Abused children and adolescents are exposed to factors that can trigger vocal changes.
ObjectiveThis study aimed to analyze the prevalence of vocal changes in abused children and adolescents, through auditory-perceptual analysis of voice and the study of the association between vocal changes, communication disorders, psychiatric disorders, and global functioning.
MethodsThis was an observational and transversal study of 136 children and adolescents (mean age 10.2 years, 78 male) who were assessed by a multidisciplinary team specializing in abused populations. Speech evaluation was performed (involving the aspects of oral and written communication, as well as auditory-perceptual analysis of voice, through the GRBASI scale). Psychiatric diagnosis was performed in accordance with the DSM-IV diagnostic criteria and by applying the K-SADS; global functioning was evaluated by means of the C-GAS scale.
ResultsThe prevalence of vocal change was 67.6%; of the patients with vocal changes, 92.3% had other communication disorders. Voice changes were associated with a loss of seven points in global functioning, and there was no association between vocal changes and psychiatric diagnosis.
ConclusionThe prevalence of vocal change was greater than that observed in the general population, with significant associations with communication disorders and global functioning. The results demonstrate that the situations these children experience can intensify the triggering of abusive vocal behaviors and consequently, of vocal changes.
Crianças e adolescentes vítimas de maus tratos estão expostas a fatores que podem desencadear alterações vocais.
ObjetivoAnalisar a prevalência de alteração vocal nesta população realizando análise perceptivo-auditiva da voz e estudar a associação entre alteração vocal, transtornos da comunicação, transtorno psiquiátrico e funcionamento global.
MétodoEstudo observacional e transversal. Participaram 136 sujeitos, com idade média de 10,2 anos, atendidos por equipe multidisciplinar especializada no tratamento ambulatorial de vítimas de maus tratos. Foi realizada avaliação fonoaudiologia (aspectos da comunicação oral e escrita e análise perceptivo-auditiva da voz a qual foi feita por meio da escala GRBASI). O diagnóstico psiquiátrico foi dado de acordo com os critérios diagnósticos da CID-10 e aplicação do K-SADS; o funcionamento global foi avaliado por meio da escala C-GAS.
ResultadosA prevalência de alteração vocal foi de 67,6%, dos pacientes com alteração vocal, 92,3% apresentaram outros transtornos da comunicação. A alteração vocal está associada a um prejuízo de sete pontos no funcionamento global e não apresentou associação com transtorno psiquiátrico.
ConclusãoA prevalência de alterações vocais encontrada foi maior do que a observada na população geral, com associações significantes com transtornos da comunicação e funcionamento global. As situações que estas crianças vivem podem intensificar o desencadeamento de comportamentos vocais abusivos e consequentemente de alterações vocais.
Violence against children and adolescents is considered to be a public health problem due to the many negative consequences to biopsychosocial development,1 such as internalizing and externalizing problems,2,3 below average intellectual function,3 academic and school performance impairment,4,5 as well as oral and written communication disorders.6,7
Oral language, one of the most elaborate forms of human communication, allows the child to organize his/her perceptions, acquire knowledge, and build memories. It provides not only social interaction, but also the learning and use of rules to regulate one's own behavior and emotional state.8 Oral language acquisition disorders can impair learning9 and cause social, emotional, and behavioral problems.10,11
Successful communication depends not only on the content of what is said, but also on the manner and attitude that the speaker assumes during the interaction. Specifically, facial expressions and vocal modulations during oral emission convey the speaker's emotional state and intention.12 Thus, the production and recognition of specific characteristics of the speaker contribute to effective communication.
The voice is an innate neurophysiological function, resulting from a sophisticated muscular processing. Through its flexibility, it acts as a sensitive indicator of the speaker's emotions, attitudes, physical condition, and sociocultural role.13
Any difficulty or alteration in vocal emission that prevents natural voice production characterizes dysphonia,14 an increasingly common observation, with a prevalence of 6%–37%.15–17
Genetic and environmental components influence the onset of vocal symptoms in different ways: the genetic effect is moderate, while the environmental effects are the more important factors in the onset of dysphonia.18
The causes of dysphonia include premature birth;19 nasal obstruction;20 allergic pulmonary reactions, such as asthma and bronchitis; gastroesophageal reflux; auditory symptoms;16 and sleeping problems.21 The main cause, however, is vocal abuse by children, as indicated by studies with dysphonic children (90.3%,22 45.2%,23 and 54.67%24). The rapid and continuous collision of the vocal folds during phonation causes trauma to the mucosal capillaries, edema, and initiates the process of nodule formation. Lesions such as cysts, sulci, paralysis, and papillomatosis may also occur.24
Knowing that voice changes in childhood can interfere with emotional development and socialization of children,25 the identification and care of these disorders are important to allow for the child's global functioning, helping to promote physical and emotional health.
