Balloon sinuplasty is a minimally invasive endoscopic procedure, developed with the aim of restoring patency of the paranasal sinuses ostia with minimal damage to the mucosa.
ObjectiveTo evaluate the effectiveness of balloon sinuplasty in patients with chronic rhinosinusitis.
MethodsThis was a prospective cohort study comprising 18 patients with chronic rhinosinusitis without polyposis who underwent balloon sinuplasty. Patients were evaluated for clinical criteria, quality of life (Sino-Nasal Outcome Questionnaire Test-20 [SNOT-20]), and computed tomography of the sinuses (Lund–Mackay staging) preoperatively and three to six months after the procedure.
ResultsOut of 18 patients assessed, 13 were included, with a mean age of 39.9±15.6 years. Ostia sinuplasty was performed in 24 ostia (four sphenoid, ten frontal, and ten maxillary sinus). At the follow-up, 22 (92%) ostia were patent and there was no major complication. There was symptomatic improvement (SNOT-20), with Cronbach coefficients for consistency of the questionnaire items of 0.86 (95% CI: 0.73–0.94) preoperatively and of 0.88 (95% CI: 0.77–0.95) postoperatively, the difference being statistically significant (p<0.001). In addition, there was marked reduction of the computed tomography signs, an average of 4.2 point score (p<0.001).
ConclusionSinuplasty is effective in reducing symptoms and improving quality of life as a treatment option for chronic rhinosinusitis in selected patients.
Sinuplastia com balão é um procedimento endoscópico minimamente invasivo, desenvolvido com o objetivo de restaurar a patência dos óstios dos seios paranasais com mínimo dano à mucosa.
ObjetivoAvaliar a efetividade da sinuplastia com balão em pacientes com diagnóstico de rinossinusite crônica.
MétodoEstudo de coorte, prospectivo, envolvendo 18 pacientes com rinossinusite crônica sem polipose submetidos à sinuplastia com balão. Foram avaliados critérios clínicos, qualidade de vida (SNOT-20) e tomografia computadorizada dos seios da face (estadiamento de Lund - Mackay) três a seis meses após o procedimento.
ResultadosDos 18 pacientes avaliados, 13 foram incluídos, com média de idade 39.9±15.6 anos. A sinuplastia foi realizada em 24 óstios (10 frontais, 10 maxilares e 4 esfenóides). Após acompanhamento, 22 (92%) óstios permaneceram patentes, sem ter ocorrido nenhuma complicação maior. Houve melhora sintomática (SNOT-20) com coeficiente de Cronbach para consistência dos itens do questionário de 0,86 (IC95% 0,73 - 0,94) no pré-operatório e 0,88 (IC95% 0,77 - 0,95) no pós-operatório, respectivamente, sendo estatisticamente significativa a diferença (P<0,001) e redução marcante dos sinais à tomografia, em média 4,2 pontos do escore (P<0,001).
ConclusãoSinuplastia mostrou-se efetiva para redução de sintomas e melhora da qualidade de vida como opção de tratamento da rinossinusite crônica em pacientes selecionados.
Approximately 5–15% of the Western population has chronic rhinosinusitis,1–3 which imposes an economic burden and lowers the quality of life in patients affected.4,5 Clinical treatment is still the primary approach, but patients who do not succeed undergo surgical treatment of the chronic rhinosinusitis, which has evolved considerably with the development of endoscopic surgery.
