Tracheotomy is one of the most frequent surgical procedures performed in critically ill patients hospitalized at intensive care units. The ideal timing for a tracheotomy is still controversial, despite decades of experience.
ObjectiveTo determine the impact of performing early tracheotomies in critically ill patients on duration of mechanical ventilation, intensive care unit stay, overall hospital stay, morbidity, and mortality.
MethodsRetrospective and observational study of cases subjected to elective tracheotomy at one of the intensive care units of this hospital during five consecutive years. The patients were stratified into two groups: early tracheotomy group (tracheotomy performed from day one up to and including day seven of mechanical ventilation) and late tracheotomy group (tracheotomy performed after day seven). The outcomes of the groups were compared.
ResultsIn the early tracheotomy group, there was a statistically significant reduction in duration of mechanical ventilation (6 days vs. 19 days; p<0.001), duration of intensive care unit stay (10 days vs. 28 days; p=0.001), and incidence of ventilator-associated pneumonia (1 case vs. 44 cases; p=0.001).
ConclusionEarly tracheotomy has a significant positive impact on critically ill patients hospitalized at this intensive care unit. These results support the tendency to balance the risk-benefit analysis in favor of early tracheotomy.
A traqueotomia é um dos procedimentos cirúrgicos mais frequentes em doentes críticos internados em unidades de terapia intensiva. O seu timing ideal é ainda, apesar de décadas de experiência, uma questão controversa.
ObjetivosDeterminar o impacto da realização de traqueotomias precoces em doentes críticos na duração da ventilação mecânica, do internamento na unidade de terapia intensiva, do internamento hospitalar, e mortalidade e morbidade.
MétodoEstudo observacional retrospectivo dos casos submetidos à traqueotomia eletiva em uma das unidades de terapia intensiva do nosso hospital durante 5 anos consecutivos. Os doentes foram divididos em dois grupos, tendo sido submetidos a traqueotomias precoces (até o 7° dia de ventilação mecânica, inclusive) ou tardias (após o 7° dia de ventilação mecânica), e os resultados foram comparados.
ResultadosNos doentes submetidos a uma traqueotomia precoce verificou-se uma redução estatisticamente significativa na duração da ventilação mecânica (6 dias vs. 19 dias; p<0,001), na duração do internamento na unidade terapia intensiva (10 dias vs. 28 dias; p=0,001) e na incidência de pneumonia associada ao ventilador (1 caso vs. 44 casos; p=0,001).
ConclusãoA traqueotomia precoce tem um impacto positivo estatisticamente significativo nos doentes críticos. Os resultados suportam a tendência de equilibrar o risco-benefício em favor da traqueotomia precoce.
Tracheotomy is one of the most frequently performed surgical procedures in critically ill patients admitted to intensive care units (ICUs).1 The advantages of tracheotomy regarding prolonged orotracheal intubation have been described, such as the reduction of laryngeal lesions, greater ease in ventilator weaning by decreasing airway resistance, decreased need for deep sedation, better pulmonary hygiene, increased patient mobility, improved communication and oral nutrition, and subjective improvement in patient satisfaction.2–4 In addition to these, some studies have shown an association between early tracheotomy and shorter duration of mechanical ventilation and ICU stay, with a decrease in ventilator-associated pneumonia (VAP).4–7 However, tracheotomy carries some risk of complications, including bleeding, infection of the stoma, pneumothorax or pneumomediastinum, injury to vascular or nerve structures, tracheal stenosis, tracheoesophageal fistula, or even death.5,7,8 Thus, the decision to perform a tracheotomy and when the procedure should be conducted must be based on a balance between risks and benefits, while also considering the costs and an efficient management of resources.2 Despite decades of experience, the optimal timing of tracheotomy is still a contentious issue, for both otorhinolaryngologists and intensivists, and the impact of early tracheotomy on the results of patients admitted to ICU is still unclear7,9,10 (and even the definition of early and late tracheotomy is a controversial subject).7,11 The practices have been heterogeneous among the various centers.7,9,10 This issue was an incentive to perform a retrospective study in critically ill patients admitted to a polyvalent ICU at the present hospital, in order to analyze the impact of early elective tracheotomy in outcomes of patients admitted to the ICU. The aim was to test the hypothesis that early tracheotomy, compared with late tracheotomy, can reduce the duration of mechanical ventilation, length of stay in the ICU and in the hospital, VAP incidence, and mortality in critically ill patients.
The main objectives of the study were to compare critical patients undergoing early tracheotomy and those undergoing late tracheotomy, in relation to the duration of mechanical ventilation, length of stay in ICU and in hospital, incidence of VAP, and mortality. Secondary objectives included evaluating the incidence of complications of tracheotomy and whether there were significant differences between the two groups regarding age, gender, ICU admission diagnosis, comorbidities, and complications.
