Lemierre's syndrome (LS) is a rare and serious pharyngotonsillitis complication that usually occurs in adolescents and young adults caused by anaerobic bacteria, more specifically attributed to Fusobacterium necrophorum. First described in the early twentieth century, it was in 1936 that the French microbiologist, Dr. André Lemierre, outlined the characteristics of the disease.1
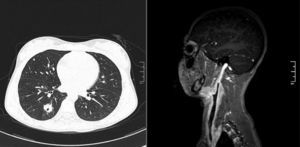
Case reportA female patient (K.C.O.), 12 years old, previously healthy, presented with sore throat and fever for seven days. She was diagnosed in another center with pharyngotonsillitis and received intramuscular Benzathine benzylpenicillin, evolving with pain improvement, but with the onset of persistent high temperature and bulging in the right anterior cervical region for three days. Hyperemia was observed in the oropharynx and cervical bulging on topography of the right sternocleidomastoid muscle, painful on palpation. Contrast tomography and angiography show right peritonsillar inflammation, thrombosis of right internal jugular vein (IJV), and pulmonary nodules consistent with microabscesses (Fig. 1). Initially, the diagnosis of LS was not considered, and intravenous antibiotic therapy was started with amoxicillin and clavulanate at a dose 90mg/kg/day, and anticoagulation with enoxaparin and warfarin, with gradual clinical improvement. After three days, with the final diagnosis established and in conjunction with the Hospital Infection Control Committee, we opted to keep the regimen due to improvement in clinical and laboratory parameters. Even with the patient being admitted on antibiotics, samples for general and anaerobic bacteria cultures were harvested; however, no bacterial growth was observed. The patient was discharged after 14 days of hospitalization, asymptomatic, with prescribed oral antibiotics to complete 21 days of treatment and oral anticoagulation therapy. After four months of anticoagulation therapy, a control resonance angiography was performed to monitor the disease, showing persistence of IJV thrombosis. The patient remains on anticoagulation medication on regular clinical visits basis, with follow up by Otolaryngology, Pediatric Hematology and Vascular Surgery teams.
DiscussionF. necrophorum is a Gram-negative anaerobic bacteria of the oropharyngeal flora capable of causing primary infection in healthy individuals with intact anatomical barriers. The condition begins with a sore throat and progresses to impairment of peritonsillar tissue, parapharyngeal space, IJV thrombophlebitis and, finally, septic emboli formation.2 The onset of sepsis occurs with marked fever (39–41°C, 102–106°F), typically 4–5 days after the start of sore throat and sometimes after improvement of the symptom.2 The appearance of the jaw angle bulging, or parallel to the sternocleidomastoid muscle, clinically reflects thrombophlebitis. Lungs are the primary site of abscess formation secondary to septic emboli; however, one can find multiple organ involvement.2,3 LS diagnosis involves: (1) recent oropharynx infection; (2) clinical or radiological evidence of IJV thrombosis; (3) isolation of anaerobic pathogens; (4) at least one septic focus.4 There is controversy in the literature regarding the classification of cases in which the pathogen cannot be isolated.2,3 However, considering that there are negative cultures in 12% of the cases,3 faced with the clinical condition and the difficulty of bacterial growth in patients during antibiotic therapy, we maintained the diagnosis and management in this case. Treatment includes antibiotics for 3–6 weeks, with coverage for anaerobes.5 Anticoagulation therapy is controversial, but it is widely used. In the absence of contraindications, the therapy must be considered, especially in patients with poor clinical response in spite of antibiotic.6
Final commentsAfter the advent of antibiotics, cases of LS practically disappeared, but there is evidence of its increased incidence in recent years, possibly associated with reduced use of antibiotics for sore throat. Described by André Lemierre as a “syndrome that is so characteristic that mistake is almost impossible”,1 this condition is potentially as serious as it is potentially treatable.3 A high degree of suspicion is crucial to avoid a delayed diagnosis with potentially fatal consequences.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Pinheiro PE, Miotto PD, Shigematsu NQ, Tamashiro E, Valera FC, Anselmo-Lima WT. Lemierre's syndrome: a pharyngotonsillitis complication. Braz J Otorhinolaryngol. 2015;81:115–6.
Institution: Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (USP), Ribeirão Preto, SP, Brazil.