Over the past two decades, endoscopic sinus surgery had a marked progress toward less invasive approaches.6 Functional endoscopic surgery (FESS) is a procedure that preserves the normal tissues and the mucosa of the paranasal sinuses, while presenting fewer postoperative complications.7,8 Although FESS is more conservative than conventional surgery, it still might cause significant bleeding, orbit lesions, and cicatricial airway stenosis. In order to minimize such complications, the endoscopic surgery through dilatation by balloon catheter (balloon sinuplasty [BSP]) method was developed.5,6 This approach appears to cause fewer complications in comparison with other procedures to preserve tissues and mucosa of the paranasal sinuses.7,8 Some of the classic goals of FESS – open the sinus ostia and restore the normal physiology of the paranasal sinuses – also apply to BSP, in addition to the recommendation for pediatric patients with serious underlying diseases or increased anesthetic risk.7,9 The safety of BSP has already been established, but its potential complications are the same as those caused by FESS, such as cerebrospinal fluid (CSF) leak and orbital injury.5,6,9
A case series with Brazilian patients has reported the technique used in BSP,10 but information on its effect on quality of life in patients with chronic rhinosinusitis is still scarce. Therefore, this study aimed to assess the clinical and radiographic effectiveness of BSP on the quality of life of patients with chronic rhinosinusitis.
Therefore, this study aimed to evaluate clinical characteristics, including quality of life, and radiographic signs, using the Lund–Mackay score, of the effectiveness of BSP in patients with chronic rhinosinusitis without polyposis.
MethodsA longitudinal cohort study was conducted among patients with symptoms of chronic rhinosinusitis, for whom sinus surgery had been indicated. This study was approved by the Institutional Research Ethics Committee, under the protocol number 019/11, and all participants provided written informed consent for participation.
Patients aged 18–75 years, males and females, with chronic rhinosinusitis without polyposis and other complications refractory to clinical treatment, were consecutively enrolled from January of 2011 to March of 2012. Symptoms were evaluated through a standardized questionnaire with primary and secondary findings of chronic rhinosinusitis,1 and severity was assessed through the sino-nasal outcome questionnaire test (SNOT-20).11 Patients underwent an optimized treatment for chronic rhinosinusitis, based on four to six weeks of antibiotics, with or without systemic and topical steroids, and for those who did not respond to clinical treatment, sinuplasty was indicated.
In addition to physical exam, patients underwent to the sinuses computed tomography scan (CT) and rigid nasal endoscopy (30°) at the baseline. Patients who had persistent symptoms of rhinosinusitis (clinical history with two main factors or a primary combined with two secondary factors and CT findings suggestive of chronic rhinosinusitis in frontal, sphenoid, or maxillary sinus) were eligible. Those who reported previously nasosinusal tumor or surgery, nasal polyposis, or psychosocial were excluded. The procedure required, on average, 24h hospitalization after the BSP, and patients were then discharged. The follow-up was conducted approximately seven days after BSP (first postoperative visit), and a new endoscopy was performed to clean the nasal cavity. Other follow-up visits were scheduled at 15 (second visit), 30 (third), 60 (fourth visit), and 90 days after surgery (fifth visit) to perform rigid endoscopy and assess incidence of complications, such as epistaxis and adhesions. In the last visit, patients were investigated for clinical symptoms, quality of life (Sino-Nasal Outcome Questionnaire Test-20 [SNOT-20]), and a new CT scan of the sinuses was requested. In the last visit, patients were asked if they would perform the procedure again, and how much time they spent before returning to their usual activities.
Clinical and quality of life evaluationThe SNOT-20 consists of 20 questions regarding symptoms and their impact on quality of life, categorized from zero (absent) to five (highest). The instrument was administered individually at the baseline and at the last postoperative visit.
