Burkitt lymphoma (BL) is a highly aggressive type B non-Hodgkin's lymphoma (NHL) found in endemic, sporadic, and immunodeficiency-related presentations. All of them show the same morphological, immunohistochemical, and genetic characteristics, with different geographical and age distributions and affected organs.1,2 The great majority of sporadic and immunodeficiency-related cases are found in the abdomen (60–80%), followed by head and neck, where Waldeyer's ring extranodal involvement is usual (palatine tonsil and nasopharynx).1–3
This study aimed to report a case in which the patient presented BL as an early manifestation of acquired immunodeficiency syndrome (AIDS).
Case reportR.F.C., a 44-year-old mixed-race male locksmith, born in Bahia and living in São Paulo, presented to the Otorhinolaryngology Emergency Room with a bleeding nose followed by massive oral bleeding with hemodynamic instability, requiring a blood transfusion. Although previously healthy, the patient recounted a progressive left nasal obstruction that had become bilateral four months earlier, and was associated with a yellowish nasal discharge and anosmia. The condition progressed with trismus, dysphagia, bilateral earache, and left orbital pain. No hearing loss was present, but he had ear fullness. He also had lost 20kg in the past two months and was a 26 pack-years smoker, a social drinker, and a former intravenous cocaine user.
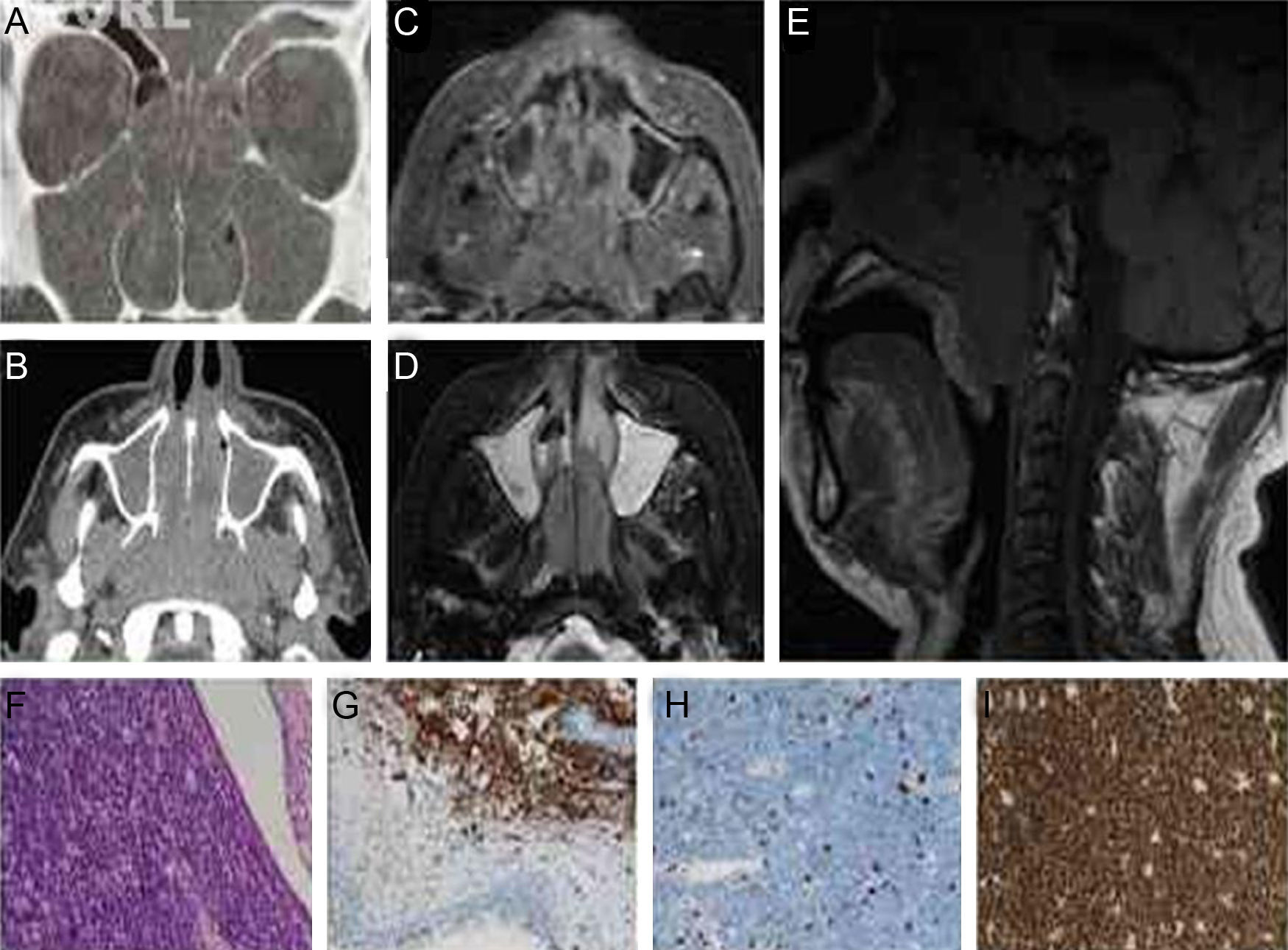
On physical examination, his general status was normal, and he had a pale conjunctiva, an emaciated appearance, mouth breathing, trismus, and a left convergent strabismus. Nasal endoscopy revealed a bilateral mucoid discharge and a pale, friable lesion that made the examination more difficult. Computed tomography and magnetic resonance imaging of paranasal sinuses (Fig. 1) showed an enlargement of the posterior wall of the nasopharynx with a post-contrast enhancement protruding into the choanae, nasal cavity, and oropharynx. Bone destruction was noted at the sphenoid sinus floor, and there was asymmetry in adjacent parapharyngeal fat planes, with an effacement on the left.
