calcification”. In addition, they demonstrate well circumscribed, sclerosed borders with narrow zones of transition.9
When compared with plain radiography, CT gives better information regarding the intraosseus extent, tumor origin, and growth into the adjacent soft tissues.10 Osteoblastomas have been described as a well circumscribed, expansile, lesion with traces of calcification and contrast enhancement. It can demonstrate mixed lytic and sclerotic components with evidence of bony destruction. In addition to the lesion extent, vascularity assessment has been done in some cases with CT angiography for the therapeutic decision plan.3
On MR the signal is variable, ranging from T1 hypointensity and T2 hyperintensity to both T1 and T2 hypointensity.10 In calvarial lesions, it provides important information on surrounding brain parenchyma and cranial nerve involvement.
In spite of a benign nature, it demonstrates increased uptake on nuclear scans (18F-FDG PET and Technetium-99).
Because of its benign nature, most authors’ recommend that osteoblastomas should be treated conservatively, e.g. using curettage and partial resection. However, because of higher rates of recurrence after curettage (up to 20%), a few authors recommend complete resection.
The differential diagnosis includes osteoid osteoma, osteosarcoma giant cell tumor, aneurysmal bone cyst, fibrosarcoma, and chondrosarcoma.4 Osteoid osteoma is an important differential, varying from osteoblastoma in aspects of size, location, clinical and radiological presentation. Osteoid osteoma is smaller and is in most instances located in the bony cortex, having a sclerotic nidus. They also differ in size: osteoid osteoma measures typically less than 2cm and osteoblastoma is larger. Osteoblastoma conversely is situated in medulla. Osteoid osteoma characteristically causes nocturnal pain which is relieved by salicylate therapy and demonstrates no soft tissue mass.
It is important to distinguish osteoblastoma from the malignant tumor osteosarcoma. The latter is radiologically aggressive with new bone formation, wide zone of transition, aggressive pattern of growth and may produce periosteal reaction. Histologically it is hypercellular with high mitotic activity and areas of necrosis.8
Giant cell tumors (also known as osteoclastoma) are epiphyseal tumors, seen in skeletally mature adults. Radiographically, they are purely lytic with well-defined and non-sclerotic margins.
An aneurysmal bone cyst is a solitary expansile well-defined osteolytic bone lesion, commonly occurring in metaphysis of long bones. CT or MRI may reveal fluid levels, representing layering blood products.11 The presence of enhancement of the soft tissue in our case refutes the diagnosis of primary aneurysmal bone cyst.
ConclusionThe occurrence of benign osteoblastoma in the temporal bone and middle ear is rare. A high degree of clinical suspicion with radiologic and pathologic examination is necessary for diagnosis. Cross sectional imaging like CT and MRI are extremely useful for describing the osseous lesion and involvement of adjacent soft tissues with confirmation of diagnosis on histopathological examination.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Dixit R, Gupta S, Chowdhury V, Khurana N. Aggressive osteoblastoma of the temporal bone: an unusual cause of facial palsy. Braz J Otorhinolaryngol. 2018;84:119–21.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.