Childhood victims of abuse are exposed to some factors related to dysphonia, as they grow in environments where yelling is very common among adults. The street experience also becomes an aggravating factor. Yelling very often becomes a way of standing up for oneself in the face of difficulties, in addition to the fact that these individuals are directly exposed to environmental aggressions (from pollution to climate aspects) and drug use. It is, therefore, a population more likely to show changes in vocal patterns.
The aim of this study was to assess the prevalence of voice disorders in this population and the association of these changes with other communication disorders, psychiatric disorders, and global functioning through the auditory-perceptual analysis of voice in children and adolescents victims of abuse.
MethodsA cross-sectional observational study was conducted after the approval of the Research Ethics Committee, protocol number 4353.
The participants were 136 children and adolescents treated between January 2010 and July 2012 by a multidisciplinary team specializing in outpatient treatment of victims of abuse. These children are referred to this service by the technical staff of the shelters where they live or by Child Protective Services. The mean age of participants was 10.2 years, and 78% were males. The criteria for patient inclusion in the study were age 6–18 years; at least one social diagnosis (Z55–Z65 – Persons with potential health hazards related to socioeconomic and psychosocial circumstances), according to the International Classification of Diseases (ICD-10),26 and consent from the guardian for participation in the research.
Those with neurological problems and psychiatric symptoms that could impair the understanding of the evaluation, such as patients with delusions, were excluded. Patients who were already undergoing speech therapy were also excluded.
For the speech therapy assessment, specific tests were used in the areas of oral language,27,28 written language,29 and speech.30 The diagnoses were classified as phonological disorders, alteration of semantic-syntactic skills, changes in pragmatic capacities, receptive-expressive language disorder, written language disorder, articulation disorder, and dysfluency.
For voice analysis, samples of spontaneous speech were collected, as well as of connected speech, vocal emissions, and singing voice, recorded on a digital recorder; oral motor assessment was also performed. Clear and simple language was used to assess the child/adolescent, and the procedure was exemplified to facilitate the test understanding.
Several times, more than one speech sample was collected, to ensure the subsequent analysis. Speech samples were submitted to auditory-perceptual analysis by audiologists using the GRBAS31 scale, which characterizes the pattern of change, to be classified as 0 (no dysphonia) and 1, 2, and 3 (presence of dysphonia). The Japanese GRBASI scale, used internationally, is a compact and reliable method of assessing the global degree of dysphonia (G) by identifying key factors when defining a dysphonic voice: roughness (R), breathiness (B), asthenia (A), strain (S), and instability (I). For greater data reliability, two other speech pathologists specialized in voice were asked to participate. After listening to the recorded material, they completed the same evaluation protocol. Samples whose analyses showed no agreement were excluded from the sample.
Psychiatric diagnoses were made by psychiatrists specialized in child and adolescent psychiatry. The Schedule for Affective Disorders and Schizophrenia for School-Age Children/Present and Lifetime Version (K-SADS-PL)32 was applied and disorders were classified according to the DSM-IV.
The Children's Global Assessment Scale (C-GAS) involves clinical appraisal of the general level of patient functioning based on their behavior at home, with the family, at school, with friends and during leisure activities in the last three months. The scores range from 1 to 100, and scores >70 indicate normality.33
Data treatmentA descriptive analysis of the results regarding the percentage of patients with voice disorders was performed, by gender and age. Analyses of associations between vocal change and the presence of psychiatric and communication disorders were measured through Fisher's exact test.34 Comparison of measures of global functioning (C-GAS) between groups was performed using the Kruskal–Wallis,35 and the post hoc was performed using the Wilcoxon-Mann–Whitney test with Bonferroni correction for multiple comparisons. All analyses were performed using SPSS, release 14.36
ResultsAccording to the auditory-perceptual analysis of voice, 67.6% (n=92) of the patients had vocal changes, 79.3% (n=72) were younger than 12 years, and 56.5% were males. There was no statistical difference between the groups of males and females (p=0.423).
