Endoscopic ear surgery was introduced in 19901 and over the last two decades it has become popular. It has significantly changed surgical, anatomical and physiological concepts. Introduction of an endoscope has introduced the concept of minimally invasive ear surgery. Endoscopic middle ear surgery allows excellent visualization of medial wall of mesotympanum in addition to visualization of other hidden areas such as anterior epitympanic spaces, retro-tympanum and pro-tympanum.
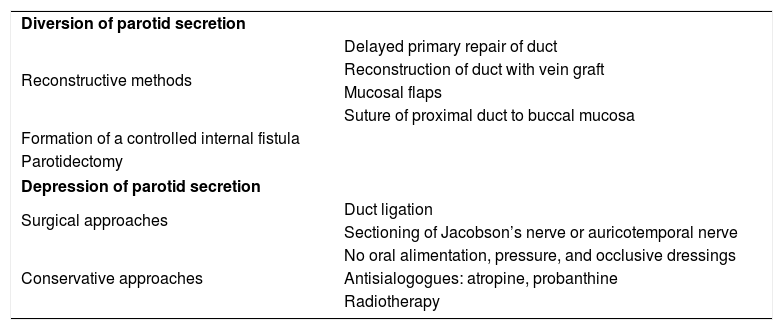
Parotid fistulae are rare and are caused by lacerations, parotid gland surgery, post- infections or neoplasms. Persistence of parotid fistulae is of great concern and causes embarrassment to the patient when eating. There is no uniform consensus regarding the treatment of choice for chronic parotid fistulae and different modalities of management have been proposed (Table 1).2 Tympanic neurectomy has been shown to be useful in persistent parotid fistulae.2 The wide angle view of the endoscope is useful for transcanal endoscopic tympanic neurectomy. The nerve divides on the promontory into an anterior branch that courses up towards the eustachian tube and a posterior branch that passes vertically, anterior to the round window niche. Also, apart from the anterior and posterior branch, the nerve can have a hypotympanic branch or more branches.3 These branches lie in a groove and are either covered by mucosa only or lie in a bony canal.2 Endoscopy has opened up new avenues to approach this nerve as the endoscope helps in precise identification of branches of the nerve.4
Classification of reported methods in literature for the management of parotid fistulae.
| Diversion of parotid secretion | |
| Reconstructive methods | Delayed primary repair of duct |
| Reconstruction of duct with vein graft | |
| Mucosal flaps | |
| Suture of proximal duct to buccal mucosa | |
| Formation of a controlled internal fistula | |
| Parotidectomy | |
| Depression of parotid secretion | |
| Surgical approaches | Duct ligation |
| Sectioning of Jacobson’s nerve or auricotemporal nerve | |
| Conservative approaches | No oral alimentation, pressure, and occlusive dressings |
| Antisialogogues: atropine, probanthine | |
| Radiotherapy | |
Before the advent of the endoscope, we have used the microscope for tympanic neurectomy for cases of persistent minor parotid gland fistulae. The aim of this study was to describe our experience with endoscopic tympanic neurectomy in selected cases.
Case reportWe identified three patients with persistent parotid fistulae who failed to respond to conservative management and underwent endoscopic tympanic neurectomy. The first patient was a 30-year-old male who had undergone incision and drainage for right parotid abscess at another hospital. and on day 8 post-drainage, he noticed clear watery discharge from the right cheek while eating/swallowing. This did not respond to conservative management and the patient presented to us 3 months after the incision and drainage procedure. The econd patient was a 12-year-old girl with history of watery discharge for 3–4 years from right infra-auricular region while eating food, with history of spontaneous rupture of a right parotid abscess following which she had developed right glandular fistula. The third patient was 34-year-old female operated for superficial parotidectomy elsewhere; following surgery on day 14 she developed watery discharge from right infra-auricular region while eating food.
Preoperatively in all patients a starch test was done where the suspected site of fistula was painted with betadine and allowed to dry (Fig. 1). Then sialagogue was given to the patient and the site was sprinkled with starch flour. At the end of the starch test, the site of salivary leak could be clearly seen (Fig. 2). Written and informed consent was taken from all patients regarding the procedure. General anesthesia was administered for 1 case (12-year-old girl) while the remaining 2 were operated under local anesthesia. After thorough counseling about the procedure the patients underwent tympanic neurectomy.