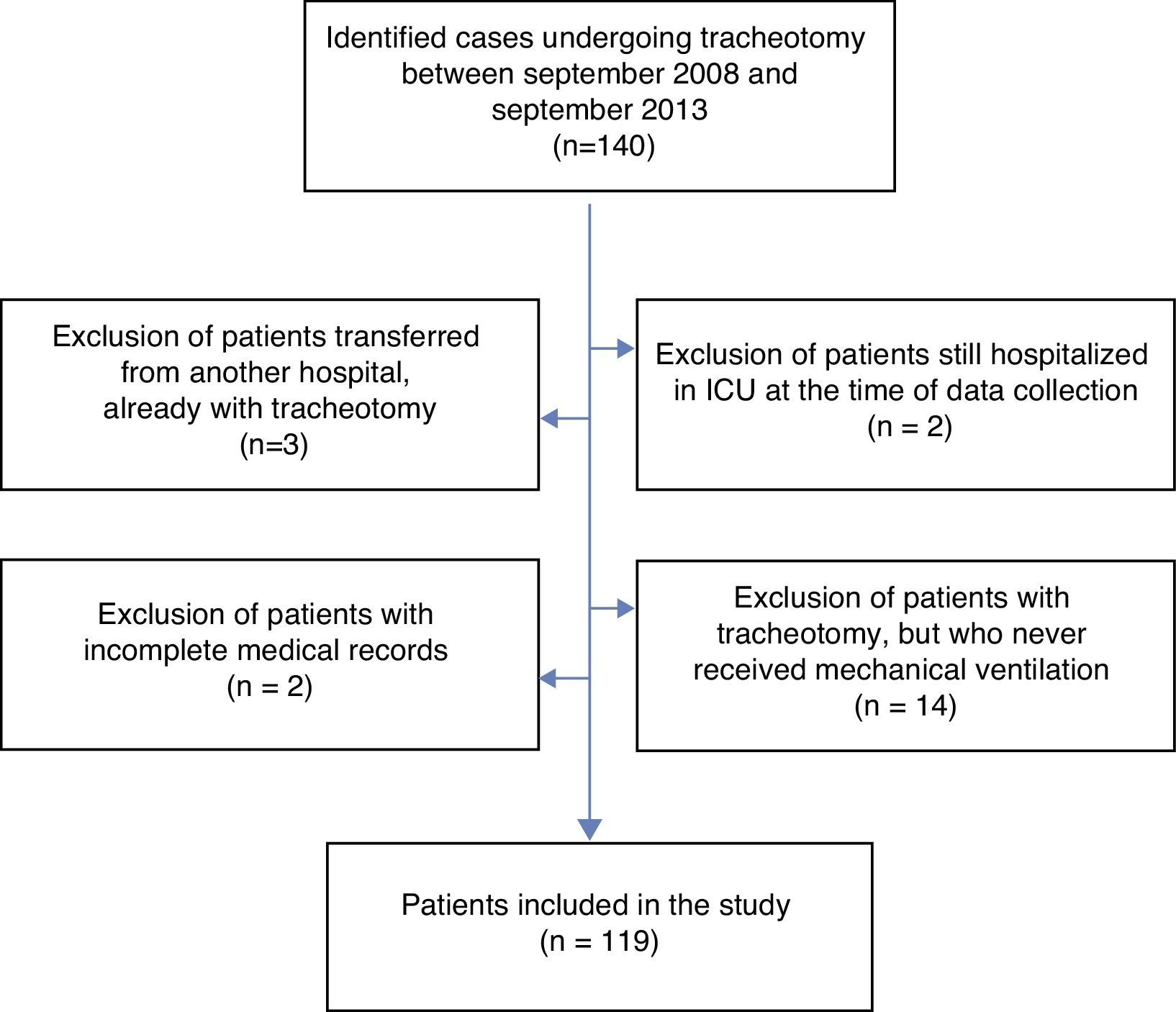
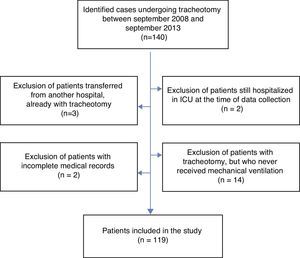
Materials and methodsStudy design and eligibilityA retrospective observational study of patients who underwent elective tracheotomy in one of the ICUs at this hospital, the Emergency Medical Unit, consecutively between September, 2008 and September, 2013, was performed. The Emergency Medical Unit is a multipurpose ICU, which receives critically ill patients of various types, including medical, surgical, neurological, and traumatic pathologies. In total, 140 patients who underwent tracheotomy during this period were identified (Fig. 1). Of these, the following were excluded: two because they were still hospitalized in ICU at the time of the study; three others because they had been transferred from another hospital ICU, with a pre-existing tracheotomy; 14 because, although tracheotomized, they never underwent mechanical ventilation (vocal cord paralysis, laryngeal fracture, mandibular fracture, and cervical abscess); and two due to incomplete medical records. Thus, a total of 119 patients were included in this study.