Endoscopic evaluationRigid nasal endoscopy, performed at 30°, was used to observe nasal cavities regarding mucosal secretions and polyps (Lund–Kennedy criteria).1,12 Nasal cavity was cleaned with topical anesthesia and forceps delicate for patients in need. The endoscopic staging of Lund–Kennedy12 was used for diagnostic classification purposes, based on: swelling of the nasal mucosa, presence of secretions, and assessment of bilateral polyp. Edema was scored as 0 (absent), 1 (mild to moderate), or 2 (polypoid degeneration); secretion as 0 (absent), 1 (hyaline), or 2 (thick mucus or pus); and polyp as 0 (absent), 1 (only in the middle meatus), or 2 (extending the nasal cavity). The evaluation of two nasal cavities resulted in a score ranging from 0 to 12.12
Tomography evaluationPatients underwent CT scan of the paranasal sinuses, and the films were independently assessed by two researchers, using the Lund–Mackay score,13 which determines an opacification ranging from 0 (none), 1 (partial), and 2 (total). The frontal, maxillary, anterior ethmoid, posterior ethmoid, and sphenoid sinus were individually graded, while complex ostiomeatal received a different assessment, scoring 0 (none) to 2 (opacification). The analysis of tomography was presented for each of the sinus (0–2), and an overall score for all sinuses was also calculated, ranging from 0 to 24.13
BSPPatients underwent general anesthesia and the procedure was performed under endoscopic visualization (optical 0°, 30°, and 45°); the catheter was placed near the sinus ostium. A guidewire was passed through the guide catheter and confirmed by transillumination catheter. The balloon catheter (Relieva Solo®) was then passed over the guidewire into the sinus ostium region. After the correct location of the balloon at the sinus ostia, the pressure inside the flask was gradually increased by saline infusion. After dilation, the balloon was deflated and the catheter was gradually withdrawn. Then, a catheter was placed for washing the sinus cavity with instillation of saline solution. Finally, the nasal cavity and structures of interest were reviewed before ending the procedure.
Statistical analysisStatistical analysis was performed using SPSS®, version 17.0 (Chicago, IL, United States). Paired t-test was used to compare means±standard deviations (SD), and non-parametric tests (Wilcoxon signed ranks test) assessed the change in severity of symptoms and quality of life before and after the BSP. The percentage of patients who would repeat the procedure and the median time to return to normal activities were also investigated.
The change in the Lund–Mackay score between preoperative and postoperative, thereby eliminating the variation among individuals and determining the intra-subject variation, was calculated. Additionally, differences among pairs of individuals using nonparametric analyses tested differences in medians. Differences were considered statistically significant if p<0.05.
The intra-class correlation coefficient was determined for the items of the SNOT-20 questionnaire using the Cronbach's alpha for consistency.
ResultsDuring the enrollment period, 18 patients were assessed for eligibility criteria and 13 were included, 62% men, aged 39.9±15.6 years. Five patients did not complete the evaluation and were excluded of the analysis.
Sinuplasty was performed in 24 sinuses of 13 patients (ten maxillar, four sphenoid, ten frontal sinuses). Only one of the 13 patients underwent a hybrid procedure consisting of balloon within the left frontal sinus surgery, followed by conventional maxillary bilateral, at the surgeon's discretion. It was considered that the balloon approach for the maxillary sinuses would not lead to good results with only the sinuplasty (uncinate process atelectasis). All other patients underwent BSP only. The technique for sinus catheterization was performed for all patients, and there was no difficulty or impossibility. Patients were reassessed at approximately 8.2±4.5 months after the procedure.