A 3mm 14cm endoscope was used to have better handling of instruments. One hand was engaged in holding the endoscope and other hand for instrumentation, hence micro instruments with incorporated suction ports give an advantage of avoiding the need for a separate suction. However, they have the disadvantage of making the instrument bulkier and suction ports are at right angle to the instrument so as the suction tubing doesn’t interfere while operating.
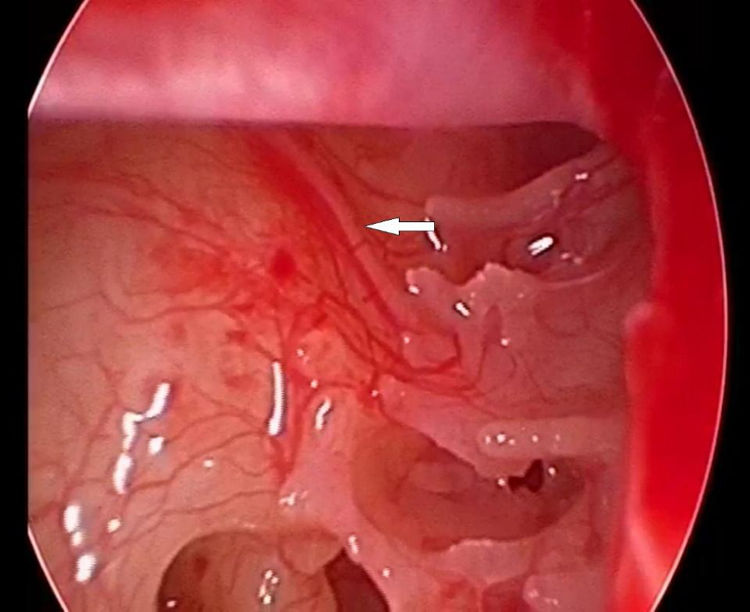
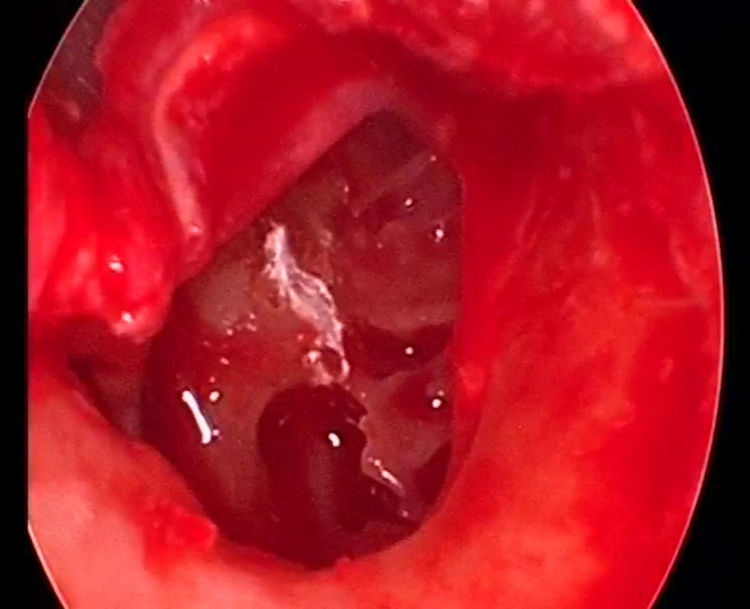
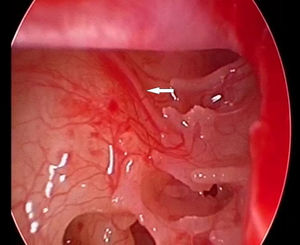
A Rosen endomeatal incision was created, and the tympanic nerve along with all its branches was identified on the promontory (Fig. 3), a right-angle pick employed to gently pick up the nerve. In 2 cases the nerve was submucosal while in 1 case it was in a bony canal. A segment of the nerve is cut with a sharp pick, removed and the cut ends were cauterized with bipolar cautery and drilled using a 0.6mm skeeter burr (Fig. 4) so as to prevent any re-innervation and thereby recurrence of symptoms. While drilling care was taken not to penetrate the promontory more than 1 to 2mm.
