The effects of the Coronavirus SARS-Cov-2 (COVID-19) have been related to different clinical presentations, unpredictable evolutions, and outcomes. Otological and neurological complaints have also been associated with COVID-19, including deafness.1 As with other viruses, the pattern is a Sensorineural Hearing Loss (SNHL) from mild to profound.
In cases of severe to profound SNHL, Cochlear Implant (CI) would be indicated, however, surgical implications and performance in COVID-patients have yet to be studied.2 We present a case of a patient with bilateral profound SNHL post-COVID-19 who underwent simultaneous bilateral CI surgery.
Case reportA 55-year-old male with a past medical history of hypertension, hypothyroidism and anxiety presented symptoms described as cough, headache, and fever on March 11st 2021. He was positive for SARS-CoV-2 and did not clinically improve with analgesics. On March 19th he was admitted in Intensive Unit Care (IUC) for acute respiratory syndrome.
During hospitalization, he was intubated and had acute renal failure, undergoing mechanical ventilation and hemodialysis. Cefepime was associated with vancomycin. Ten days later, he presented worsening hemodynamics conditions. Antibiotics had been staggered to Meropenem and a tracheostomy was performed. One month later, he presented a convulsive crisis status witnessed in electroencephalogram and new cultures showed Pseudomonas, treated with Piperacillin Sodium-Tazobactam.
On May 12th, he started daily interruption of sedatives and eight days later, he complained of bilateral hearing loss. An audiogram showed no response and Brain Evoked Response Audiometry (BERA) confirmed bilateral profound SNHL. After 98 days hospitalized, he was discharged to a rehabilitation center. Until that moment, patient had no previous vaccination for COVID-19.
On March 2022 he was referred to our center, complaining of bilateral anacusis and a sporadic tinnitus described as “machine noise”. His otoscopy and Computed Tomography (CT) were normal. Magnetic Resonance Imaging (MRI) showed increased signal on T2 and FLAIR in the periventricular white matter suggesting alteration of microangiopathy nature.
Audiometric test has showed a profound SNHL in both ears. Speech Reception Threshold (SRT) could not be defined. Tympanograms were normal and acoustic reflexes were absent. Speech perception test was 0% in open-set and closed-set. Transiently evoked and distortion-product otoacoustic emissions were absent.
Bilateral cochlear implantation was performed with a Nucleus CI622 device. During surgery, it was noted middle ear mucosal hyperplasia, without any effusion. Full insertion of electrodes array occurred without complications and no sign of cochlea ossification. Impedance field telemetry determined integrity bilaterally.
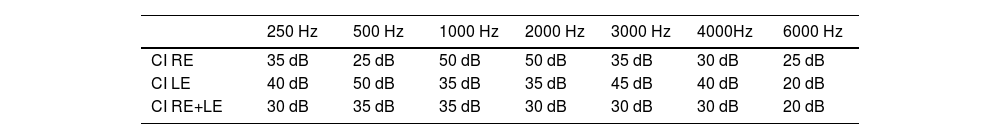
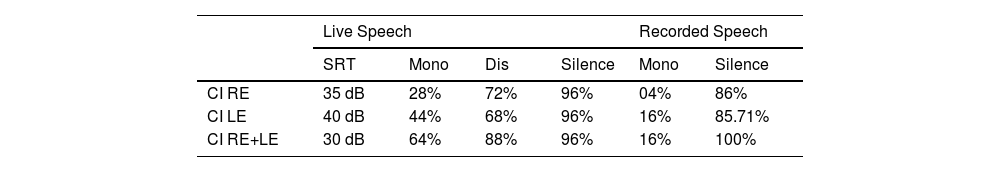
During initial activation, patient reported reasonable hearing and improving of tinnitus. Postoperative pure-tone audiometry two months after activation showed improvement of SRT, mainly with both implants (Table 1). Patient achieved 88% intelligibility of disyllables and 64% of monosyllables at 65dB with both CI. He scored 96% on sentence recognition on silence at 65dB (Table 2). Currently, he continuously reports improvement on understanding and tinnitus.
Postoperative pure-tone audiometry 2 months after CI activation.
| 250 Hz | 500 Hz | 1000 Hz | 2000 Hz | 3000 Hz | 4000Hz | 6000 Hz | |
|---|---|---|---|---|---|---|---|
| CI RE | 35 dB | 25 dB | 50 dB | 50 dB | 35 dB | 30 dB | 25 dB |
| CI LE | 40 dB | 50 dB | 35 dB | 35 dB | 45 dB | 40 dB | 20 dB |
| CI RE+LE | 30 dB | 35 dB | 35 dB | 30 dB | 30 dB | 30 dB | 20 dB |
CI, Cochlear Implant; LE, Left Ear; RE, Right Ear.
Postoperative Speech Perception 2 months after CI activation.
| Live Speech | Recorded Speech | |||||
|---|---|---|---|---|---|---|
| SRT | Mono | Dis | Silence | Mono | Silence | |
| CI RE | 35 dB | 28% | 72% | 96% | 04% | 86% |
| CI LE | 40 dB | 44% | 68% | 96% | 16% | 85.71% |
| CI RE+LE | 30 dB | 64% | 88% | 96% | 16% | 100% |
CI, Cochlear Implant; LE, Left Ear; Mono, Monosyllables; Dis, Disyllables; RE, Right Ear; SRT, Speech Recognition Threshold.
Patient consent and Universidade Federal de São Paulo Institutional Review Board approval were obtained under number 1466/2020.
DiscussionHearing loss related to COVID-19 has been reported worldwide. However, there are a restricted number of cases with indication for Cochlear Implant (CI) and few studies that present its outcomes in this specific population.
The pathophysiology of COVID-related SNHL is not completely understood and degree and duration of this sequel is still unpredictable. Furthermore, the association between SNHL and SARS-CoV-2 can be biased by confounding factors. Assuming a direct cochlear involvement, with ossification and fibrosis, CI surgery should not be postponed in order to insert the electrode array without complications.1 Such urgency was noted in one described case,3 with MRI suggesting inflammatory process in the cochlea. Another theory would be thromboembolism and the vasculitis4 probably linked to increased Angiotensin-Converting Enzyme 2 (ACE2) and an excess of cytokines. In our patient, MRI showed signs of microangiopathy, which leads us to suspect a multifactorial cause: vascular aggression to the vestibulocochlear nerve and possible effect of Vancomycin. It is observed that in most patients with post-Covid deafness, it is a multiple-factorial condition.
In case of permanent neurological damage caused by COVID-19, a great CI performance would not be expected. A report of two patients5 observed a decrease in auditory performance and speech comprehension in two previously implanted children after being affected by the coronavirus. Oppositely, there are two published reports of post-covid implanted patients who also had satisfactory outcomes.1,2
ConclusionIt is consensus that patients with acute symptoms, including SNHL, should be promptly tested for COVID-19. While research is being published, audiological rehabilitation should not be postponed, including CI in cases of profound SNHL.
Authors’ contributionsAmanda Sampaio Almeida: Surgical procedure, literature review, data collection, study’s design and writing.
Fernando Yonamine: Surgical procedures and study’s writing.
Alexandra Dezani Soares: Data collection and study’s writing.
Norma de Oliveira Penido: Literature review and study’s writing.
Oswaldo Laercio Mendonça Cruz: Literature review, study’s design and writing.
All authors read and approved the final manuscript.
Conflicts of interestThe authors declare no conflicts of interest.
This work was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP process number 2021/07346-6).
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.