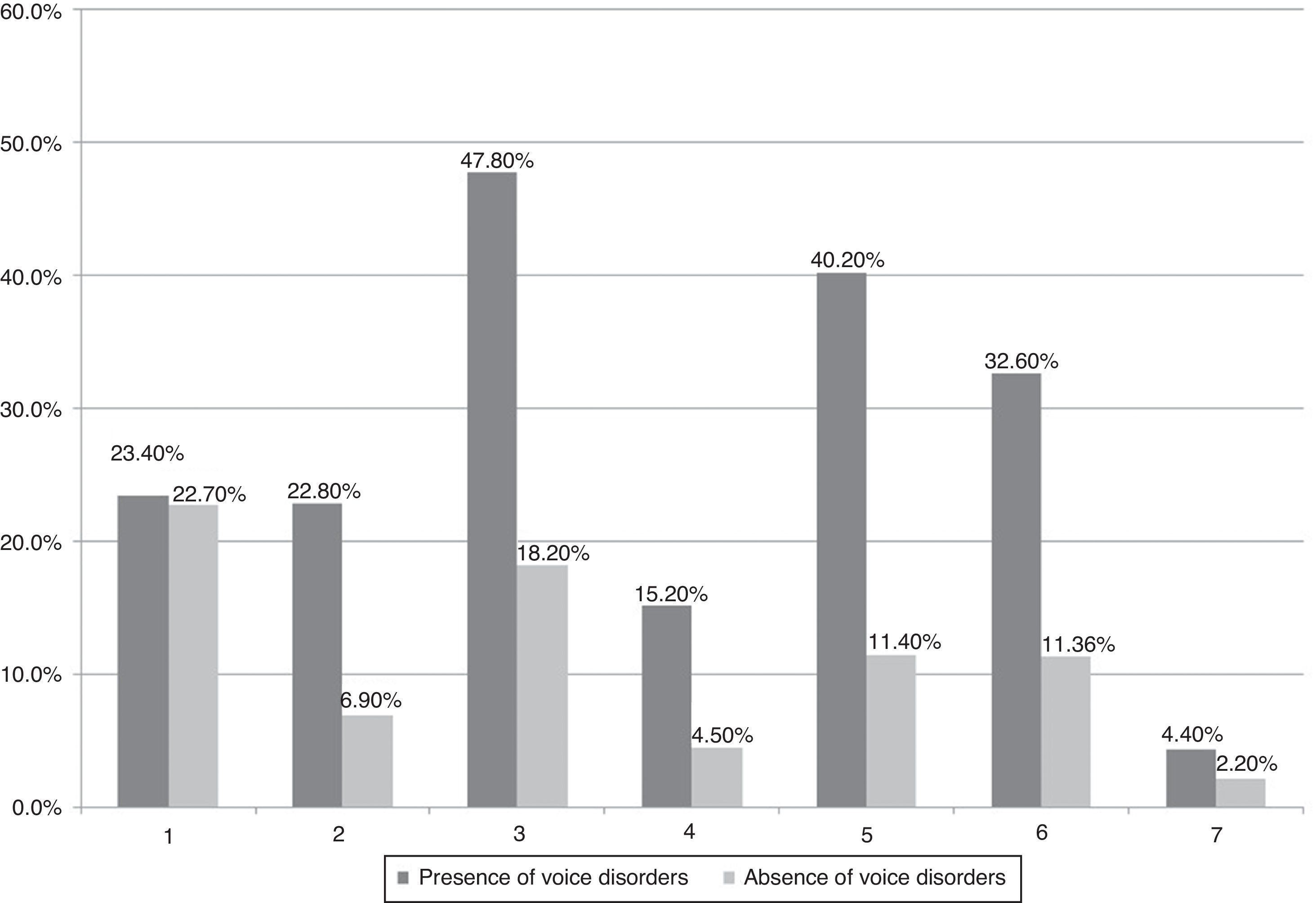
Most subjects with voice changes (92.3%) also had other communication disorders, as shown in Fig. 1. The association between the presence of vocal change and communication disorder was statistically significant in pragmatic disorders (p=0.001), articulation disorders (p=0.011), changes in semantic-syntactic skills (p=0.029), receptive-expressive language disorders (p=0.005), and written language disorder (p=0.000), indicating that individuals with these disorders showed a higher prevalence of voice changes. The pragmatic disorder may increase the occurrence of vocal change by 3.6-fold (p=0.004) and the phonetic disorder, by 3.1-fold (p=0.034).