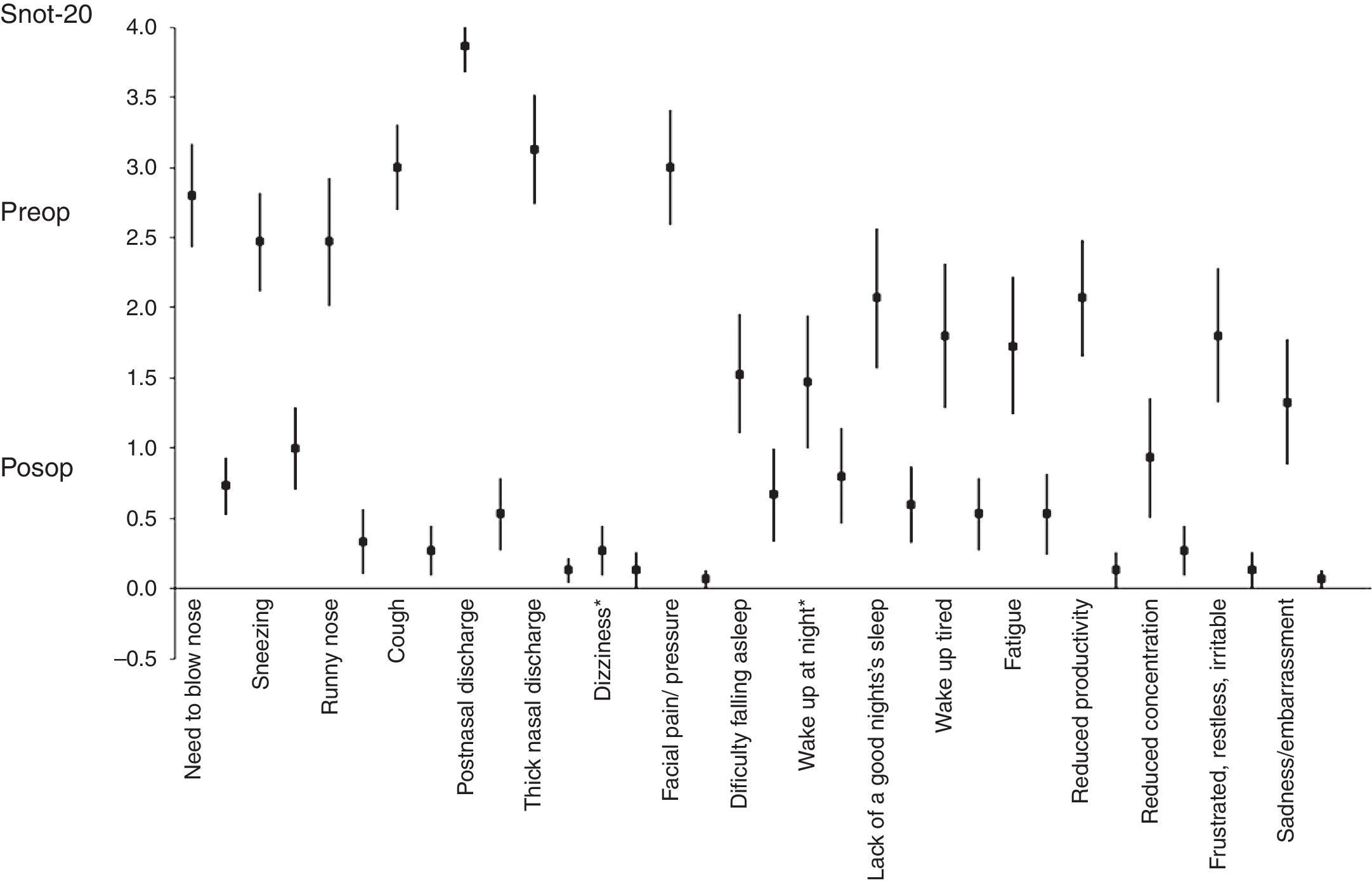
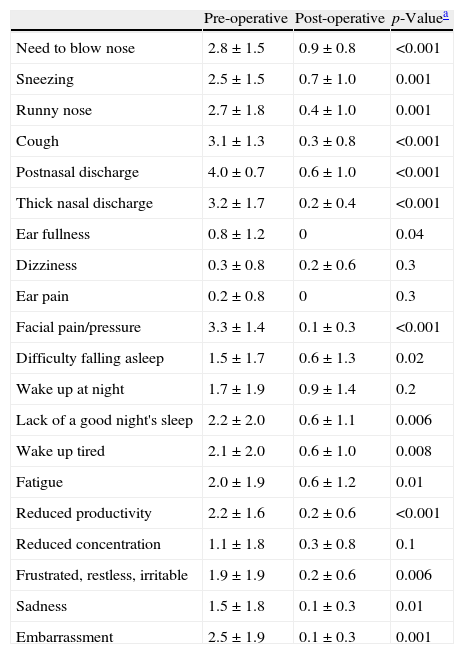
Table 1 demonstrates that there were marked differences in clinical signs at the pre- and postoperative assessment, verified through the SNOT-20, particularly cough, post-nasal drip, thick nasal discharge, pain over the sinuses, and reduction of daily life activities. The Cronbach coefficient for consistency of the items of the SNOT-20 questionnaire was 0.86 (95% CI: 0.73–0.94) in the preoperative and 0.88 (95% CI: 0.77–0.95) in the postoperative period (p<0.001).