Patients and procedureThe 119 patients were divided into two groups, depending on the timing of tracheotomy. In the early tracheotomy group, patients who underwent tracheotomy between days one and seven (included) of mechanical ventilation were included; in the late tracheotomy group, patients who underwent tracheotomy after the seventh day of mechanical ventilation were included. Early and late tracheotomy were defined as such, since most recent studies have adopted this definition,4–7 and some authors indicate that there are signals of endolaryngeal lesions after seven days of orotracheal intubation.2
All patients were over 18 years old. All tracheotomies were elective and performed by otolaryngologists using the traditional surgical technique, whether at the bedside (ICU) or in the operating room. In the ICU, the tracheotomies were performed under unconscious sedation, and in the operating room under general anesthesia. The technique consisted of a horizontal skin incision, the infra-isthmic approach of trachea, with opening of the trachea in “lying down H.” In most patients, Shiley cuffed cannulas (#6 or #8, in women and men, respectively) were placed, unless the patient's anatomy necessitated the use of another type of cannula.
Collection of dataData were collected by the authors and organized with Microsoft Excel® for Mac 2011. Data on demographics; cause of ICU admission; comorbidities; date of admission and of hospital and ICU discharge; date of orotracheal intubation; date of starting and ending of mechanical ventilation; incidence of VAP (defined as a visible pulmonary infiltrate on a chest radiograph with fever, leukocytosis, and purulent tracheobronchial secretions with positive cultures, starting at least 48h after intubation);12 date and place of tracheotomy; and complications of tracheotomy and mortality were collected.