Association between voice disorders and other disorders of oral communication in 136 children and adolescent victims of abuse (1, Phonological disorder; 2, Alteration in semantic-syntactic skills; 3, Alteration in pragmatic skill; 4, Receptive-expressive language disorder; 5, Written language disorder; 6, Articulation disorder; 7, Speech disfluency).
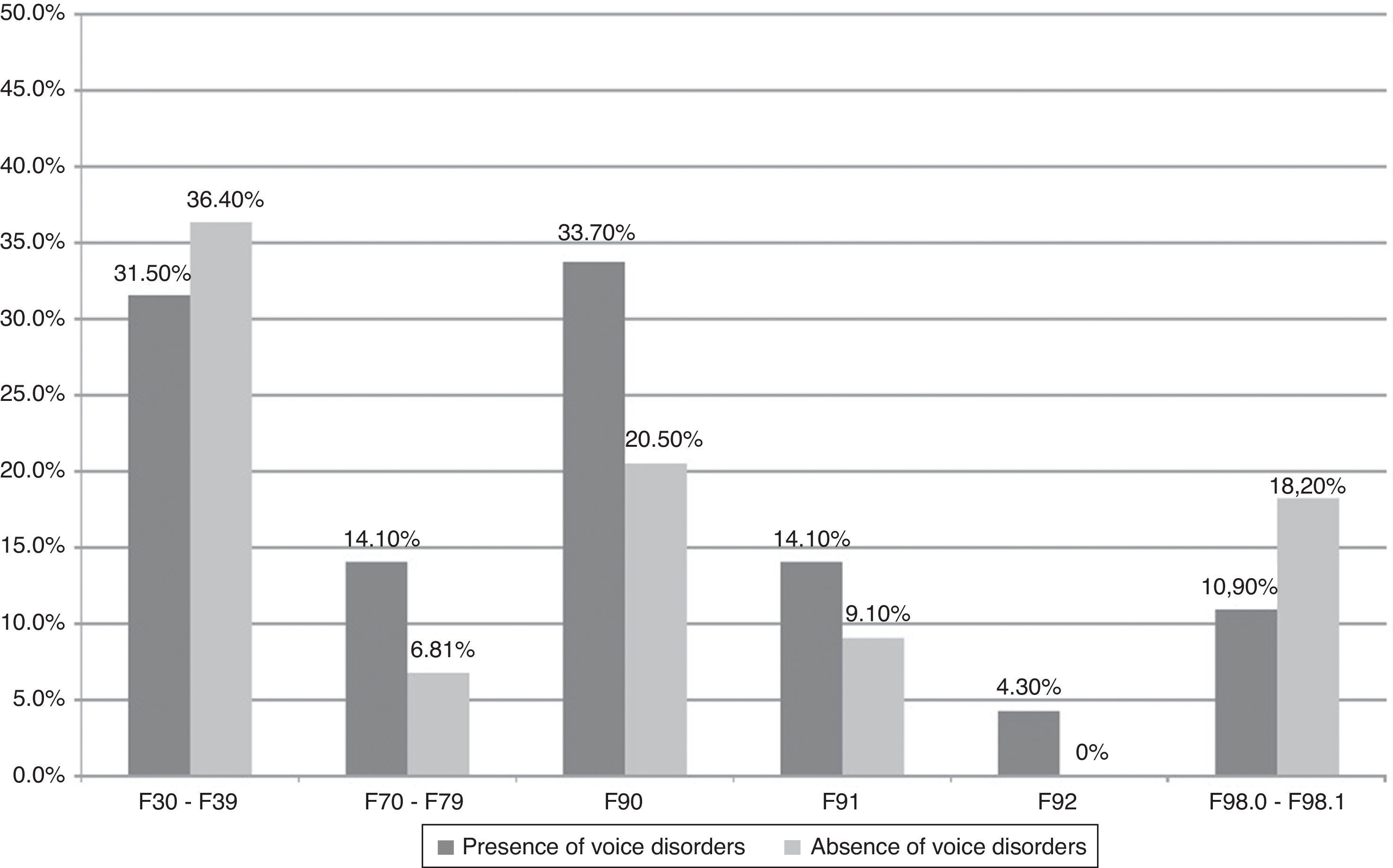
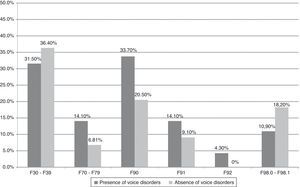
Fig. 2 shows the percentage of presence and absence of vocal disorders in psychiatric disorders, distributed in the most prevalent DSM-IV diagnostic categories in this sample. Although a higher proportion of voice changes was observed in children with hyperkinetic disorders and mental retardation, there was no statistically significant association between these variables (mood disorders, p=0.697; mental retardation, p=0.266; hyperkinetic disorders, p=0.159; disorders of conduct, 0.581; mixed disorders of conduct and emotions, p=0.304; enuresis and encopresis of nonorganic origin, p=0.282).