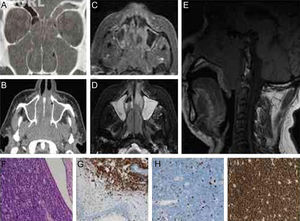
Computed tomography of paranasal sinuses. (A) Coronal view, bone window and (B) axial view, soft tissue window, with a soft tissue density lesion in the nasopharynx, nasal cavity, and sinuses; magnetic resonance imaging of paranasal sinuses, (C) axial view, contrast T1-weighted imaging, (D) T2-weighted view, (E) T1-weighted sagittal view with an enlargement of nasopharyngeal posterior wall and post-contrast enhancement protruding into the nasal cavity; lesion microscopy with (F) massive lymphoid cell proliferation, with submucous histiocytes containing intracytoplasmic stainable bodies with a starry sky appearance, (G) CD-20 positive neoplastic cells, (H) CD3-negative neoplastic cells, (I) virtually 100% of cells positive for Ki67, a cell proliferation marker.
An endoscopic incisional biopsy of the nasal cavity lesions and the hardened nasopharyngeal lesion was performed. An exposed and engorged vessel was identified in the nasopharynx, which could explain the severe bleeding from the mouth. Histopathological examination demonstrated basophil cells with numerous lipid vacuoles, round nuclei with dense chromatin and multiple nucleoli, and starry sky diffuse infiltration pattern consistent with classic BL. The immunohistochemistry confirmed Burkitt B-cell NHL, and was positive for CD20, CD3, CD10, Bc16, and ki67; and negative for Bc12, TdT, CD99, CD56, and EBV.
One week following the biopsy, there was a tumor enlargement, with proptosis, worsened dysphagia, respiratory distress, major health status worsening, and melena. The patient was admitted to the hospital with dehydration, malnutrition, acute kidney failure, severe sepsis criteria, and with the presence of a tumor lysis syndrome. Serological investigation revealed human immunodeficiency virus (HIV) infection with a CD4 count of 318. Bone marrow examination showed 63% blasts, thus demonstrating Burkitt leukemia. After proper clinical support, aggressive antiretroviral therapy and EPOCH-R-based chemotherapy were initiated. He underwent tracheostomy to secure the airway. After ten days of chemotherapy, he had no nasal obstruction and had responded favorably to treatment.
DiscussionBL may be the first AIDS-defining criterion, as this kind of lymphoma often occurs with high levels of CD4 (>200), that is, at an early stage of immunodeficiency with few symptoms.1,2,4 In developing countries, the concurrent diagnosis of HIV and lymphoma occurs in up to half of all cases, whereas the rate is substantially lower (around 10%) in developed countries, which highlights the difficulty of early HIV diagnosis in developing countries.4
Final remarksBL should be included in differential diagnosis of nasopharyngeal tumors even with no prior HIV diagnosis, as it can occur as an early manifestation of AIDS even in patients with a preserved immune status. Diagnostic suspicion should lead to an early biopsy due to the rapid course of this type of lymphoma, with prompt treatment performed by a hematologist and an infectious disease specialist.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Mascarenhas JG, Araújo Júnior F, Bolzan TV, Gregório LC, Kosugi EM. Nasopharyngeal Burkitt lymphoma as an early AIDS manifestation. Braz J Otorhinolaryngol. 2014;80:546–8.