In 1 patient where the fistula developed post- incision and drainage of parotid abscess, in addition to the above procedure, 20% Trichloroacetic acid was applied to the fistulous tract.
Postoperatively patients were advised to follow a bland diet, utilize antibiotics and antisialogogue in form of tab glycopyrrolate 0.5mg for a week. Followup visits were done weekly for first two weeks and then at 1st, 2nd and 3rd month.
There were no adverse effects following the procedure and all patients reported subjective improvement in symptoms within 2 weeks; objectively the starch test was negative. There was successful cessation of flow from the parotid fistula with no recurrence or any complications on followup. Use ofhe endoscope helped in precise identification of the branches of Jacobson’s nerve and also helped to reduce the intraoperative time.
DiscussionJacobson’s nerve is a branch of the ninth cranial nerve and provides parasympathetic secretomotor preganglionic fibres to the parotid gland. It originates in the inferior salivatory nucleus in the medulla.2 It enters the floor of the middle ear and traverses the promontory and exists anteriorly as the lesser superficial petrosal nerve. It synapses at the otic ganglion and postganglionic fibers then enter the parotid gland via the auriculotemporal nerve.5 Tympanic neurectomy eliminates the parasympathetic activity in the parotid gland and is one form of treatment in cases of persistent parotid fistulae. It is also useful in cases of Frey’s syndrome and excessive drooling of saliva.6 It has also been tried in cases of parotid duct stenosis, salivary duct dilation (sialectasis), chronic intractable otalgia of glossopharyngeal origin (not responding to conservative line of management).7 We have limited experience regarding these.
Parotid fistula is most commonly a posttraumatic situation and can be either intraductal or intraglandular. Glandular fistula can respond well to conservative treatment while ductal fistula is less likely to close spontaneously.8 Conservative approaches in the form of antibiotics and anticholinergic drugs are useful as they decrease the production of saliva. Fistulae which fail to response to conservative line of management should be managed surgically. Low dose radiotherapy9 and excision of the fistulous tract with ligation of the parotid duct has been advocated by some authorities.10 Tympanic neurectomy is an excellent treatment modality and when done endoscopically, it is minimally invasive, helps in excellent visualization and delineation of the nerve and reduces intra-operative time. In all our cases there was complete relief of symptoms with successful closure of fistula over a period of two weeks and negative starch test, which was done at end of 1 month. In our series tympanic neurectomy was successful in closure of both ductal and glandular fistulae. Sometimes the effect of tympanic neurectomy can be transient as parasympathetic fibers which reach the otic ganglion via the geniculate ganglion or by anastomoses between the chorda tympani and the otic ganglion, may not be affected by tympanic neurectomy. But as the major stimulus comes from Jacobson’s nerve, the failure rate of the procedure is minimal.2 Hence, whether the effects of tympanic neurectomy are transient or permanent appear to be less significant in case of parotid fistula as the suppression of activity is sufficiently long to allow for healing of the fistulous tract and relief of symptoms.
ConclusionEndoscopic tympanic neurectomy is minimally invasive, cost effective with good therapeutic outcome, and it can be done as an outpatient procedure. Tympanic neurectomy has been an established treatment modality for persistent parotid fistulae in the past but recurrences have been seen following the procedure. Though the microscope has been used for tympanic neurectomy in the past, endoscopy offers excellent visualization of middle ear anatomy and allows precise identification of the nerve. The combination of two established techniques – tympanic neurectomy and the use of an endoscope in ear surgery – shows the advantages of associating the two methods in the correction of persistent parotid fistulae and thus improving the outcomes.
The most important point to highlight here is that the segment of the Jacobson’s nerve must be excised, and the cut ends must be cauterized or drilled to prevent any reinnervation and recurrences.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.