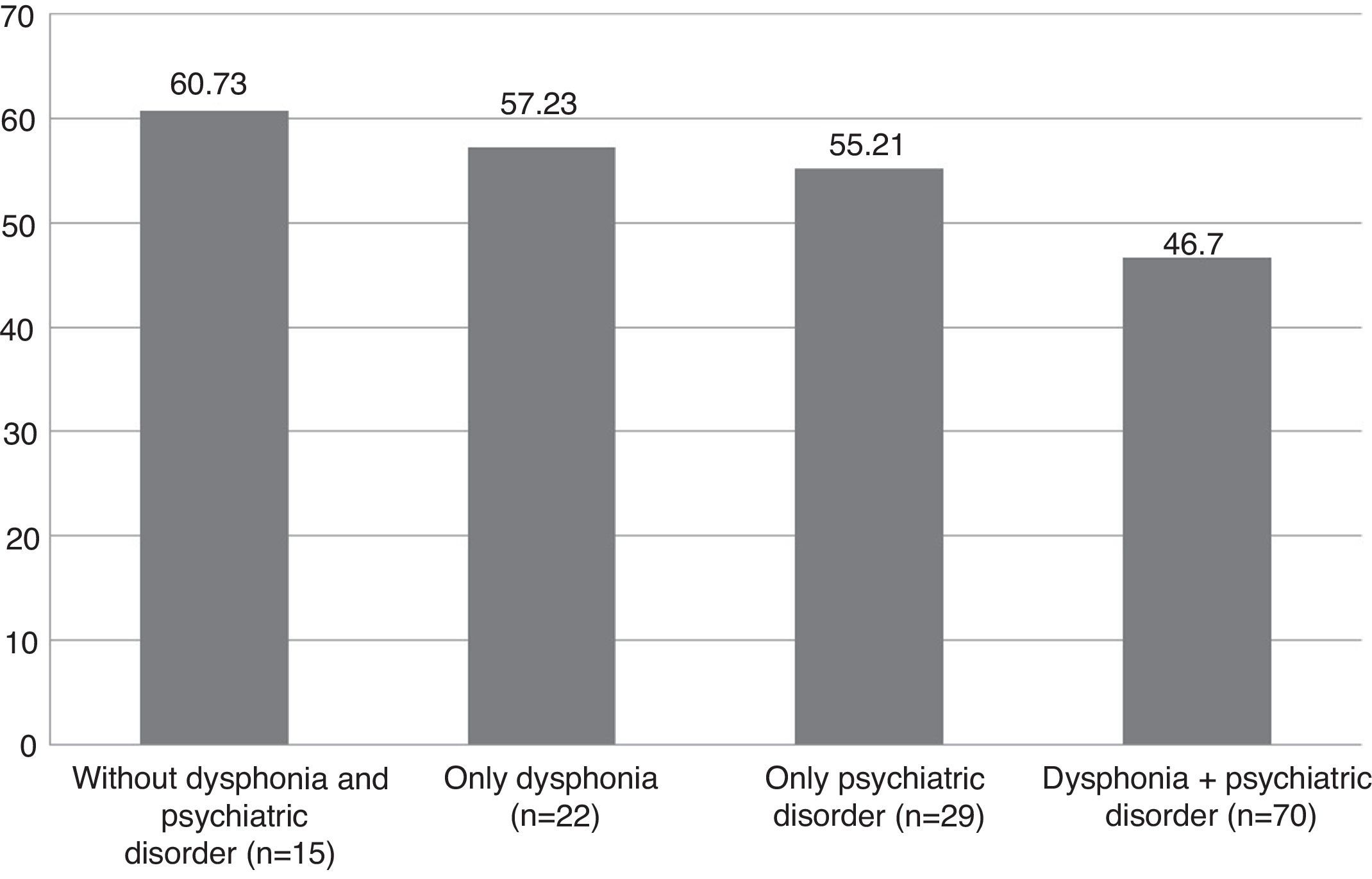
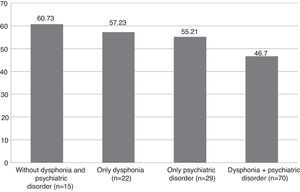
To verify the subjects’ global functioning, they were divided into four groups according to the presence or absence of vocal and psychiatric disorders. The mean global functioning (C-CGAS) for each group was below the level of normality and can be seen in Fig. 3.
The global functioning scores of participants without a disorder and in groups with vocal changes or psychiatric disorders were found to be between 51 and 60, which corresponds to children with some problems in more than one area. Participants who have voice changes and psychiatric disorders have a global functioning in the range 41–50, which corresponds to children with obvious problems, deficits in most areas, or severe deficits in one area. Statistical analysis showed no association between voice changes and psychiatric disorders (p=0.289) for global functioning. However, the presence of voice change was associated with a loss of seven points in the CGAS (p=0.002), whereas the presence of a psychiatric disorder was associated with a loss of 8.6 points (p<0.001).
DiscussionThe aim of this study was to determine the prevalence of vocal changes in children and adolescent victims of abuse, and to study the association between voice disorders and communication and psychiatric disorders, as well as global functioning.
The results indicate a prevalence of voice disorders higher than that observed in the general population; higher prevalence of voice disorders in individuals with communication disorders (significant association); no significant association between voice disorders and psychiatric disorders; and association between voice changes and loss of seven points in global functioning.
We observed a higher prevalence of voice disorders than that described in studies on childhood dysphonia, where the prevalence ranges from 6% to 37%15–17; this suggests that the factors to which children and adolescent victims of abuse are exposed may increase the risk for the development of vocal disorders.