Due to some characteristics inherent to the organization of the Portuguese Health Service, 48 patients (40.3%) were transferred, after discharge from ICU, to other national hospitals in their area of residence (or international hospitals, in the case of foreign patients), or to continued care units. For this reason, hospital discharge dates were only obtained for the remaining 71 (59.7%) patients, who were transferred to other inpatient services of the present hospital.
Data analysisThe duration of mechanical ventilation and of ICU and hospital stay was then calculated. Mechanical ventilation was measured (in days) from the connection of the orotracheal tube to the ventilator until the complete disconnection, or patient death; duration of ICU stay was measured from admission until discharge from the ICU, or patient death; and duration of hospital stay was measured from admission until hospital discharge, or patient death. The timing of tracheotomy was measured in days from the beginning of mechanical ventilation until the day of tracheotomy. The time elapsed between the tracheotomy and the discharge from ICU was also calculated.
The statistical analysis was performed with SPSS 20.0 for Mac. To describe categorical variables, frequencies and proportions were used. For continuous variables, medians and interquartile range were used as measures of central tendency and dispersion, respectively, as they had skewed distribution. In the analysis of association between variables, the following nonparametric tests were performed: Mann–Whitney U, chi-squared, and Spearman's correlation. A value of p<0.05 was considered statistically significant.
ResultsCharacteristics of patientsOf the 119 patients included in the study, 18 (15.1%) underwent early tracheotomy (ET), i.e. up to seven days of mechanical ventilation; the remaining 101 (84.9%) underwent late tracheotomy (LT), i.e. after the seventh day.
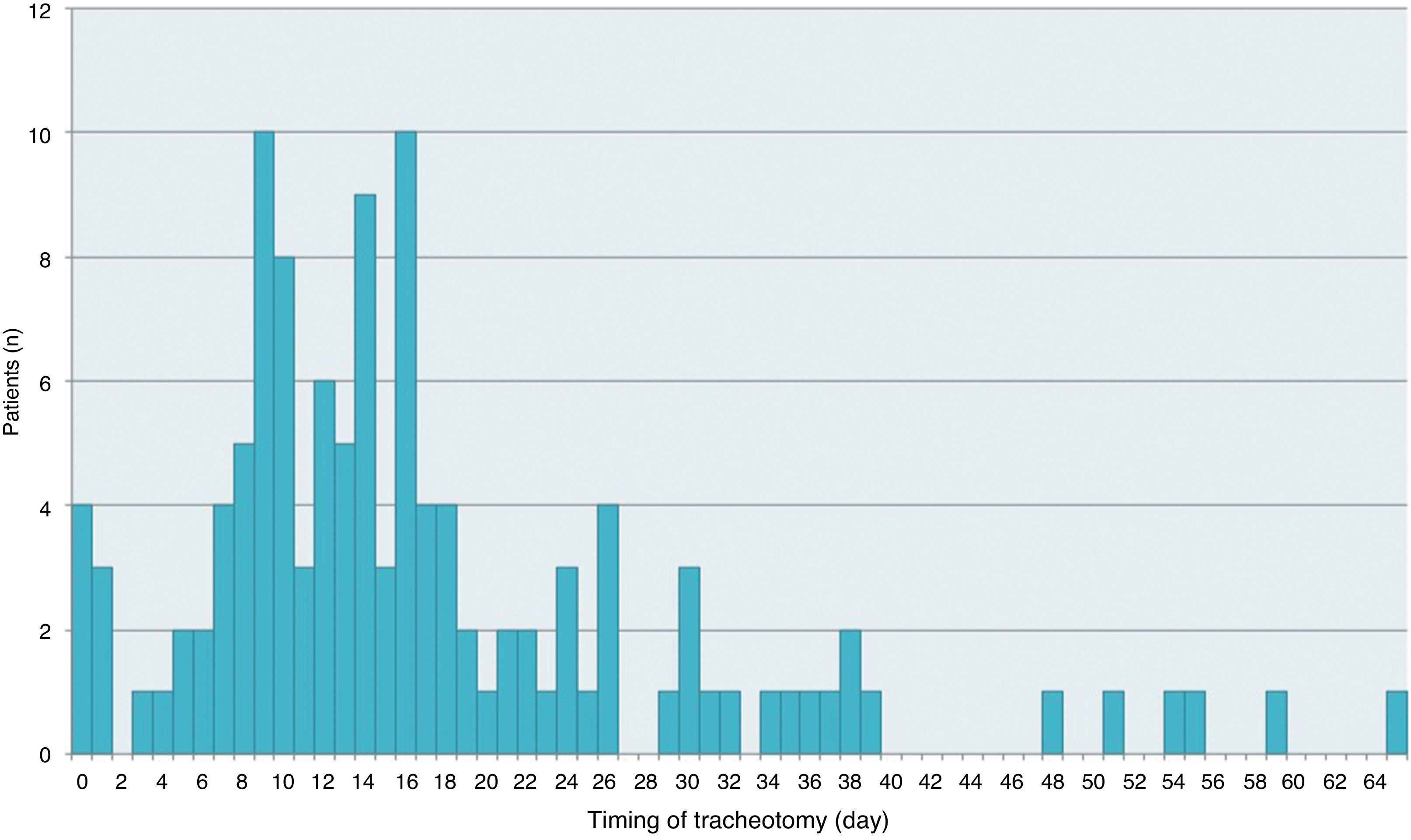
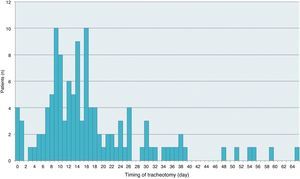
The distribution of patients by timing of the tracheotomy is depicted in Fig. 2.
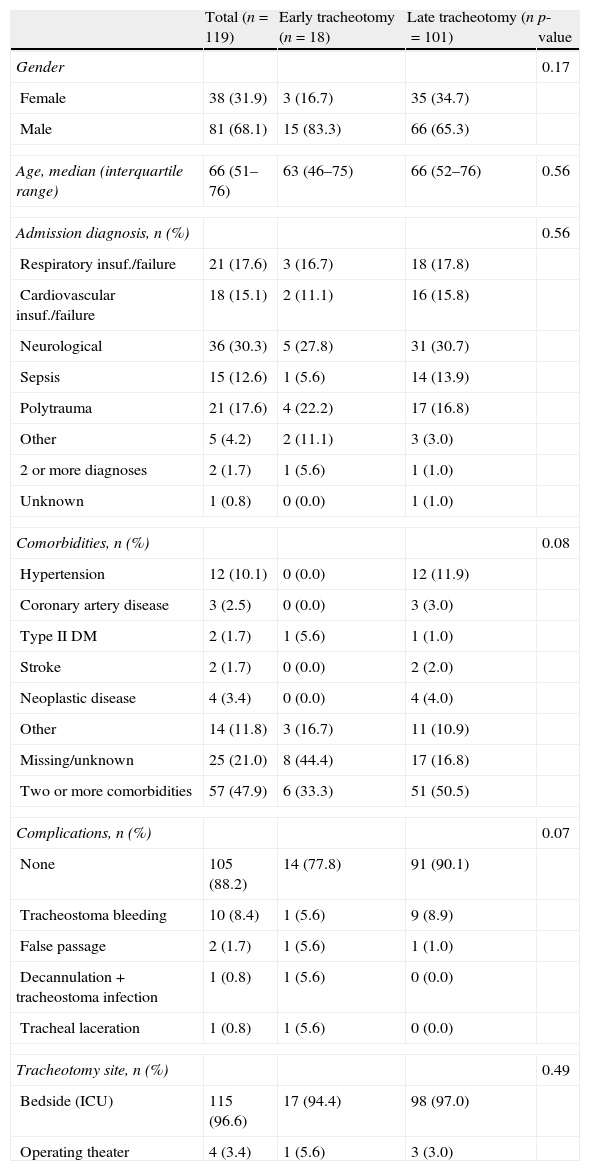
ET and LT groups did not differ significantly by gender (p=0.17), age (p=0.56), admission diagnosis (p=0.56), or comorbidities (p=0.08) (Table 1).
