An accessory parotid gland (APG) is present in 56% of the general population according to Toh et al.1 Although the pathology of the APG is similar to that found in the main parotid gland, the presence of an APG does not increase the risk for parotitis per se.2 Further, despite malignant pathology of the APG being reported in previous literature, obstructive sialolithiasis in the APG has rarely been reported.3–6
The main clinical feature of APG sialolithiasis is swelling located anterior to the main parotid gland, specifically when eating.6 Due to the APG’s location, it poses a potential diagnostic challenge to many doctors.
The aim of this paper is to report the first published case of a percutaneously extruded APG sialolithiasis during the perioperative period and to review the literature issues regarding chronic obstructive pathology affecting APG.
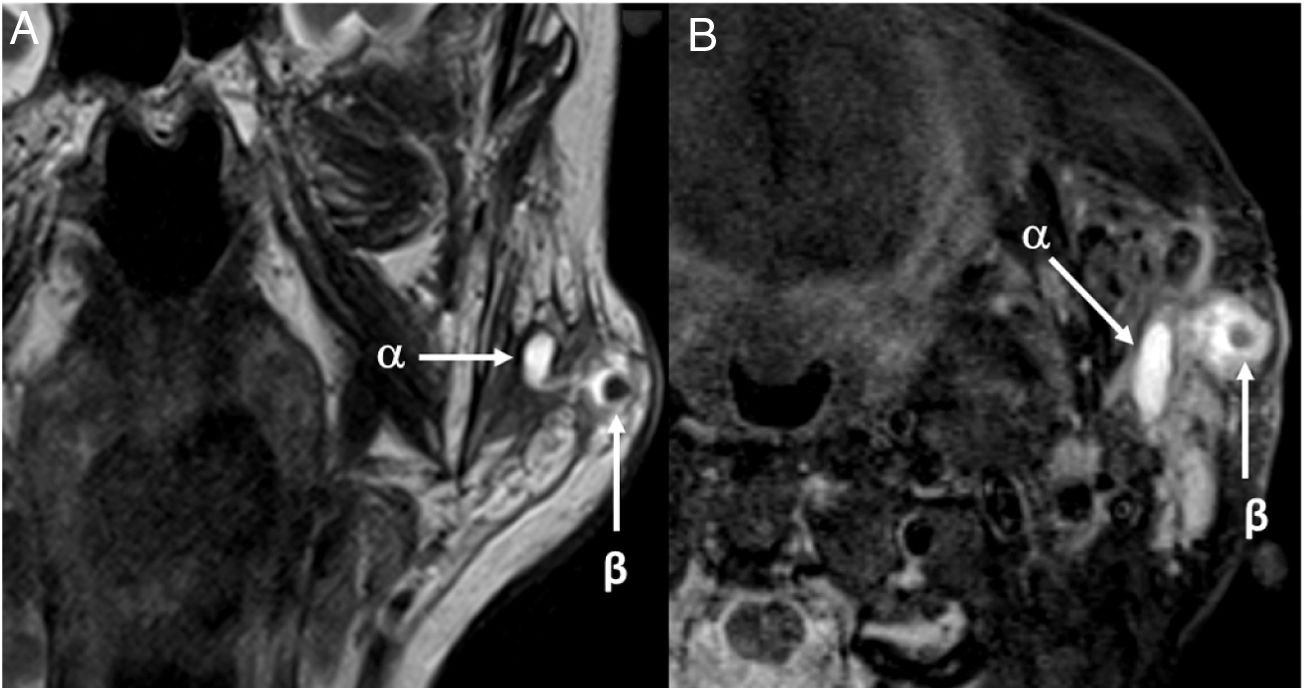
Case reportA 91-year-old female was admitted to the emergency department showing anterior left parotid swelling above the mandible bone (Fig. 1). Physical examination of the oral cavity confirmed the presence of a blockage of the left Stensen’s duct,resulting in pain in the left zygomatic area of the face. The salivary gland ultrasound showed a severe dilation of Stensen’s duct with the presence of a 4 mm sialith in a potential accessory gland. The diagnosis was completed with an MRI following sialography protocol, where acute inflammatory changes were confirmed and a 4 mm sialith in the left APG was present (Fig. 2). Additionally, the presence of moderate stenosis of the main duct was evidenced, leading to severe retrograde dilation of the Stensen’s duct and acute inflammatory changes in the main parotid (Fig. 3). Therefore, the patient was diagnosed with APG sialadenitis caused by sialolithiasis.