Deviant vocal behavior is a form of interaction, aggression, leadership, and a way to become accepted by a group, and represents the result of the interaction of anatomical, physiological, social, emotional, or environmental factors.37
One of the factors that could trigger voice changes in this study population was the disorganized environment in which they lived or still live. Families with troubled dynamics, crowded shelters and lack of individualized attention, or even the streets, where the most efficient communication is not always the socially accepted type, are three risk factors for the onset of vocal disorders. The individual produces vocal modulations that are specific for each type of situation experienced (happiness, sadness, and anger, among others) and environmental factors can cause them to make motor adjustments and change the physiological mechanisms, so that the voice meets their needs. Studies indicate that factors such as divorce, separation, abnormal life conditions, too many adults in the environment, impaired parent–child relationships, and unusual kinship relations were associated with the incidence of dysphonia in 42% of the assessed children.13 Children born to depressed mothers are less responsive to faces and voice and interact less with their mothers.38
If these children and adolescences need to change the vocal pattern to meet their communication needs, it can be inferred that an impediment (whether organic or functional) in some aspect of message transmission can worsen the vocal disorder and intensify voice changes. Distortions in the production of speech sounds due to changes in the position of the teeth in the dental bite, in the tone of the lips, tongue and cheeks, and in breathing change the movement of the phonoarticulatory tract, and can also cause vocal disorders. Similarly, children with fewer language resources to understand the environment and work out their needs through an efficient speech, make use of other means such as yelling, interrupting, crying, talking excessively, which characterizes an abusive vocal behavior that also triggers voice alterations.