Characteristics of patients, complications, and site of the tracheotomy.
| Total (n=119) | Early tracheotomy (n=18) | Late tracheotomy (n=101) | p-value | |
| Gender | 0.17 | |||
| Female | 38 (31.9) | 3 (16.7) | 35 (34.7) | |
| Male | 81 (68.1) | 15 (83.3) | 66 (65.3) | |
| Age, median (interquartile range) | 66 (51–76) | 63 (46–75) | 66 (52–76) | 0.56 |
| Admission diagnosis, n (%) | 0.56 | |||
| Respiratory insuf./failure | 21 (17.6) | 3 (16.7) | 18 (17.8) | |
| Cardiovascular insuf./failure | 18 (15.1) | 2 (11.1) | 16 (15.8) | |
| Neurological | 36 (30.3) | 5 (27.8) | 31 (30.7) | |
| Sepsis | 15 (12.6) | 1 (5.6) | 14 (13.9) | |
| Polytrauma | 21 (17.6) | 4 (22.2) | 17 (16.8) | |
| Other | 5 (4.2) | 2 (11.1) | 3 (3.0) | |
| 2 or more diagnoses | 2 (1.7) | 1 (5.6) | 1 (1.0) | |
| Unknown | 1 (0.8) | 0 (0.0) | 1 (1.0) | |
| Comorbidities, n (%) | 0.08 | |||
| Hypertension | 12 (10.1) | 0 (0.0) | 12 (11.9) | |
| Coronary artery disease | 3 (2.5) | 0 (0.0) | 3 (3.0) | |
| Type II DM | 2 (1.7) | 1 (5.6) | 1 (1.0) | |
| Stroke | 2 (1.7) | 0 (0.0) | 2 (2.0) | |
| Neoplastic disease | 4 (3.4) | 0 (0.0) | 4 (4.0) | |
| Other | 14 (11.8) | 3 (16.7) | 11 (10.9) | |
| Missing/unknown | 25 (21.0) | 8 (44.4) | 17 (16.8) | |
| Two or more comorbidities | 57 (47.9) | 6 (33.3) | 51 (50.5) | |
| Complications, n (%) | 0.07 | |||
| None | 105 (88.2) | 14 (77.8) | 91 (90.1) | |
| Tracheostoma bleeding | 10 (8.4) | 1 (5.6) | 9 (8.9) | |
| False passage | 2 (1.7) | 1 (5.6) | 1 (1.0) | |
| Decannulation + tracheostoma infection | 1 (0.8) | 1 (5.6) | 0 (0.0) | |
| Tracheal laceration | 1 (0.8) | 1 (5.6) | 0 (0.0) | |
| Tracheotomy site, n (%) | 0.49 | |||
| Bedside (ICU) | 115 (96.6) | 17 (94.4) | 98 (97.0) | |
| Operating theater | 4 (3.4) | 1 (5.6) | 3 (3.0) | |
DM, diabetes mellitus; ICU, intensive care unit.
The median age was 66 years (interquartile range 51–76). Male gender was prevalent (68.1%), both in the ET group (83.3%) and the LT (65.3%) group. The most frequent ICU admission diagnosis was neurological disorder (30.3%), both in the ET group (27.8%) and the LT (30.7%) group. Most (47.9%) patients had two or more comorbidities, and the most commonly observed were hypertension with dyslipidemia and/or diabetes mellitus type II. In all patients, 21.0% had no comorbidities or they were unknown (44.4% and 16.8% of patients in the LT and ET groups, respectively).
Site of tracheotomy and complicationsThe groups also did not differ significantly regarding the tracheotomy site (p=0.49) (Table 1). Most tracheotomies were performed at the ICU bedside (96.6% ICU vs. 3.4% operating theater). The tracheotomies performed in the operating room were conducted in patients undergoing other surgeries, in whom there was a need for tracheotomy; both procedures were performed during the same operation. Otherwise, the tracheotomy would have also been performed at the bedside.
The occurrence of early complications (up to one month after tracheotomy) was observed in only 14 patients (11.8%), and the most common complication was tracheostoma bleeding (8.4%); other complications were the emergence of a false passage (1.7%) necessitating a tracheotomy revision; decannulation and tracheostoma infection, which occurred in the same patient (0.8%), and laceration of the posterior wall of the trachea in another patient (0.8%). Most bleedings were of low output and self-limited, occurring 24–48h after the procedure; some had to be controlled with compression packing using a hemostatic agent. There were no statistically significant differences between the two groups regarding complications (ET 22.2% vs. LT 22.9%; p=0.07).
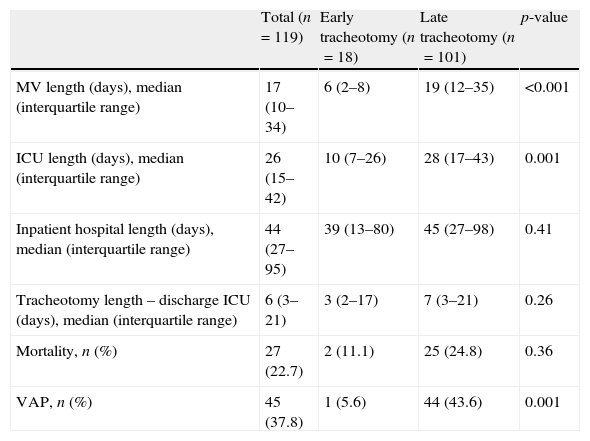
Duration of mechanical ventilation, ICU stay, and hospital stayTable 2 shows the main results in accordance with the timing of tracheotomy. In all patients, the median duration of mechanical ventilation was 17 days (interquartile range 10–34) and, for the ICU stay, 26 days (interquartile range 15–42). However, ET was associated with a significantly shorter duration of mechanical ventilation (6 vs. 19 days, p<0.001) and a shorter duration of ICU stay, also statistically significant (10 vs. 28 days, p=0.001).