Comparison of Sino-Nasal Outcome Questionnaire Test-20 [SNOT-20] scores per item (mean±DP) between pre- and postoperative period (n=13).
| Pre-operative | Post-operative | p-Valuea | |
| Need to blow nose | 2.8±1.5 | 0.9±0.8 | <0.001 |
| Sneezing | 2.5±1.5 | 0.7±1.0 | 0.001 |
| Runny nose | 2.7±1.8 | 0.4±1.0 | 0.001 |
| Cough | 3.1±1.3 | 0.3±0.8 | <0.001 |
| Postnasal discharge | 4.0±0.7 | 0.6±1.0 | <0.001 |
| Thick nasal discharge | 3.2±1.7 | 0.2±0.4 | <0.001 |
| Ear fullness | 0.8±1.2 | 0 | 0.04 |
| Dizziness | 0.3±0.8 | 0.2±0.6 | 0.3 |
| Ear pain | 0.2±0.8 | 0 | 0.3 |
| Facial pain/pressure | 3.3±1.4 | 0.1±0.3 | <0.001 |
| Difficulty falling asleep | 1.5±1.7 | 0.6±1.3 | 0.02 |
| Wake up at night | 1.7±1.9 | 0.9±1.4 | 0.2 |
| Lack of a good night's sleep | 2.2±2.0 | 0.6±1.1 | 0.006 |
| Wake up tired | 2.1±2.0 | 0.6±1.0 | 0.008 |
| Fatigue | 2.0±1.9 | 0.6±1.2 | 0.01 |
| Reduced productivity | 2.2±1.6 | 0.2±0.6 | <0.001 |
| Reduced concentration | 1.1±1.8 | 0.3±0.8 | 0.1 |
| Frustrated, restless, irritable | 1.9±1.9 | 0.2±0.6 | 0.006 |
| Sadness | 1.5±1.8 | 0.1±0.3 | 0.01 |
| Embarrassment | 2.5±1.9 | 0.1±0.3 | 0.001 |
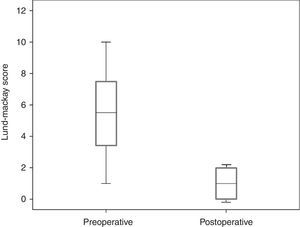
Fig. 1 shows a significant reduction in the overall score of clinical signs between the pre- and postoperative period.