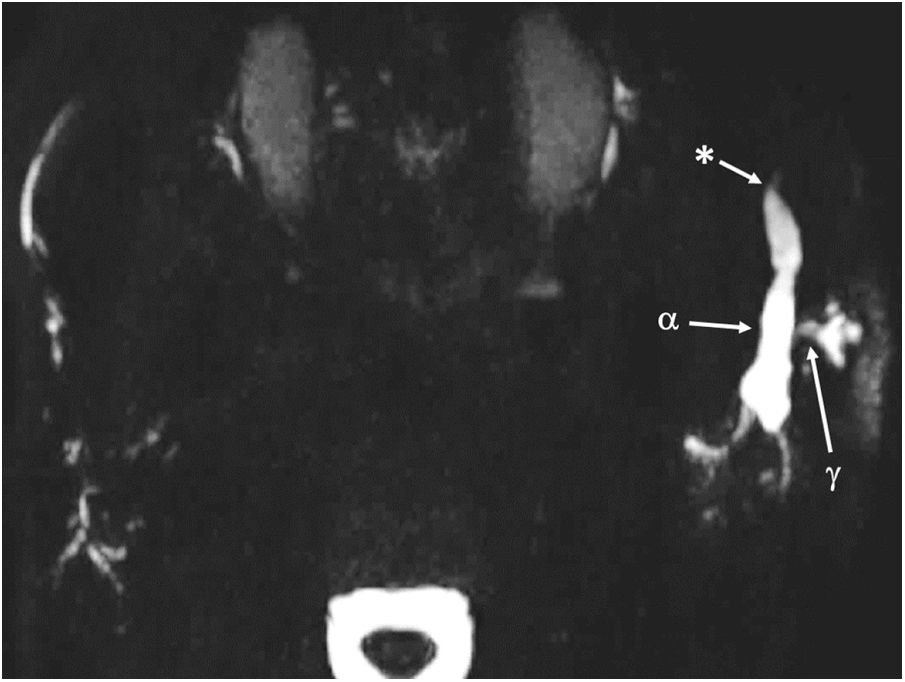
Axial MIP of 3D MR sialography demonstrates the presence of small ductules anterior and lateral to the left parotid gland draining into the main Stensen’s duct (α), in keeping with an accessory parotid lobe. Stensen’s duct is severely dilated (γ) secondary to a tight distal stricture (*).
According to the technique described by Nahieli,7 percutaneous extraction of the lithiasis under local anaesthesia and sedation was considered due to the age of the patient.
Surprisingly, the patient returned to the department two days later concerned about progressive skin ulceration on the left cheek with purulent discharge (Fig. 1). In view of these findings at the outpatient clinic, we proceeded under local anesthesia (articaine with epinephrine) debridement and complete removal of the left APG intraglandular 5 × 3 mm sialolith was carried out. A strip of gauze with terramycin was placed in the skin defect and oral antibiotic treatment (amoxicillin-clavulanic 875/125 mg every 8 h for 10 days) was prescribed. After 2 weeks, the skin wound was completely healed, and the patient's symptomatology had ceased. After a 6 month followup, the patient was asymptomatic and no chronic obstructive sialadenitis signs were observed.
DiscussionThe APG is located in the lateral area of the face behind the zygomatic process, usually anterior to the parotid gland, parallel to Stensen’s duct and superficial to the masseter muscle.8 An APG can be situated either superior or inferior to Stensen’s duct. Despite its prevalence in more than 50% of human beings,1 APG disorders can create a diagnostic challenge when its existence is unsuspected..
The accessory glandular tissue, unlike the main parotid gland, presents both serous and mucous acines.1 This histopathological characteristic reveals a lack of differentiation of the APG. The main parotid gland shows mixed acines9 only in the neonatal stage and serous acines are predominant in adulthood. Mucous acines are known to be more prone to sialolithiasis, as is the case with the submandibular glands.10 Thus, presence of mucous acines could justify the APG’s predisposition to developing sialolithiasis.
In previous literature there are multiple publications reporting different tumors originating in the APG. Among benign tumors that affect it, pleomorphic adenoma is the most common. As for the malignant tumors mucoepidermoid carcinoma, lymphoma, lymphoepithelioma or acinar cell carcinoma are the most common.4
Very few articles are available on chronic obstructive sialadenitis that specifically affects the APG caused by sialolithiasis.3–6 Nevertheless, a spontaneous cutaneous extrusion of an accessory parotid gland lithiasis was not found in the searched medical literature.
Recently, the possible participation of the APG in the development of parotid sialadenitis has been postulated.2 The presence of APG and the length of Stensen,s duct along with any stones inside the accessory gland3,5 have been linked, and are significant for the development of parotitis.
Patients suffering from APG sialolithiasis commonly describe an anterior parotid swelling, usually when eating, which could involve the main parotid gland. The clinical diagnosis should be investigated with a radiological study consisting of ultrasound and/or a CT or MRI. In recent years, the use of magnetic resonance sialography has been recommended. MRI techniques can demonstrate with high specificity the presence of strictures, minute stones or other less frequent causes of obstruction10 while sparing the patient the exposure to radiation associated with a CT scan.
Treatment for APG sialolithiasis has not yet been standardised due to the unusual nature of this pathology. Most authors advocate conservative treatment as a first step, with oral antibiotics and anti-inflammatory drugs for the infection and pain.6 Surgical treatment is probably most appropriate when the symptoms recur after medical failure. The recommended surgical approach for the removal of the APG and its lithiasis4,5 is through a parotidectomy incision and dissection anteriorly to the parotid gland in order to reach the APG. On the other hand, a transoral approach with a microscope, and under strict facial nerve monitoring,3 can also be considered.
ConclusionThe accessory parotid gland may suffer from chronic obstructive sialadenitis related to sialolithiasis. Knowledge of the presence of the accessory parotid gland should be disseminated so medical practitioners are able to perform an early diagnosis and treatment, and ultimately avoid associated complications such as facial skin ulceration and lithiasis extrusion.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.