Main results.
| Total (n=119) | Early tracheotomy (n=18) | Late tracheotomy (n=101) | p-value | |
| MV length (days), median (interquartile range) | 17 (10–34) | 6 (2–8) | 19 (12–35) | <0.001 |
| ICU length (days), median (interquartile range) | 26 (15–42) | 10 (7–26) | 28 (17–43) | 0.001 |
| Inpatient hospital length (days), median (interquartile range) | 44 (27–95) | 39 (13–80) | 45 (27–98) | 0.41 |
| Tracheotomy length – discharge ICU (days), median (interquartile range) | 6 (3–21) | 3 (2–17) | 7 (3–21) | 0.26 |
| Mortality, n (%) | 27 (22.7) | 2 (11.1) | 25 (24.8) | 0.36 |
| VAP, n (%) | 45 (37.8) | 1 (5.6) | 44 (43.6) | 0.001 |
MV, mechanical ventilation; ICU, intensive care unit; VAP, ventilator-associated pneumonia.
As explained in the methodology of this study, the authors had access only to dates of hospital discharge for 71 patients (59.7%). In these patients, the median duration of hospitalization was 44 days (interquartile range 27–95). A shorter duration of hospitalization in the ET group (39 days vs. 45 days) was found, although with no statistical significance (p=0.41).
The time elapsed between tracheotomy and discharge from ICU was shorter in ET group (3 days vs. 7 days), although not statistically significant (p=0.26).
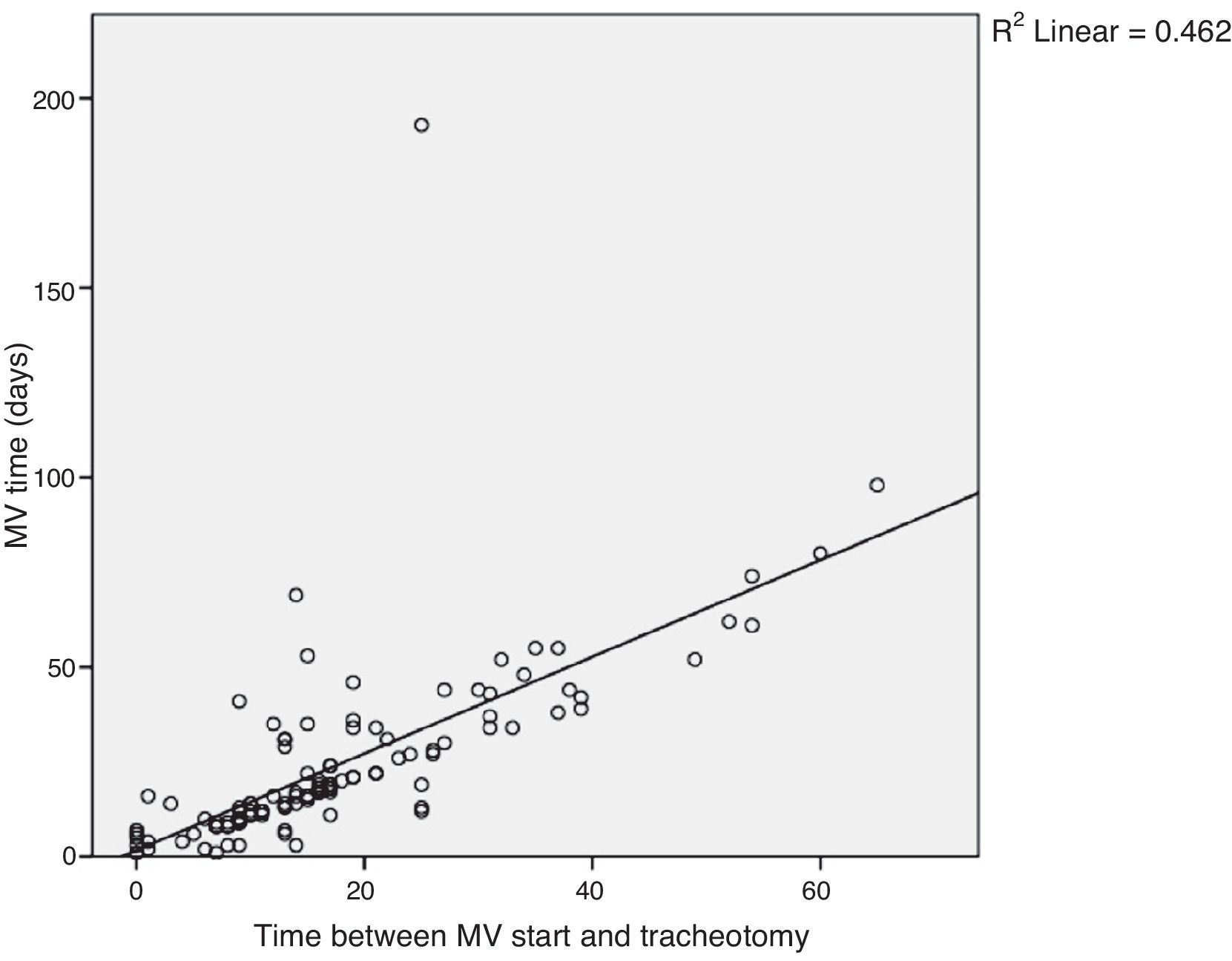
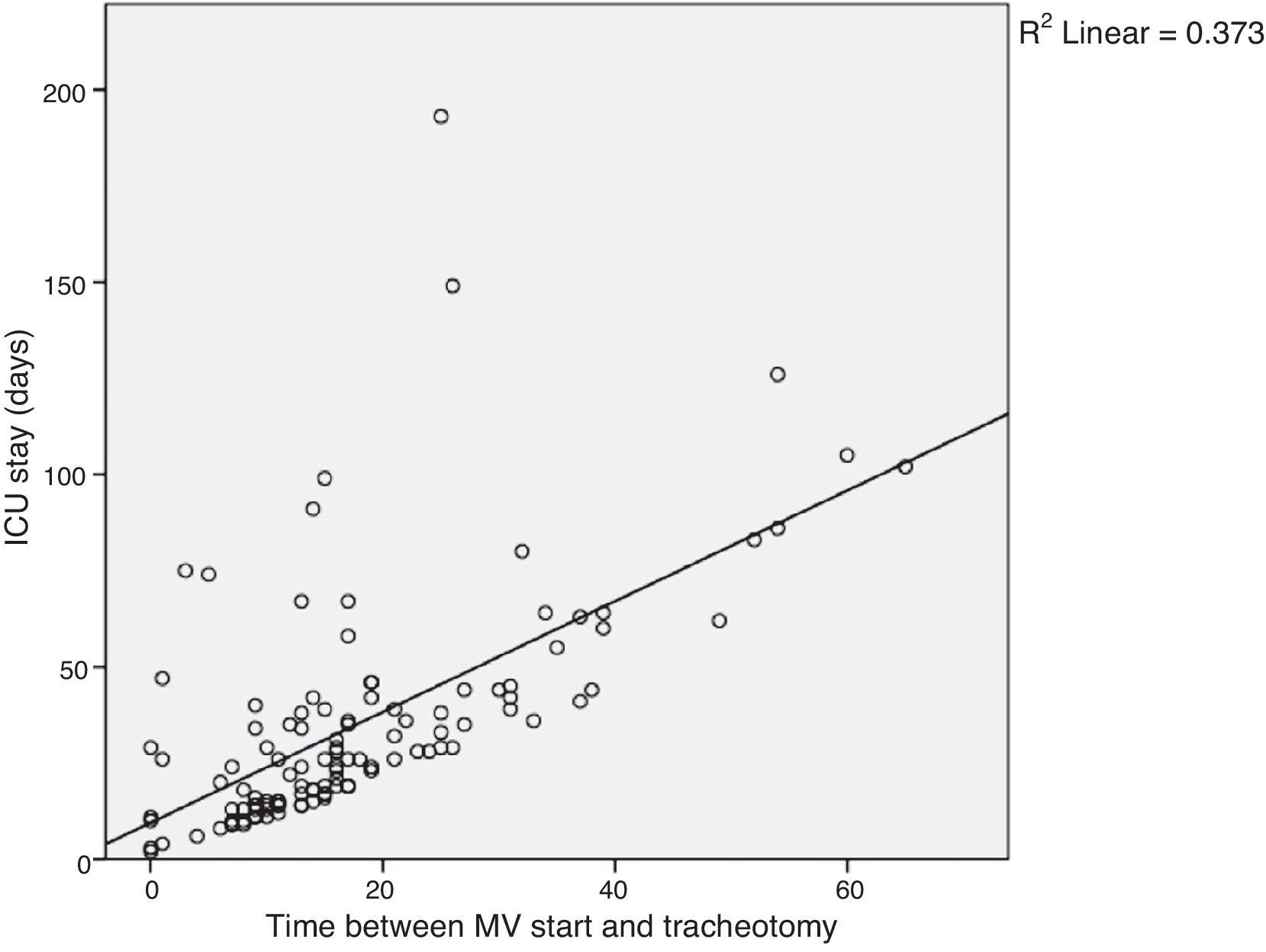
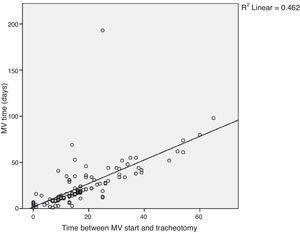
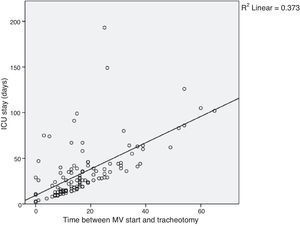
Figs. 3 and 4 show the distribution of patients by timing of tracheotomy (time elapsed between the onset of mechanical ventilation and the tracheotomy procedure) and duration of mechanical ventilation or ICU stay, respectively. A correlation between the duration of mechanical ventilation and timing of tracheotomy (Spearman's correlation=0.68, corresponding to a R2=0.46) and between the duration of ICU stay and the timing of tracheotomy (Spearman's correlation=0.61; R2=0.37) was found.