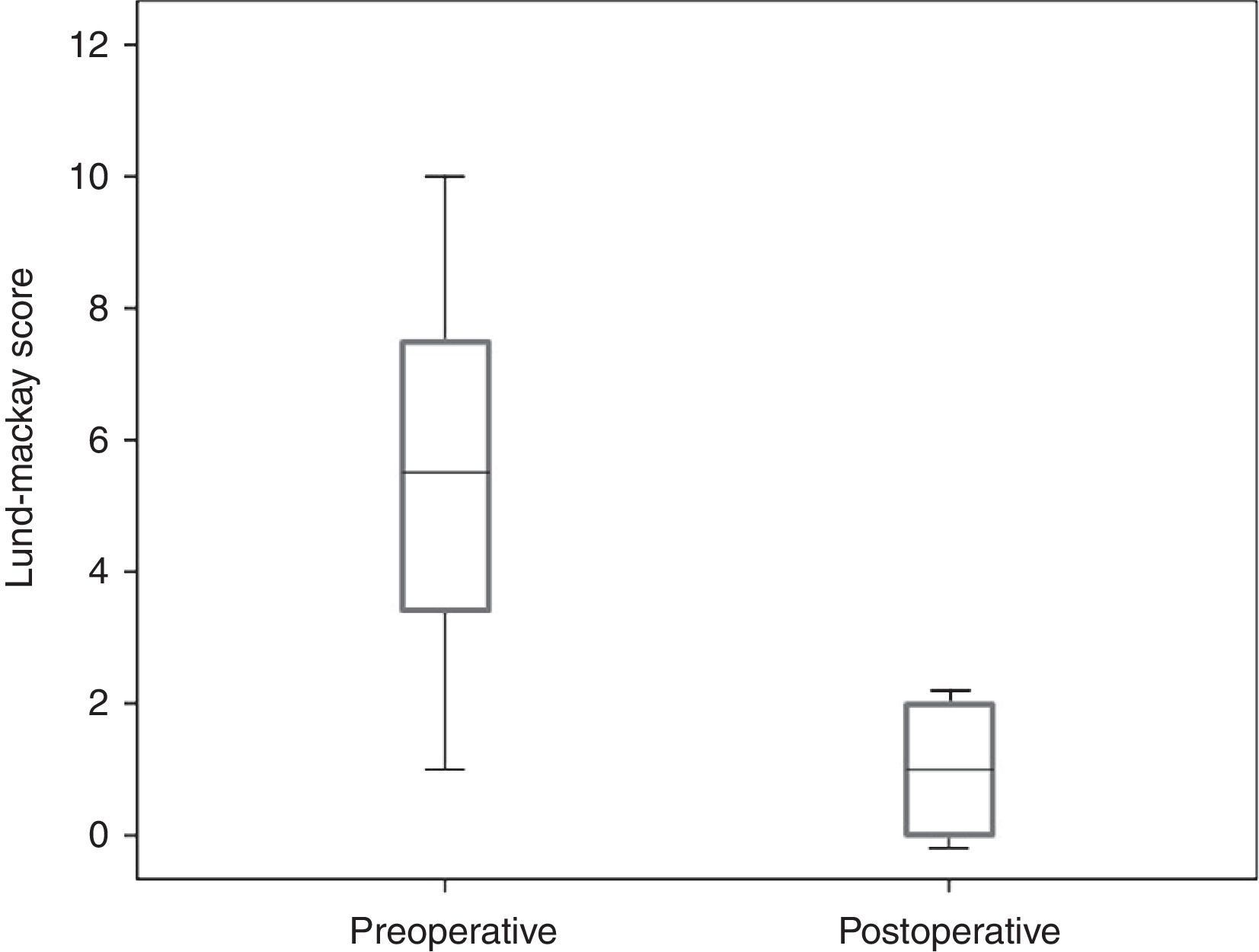
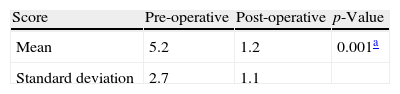
Table 2 shows a marked reduction in the tomographic score, on average 4.2±2.5 points. Besides the individual variation, there were significant differences in the scores, since the minimum and maximum scores ranged from 1 to 10 in the pre-operative period, and from 0 to 3 in the postoperative. There was high patency rate after the procedure (22 out of 24 catheterized sinuses). Fig. 2 shows a tomographic improvement in treated patients.
Comparison of Lund–McKay tomographic score between pre-operative and postoperative.
| Score | Pre-operative | Post-operative | p-Value |
| Mean | 5.2 | 1.2 | 0.001a |
| Standard deviation | 2.7 | 1.1 |
In the preoperative period, on average 1.9 sinuses per patient were affected; in the postoperative, there was a reduction to 0.4 per patient. The number of balloon catheterizations per patient ranged from one to four.