Other disorders of communication, not assessed in this study, such as hearing loss and auditory processing difficulties, are more common in children and adolescent victims of abuse,39 which prevents the auditory feedback of their own speech and causes disorders in the vocal fold movement.
Although no association was observed between vocal and psychiatric disorders in this study, it is known that abused individuals exhibit certain characteristics, such as low self-esteem; low tolerance to frustration; difficulty establishing trust and attachment; and behavioral, communication, and interpersonal skill problems. Behaviors such as agitation, motor restlessness, impulsiveness, inattention, anxiety, and insecurity lead to abusive and prolonged vocal behaviors, such as talking too much or at an increased speech velocity, raising the vocal intensity, yelling, and sudden vocal attack, which overloads the apparatus.
For instance, a high-pitched voice may in some cases reflect tension in the intrinsic muscles of the larynx resulting from anxiety states. More insecure individuals tend to use a higher-pitched voice and lower intensity, word pronunciation tends to be imprecise, and they normally use a more restricted voice modulation, which can give a more monotonous speech.40,41
Changes in behavior, with physical and verbal aggression, often appear to substitute the socially structured behavior and communication in children and adolescents at social risk. This form of expression is essential in the streets, and is often related to survival and an important possibility to demonstrate the feelings of being ignored by society – it is a way to be seen and heard in relation to their needs and desires. Moreover, in shelters, episodes of psychomotor agitation can be interpreted as a clear sign of the need for individualized attention. Thus, one must consider that this type of behavior and expression, both physical and verbal, is part of the interaction process of these children with the world around them and that it has its role.42
There was no difference between genders for voice alterations, which differs from other studies that indicated a prevalence of voice disorders in boys.22–24,43,44 Researchers highlight that the behavior of boys is more impulsive and aggressive than that of girls, who more typically exhibit hyperactivity, anxiety, and leadership; the male behaviour when translated to the phonation mechanisms results in vocal abuse. However, among the population of victims of abuse, girls also need the abusive use of voice to communicate and meet their needs, which could explain the absence of gender differences in this study.
Difficulties in communication and behavioral and emotional problems cause impairment of social skill,45,46 as well as academic achievement and school engagement limitations,47 which characterizes a global functioning that is below expectations. Although the vocal change has an impact on overall health, on communication efficiency, on educational and social development, self-esteem, self-image, and participation in group activities,48 in the present study a causal association between voice disorders and global functioning could not be inferred, given the complexity of the involved factors.
Another limitation refers to the vocal assessment used. The scale used in the present study for the auditory-perceptual analysis of voice was employed in other recent studies and considered to be an excellent means of vocal assessment.16,49 However, the researchers suggest the performance of otorhinolaryngological examinations to verify the presence of vocal fold lesions.
Martins et al.24 identified 57.5% of vocal nodules at the videolaryngoscopic assessment. In this study, patients were initially referred to the otorhinolaryngology service of the city health care network for examination and treatment, if necessary. However, the authors do not have the results of these evaluations yet, which they intend to address in a future study. Another salient point is that the children's attitudes and those of their interlocutors were not assessed in the physical, social/emotional, and functional domains. The authors indicate the inclusion of subjective voice analysis through interviews with parents/tutors and the children themselves, in order to include specific techniques to reduce the abusive vocal behavior.50
ConclusionChildren victims of abuse have a high prevalence of voice disorders, mainly associated with communication disorders and impaired global functioning. Characteristics of this population, such as living in unsanitary places, disturbed interpersonal relationships, behavioral and emotional problems, and communication difficulties can constitute a complex picture associated with abusive vocal behavior. Otorhinolaryngological evaluation, as well as the assessment of the attitudes of children and caregivers, should be considered in order to complement the vocal assessment and improve the management of this population.
FundingThis study was supported by Research Grant – Fundação Faculdade de Medicina.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Stivanin L, dos Santos FP, de Oliveira CC, dos Santos B, Ribeiro ST, Scivoletto S. Auditory-perceptual analysis of voice in abused children and adolescents. Braz J Otorhinolaryngol. 2015;81:71–8.
Institution: Programa Equilíbrio, Departamento e Instituto de Psiquiatria do Hospital das Clinicas, Faculdade de Medicina da Universidade de São Paulo (FM-USP), São Paulo, SP, Brazil.