VAP occurred in 45 patients (37.8%). Only one patient in ET group developed VAP. The difference between the two groups was statistically significant (p=0.001) (Table 2).
The overall mortality was 22.7%, with no statistically significant differences between groups (p=0.36) (Table 2), although with a tendency to lower mortality in ET group (11.1% vs. 24.8%). None of the deaths were attributed to the tracheotomy procedure.
DiscussionThis study demonstrates that the practice of early tracheotomy in critically ill ICU patients is associated with a statistically significant reduction in duration of mechanical ventilation, duration of ICU stay, and incidence of VAP. This finding is in agreement with many studies that have been conducted in other centers.4–7 This suggests that ET, as well as having a positive impact on patient morbidity (lower incidence of VAP), has the potential to positively influence the management of resources associated with the hospitalization of patients in an ICU, by decreasing the ICU stay.
In addition, a correlation between the duration of mechanical ventilation and timing of tracheotomy (Fig. 3), and between the length of ICU stay and the timing of the tracheotomy (Fig. 4) was found, which indicates that the timing of the tracheotomy explains 46% of the days of mechanical ventilation (R2=0.46) and 37% of the days of ICU stay (R2=0.37). Therefore, considering that continuous variables were compared, it can be concluded that the sooner the patient is subjected to tracheotomy, the shorter the duration of mechanical ventilation and of ICU stay.
Mortality was not significantly lower in ET group, although there was a trend toward reduced mortality in this group compared to the LT group (11.1% vs. 24.8%). This finding is consistent with most studies in the literature.4–7,13
Considering that 71 patients remained hospitalized after discharge from the ICU, the duration of the total hospitalization was not significantly reduced in ET group (although with a tendency toward reduction), as has been demonstrated in many studies, and in accordance with the shorter duration of ICU stay of this group.
After tracheotomy, discharge from the ICU occurred rapidly (ET 3 days vs. LT 7 days) and in a similar period in both groups (p=0.26), suggesting that this procedure was a key factor in facilitating the discontinuation of invasive ventilation support, decreasing the level of intensive care, and in facilitating ICU discharge, as has been suggested in other studies.4–6,11
Gender, age, admission diagnosis, and comorbidities were similar in both groups.
Elective tracheotomy by traditional surgical technique is a safe procedure; in the present study, a low incidence of early complications was found (11.8%), mostly unimportant (self-limited bleeding) and without serious consequences for the patient. These early complications were also similar in both groups.
Most procedures were performed in the ICU, and this contributed to a reduction in the cost and time associated with surgery, avoiding unnecessary costs of room occupancy in the operating theater and of movement of ventilated patients, with better patient comfort. Likewise, no differences between groups were found resulting from the site of the procedure.
This study has the advantage of demonstrating benefits of ET on a population of unselected critically ill patients, while most previous studies have focused on more specific patient subgroups: medical pathology,14 traumatic condition,6 and the elderly,5 among others.
Due to its retrospective design, this study has some limitations. Although the data analysis for age, admission diagnosis, and comorbidities of the two groups did not show statistically significant differences, a selection bias of patients who underwent ET, compared to LT, probably occurred; this bias would be eliminated with a prospective randomized study. The timing of tracheotomy was chosen by the physician responsible for the patient; certainly, an individual selection process for the realization of ET existed, a process that was not documented in the medical records, such as when the decision to perform tracheotomy was made, and the exact reason for it.
In this study, most patients underwent LT (84.9%). It is believed that this option occurred for several reasons, including an expected improvement of the patient that did not occur; instability of the patient for an early tracheotomy; and difficult weaning from invasive ventilation. Various attempts have been made to develop a formula for predicting the likelihood of a patient requiring prolonged ventilation; such a formula would allow a better selection of patients for performing ET. To date, no validated system has been found to forecast the need for prolonged ventilation in the intensive care general population, and therefore the selection of patients for tracheotomy remains a subjective decision. However, the favorable results of this trial and of studies conducted in other centers suggest a benefit in early performance of tracheotomy (up to day seven of mechanical ventilation).
ConclusionsThis study suggests that ET (up to day seven of mechanical ventilation) has a statistically significant positive impact in critically ill ICU patients, by reducing the duration of mechanical ventilation, ICU stay, and incidence of VAP, and likely reducing mortality and length of hospital stay. The study demonstrated that the sooner the patient is subjected to tracheotomy, the shorter the duration of mechanical ventilation and the time of ICU stay. These results support the tendency to balance the risk-benefit analysis in favor of early tracheotomy.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank Dr. Manuel José Magalhães for his help with the statistical analysis.
Please cite this article as: Correia IA, Sousa V, Pinto LM, Barros E. Impact of early elective tracheotomy in critically ill patients. Braz J Otorhinolaryngol. 2014;80:428–34.