No patient had significant bleeding, CSF leak, orbital injury, or other complications. Surgical revision was not necessary in any patient. It was observed that all patients remained motivated and were willing to repeat the procedure, and took, on average, 7.0±2.8 days to return to their usual activities.
DiscussionThis study confirmed the safety and high success rate in ostial dilation of the procedure, which resulted in patency of the sinuses at the follow-up. There were no severe adverse events, such as CSF fistula, orbital injury, or major bleeding. This study confirmed the reduction of symptoms and the increase in quality of life in patients with chronic rhinosinusitis who underwent balloon catheterization.14,15
The effectiveness of sinuplasty had already been described5,10,14,15 and the present results confirmed the viability of this procedure in otolaryngology practice.5,14,15 The use of a standardized instrument, such as the SNOT-20 questionnaire, allowed to quantify the improvement on symptoms and quality of life14,15 after the procedure, and there were substantial benefits. Considering the patient's perspective, the results justify the therapeutic approach by balloon catheterization.
However, some considerations should be made regarding these patients, since they were selected in a reference center, according to the recommendations for sinuplasty (patients with chronic rhinosinusitis and with localized disease without polyposis or other complicating factors).13,15 Therefore, the present study evaluated a subset of patients with chronic rhinosinusitis refractory to clinical treatment, for whom sinuplasty was effective.
Radiological assessment of the sinuses by the Lund–Mackay score is strength of the study, since the balloon catheterization causes bone micro-fractures of the paranasal ostia and a CT scan can detect them.15
The rigid endoscopy was used as a complementary diagnostic exam to the physical exam, in the preoperative as well as the postoperative follow-up. This procedure allowed for the detection of potential complications, but due to the subjectivity in the interpretation of the results, it was not further analyzed in the before–after comparisons; it was used to assess the anatomy of the sinuses.
Specific indications for use of BSP in rhinosinusitis are not yet consensual, beyond those used in this study. They probably will emerge in subsequent studies, designed to establish further indications and their advantages. Statistical power was determined a posteriori to establish the beta error in the detection of associations. The differences between the pre- and post-operative Lund–Mackay score (5.2±2.7 vs. 1.2±1.1), in a sample of 13 patients, were large enough to confer over 90% of power and p<0.05, a statistically significant association. Finally, a broader analysis of the benefits of the procedure should take into account a cost-effectiveness analysis. A study comparing sinuplasty versus conventional FESS showed similar costs.8 However, they were not representative of the Brazilian patients and the public health care system.
ConclusionsIn conclusion, sinuplasty with balloon catheterization is effective in reducing symptoms and improving quality of life in selected patients with chronic rhinosinusitis. The results are beyond reported symptoms and confirm the benefit of BSP.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Abreu CB, Balsalobre L, Pascoto GR, Pozzobon M, Fuchs SC, Stamm AC. Effectiveness of balloon sinuplasty in patients with chronic rhinosinusitis without polyposis. Braz J Otorhinolaryngol. 2014;80:470–5.
Centro de Otorrinolaringologia e Fonoaudiologia de São Paulo – Complexo Hospitalar Edmundo Vasconcelos, São Paulo, SP, Brazil.



![Change in clinical signs of the Sino-Nasal Outcome Questionnaire Test-20 [SNOT-20] from pre- to post-operative period. For all clinical signs, the change from pre- to postoperative had p-value≤0.01, except for those marked with * (≥0.2). Change in clinical signs of the Sino-Nasal Outcome Questionnaire Test-20 [SNOT-20] from pre- to post-operative period. For all clinical signs, the change from pre- to postoperative had p-value≤0.01, except for those marked with * (≥0.2).](https://static.elsevier.es/multimedia/18088694/0000008000000006/v1_201411220154/S1808869414001116/v1_201411220154/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/7hLX2FbBoxC1192i158SI=)