Mucopolysaccharidosis is a hereditary lysosomal storage disease, which develops due to a deficiency in the enzymes that play a role in the metabolism of glycosaminoglycans (GAG). The incidence of mucopolysaccharidosis is 1/25,000, with autosomal recessive inheritance (except for MPS II). Mucopolysaccharidosis occurs in seven different types, each with a different congenital deficiency of lysosomal enzymes. In mucopolysaccharidosis patients, even though progression of clinical findings is not prominent, the disease advances and causes death at early ages. Facial dysmorphism, growth retardation, mental retardation, and skeletal or joint dysplasia are the most frequently found symptoms in these patients.
ObjectiveThe purpose of our study is to present the types of hearing loss types and tympanometric findings of patients with mucopolysaccharidosis referred to our clinic with suspicion of hearing loss.
MethodsAfter otorhinolaryngological examination, 9 patients with different types of mucopolysaccharidosis, underwent to immittance and audiometric evaluations, performed according to their physical and mental abilities, and ages, in order to determine their hearing thresholds.
ResultsThe audiometric findings of the 9 patients followed with mucopolysaccharidosis were reported separately for each case.
ConclusionBased on the high frequency of hearing loss in mucopolysaccharidosis patients, early and detailed audiological evaluations are highly desirable. Therefore, regular and systematic multidisciplinary evaluations are very important.
Mucopolissacaridose (MPS) é uma doença hereditária de depósito lisossômico, decorrente da deficiência das enzimas que influenciam o metabolismo dos glicosaminoglicanos (GAGs). A incidência de MPS é de 1/25.000 habitantes, resultante de herança autossômica recessiva (exceto no caso de MPS II). MPS se apresenta na forma de sete tipos diferentes e, em cada tipo, ocorre uma deficiência congênita distinta de enzimas lisossômicas. Embora em pacientes com MPS os achados clínicos não sejam geralmente observados, a doença progride em seu curso natural e costuma levar a óbito pacientes muito jovens. Dismorfismo facial, retardo de crescimento, retardo mental e displasia esquelética ou articular são os sinais e sintomas mais frequentemente observados nesses pacientes.
ObjetivoA finalidade do presente estudo foi apresentar os tipos de perda auditiva e os achados timpanométricos de pacientes com MPS encaminhados para nossa clínica com suspeita de perda auditiva.
MétodoEm seguida ao exame otorrinolaringológico, nove pacientes com diferentes tipos de MPS, foram submetidos a avaliações imitanciométricas e testes audiométricos de acordo com sua faixa etária eficiência física e mental, no intuito de identificar seus limiares auditivos.
ResultadosOs achados audiométricos dos nove pacientes acompanhados por MPS foram descritos separadamente para cada caso.
ConclusãoBaseado na alta frequência de perda auditiva em pacientes com MPS, avaliação audiológica precoce e detalhada é altamente desejável. Para tanto, é importante que sejam realizados avaliações multidisciplinares periódicas e sistemáticas.
Mucopolysaccharidosis (MPS) is a hereditary lysosomal storage disease, which develops due to the deficiency in the enzymes that play a role in the metabolism of glycosaminoglycans (GAG). Progressive GAG accumulation causes advanced growth retardation, skeletal deformities, hearing loss, weak joint movement, and facial dysmorphism. In accordance with the deficiency of the known 11 enzymes, MPS has seven sub-types (MPS I, MPS II, MPS III, MPS IV, MPS VI, MPS VII, MPS IX). Although the incidence of MPS in accordance with its sub-types varies, a general incidence of 1/25,000 has been reported.1–3
In patients with MPS, hearing loss is observed due to various reasons. Conductive hearing loss (CHL) may develop due to recurrent upper respiratory tract infections and serous otitis media or bone chain deformities. Sensorineural hearing loss (SHL) is thought to be caused due to the accumulation of GAG in the cochlea, auditory nerve, and brain stem. In many patients, mixed-type hearing loss, along with the symptoms of conductive and sensorineural hearing loss, can also be seen. In CHL related to middle ear effusion, while the ventilation tube implementation is frequently used as treatment, hearing aids are advised in SHL.4–7 Early diagnosis of hearing losses carries great importance in terms of early intervention in MPS patients, as well as in all other patients.8,9
The purpose of the present study was to present the hearing loss type, degree, and tympanometric findings of patients with MPS, who are directed to this clinic with the suspicion of hearing loss.
MethodsThe nine patients who had been directed to this department with the suspicion of hearing loss, whose follow-up had been conducted after they have been diagnosed with MPS, were included in this study (Ethical Committee approval number: GÜKAEK-461). The otological examinations of the patients were performed by the otorhinolaryngologist. Information related to each patient's otorhinolaryngological complaints and treatments were compiled and middle ear infection, ear discharge, tinnitus, dizziness, tympanum problems, adenoidectomy, ear tube placement, and hearing aid usage were determined. After the otorhinolaryngological examination, the immitancemetric evaluations were conducted and tests which are appropriate for the patients’ ages, physical and mental efficiencies, and both air and bone conduction thresholds were determined at 250, 500, 1000, 2000, 4000, 6000, and 8000Hz.
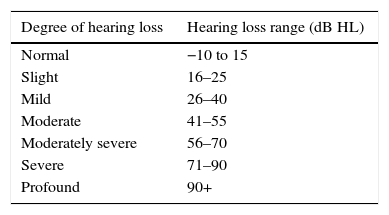
The hearing loss levels were determined by taking the average of pure tone air conduction thresholds, determined at 0.5, 1, 2, and 4kHz, in accordance with the intervals given in Table 1.
Hear loss was classified under three groups as conductive, mixed, and sensorineural. For CHL, while the bone hearing thresholds were present audiometrically (less than 20dB), it has been accepted that; the average air-bone gap in 0.5, 1, 2kHz to be more than 15dB; in mixed type hearing losses, bone hearing thresholds to be 20dB and over audiometrically and the average air-bone gap to be more than 15dB in 0.5, 1, 2kHz; in sensorineural hearing loss (SHL), the difference between the air and bone conduction thresholds to be less than 15dB in average in 0.5, 1, 2kHz.
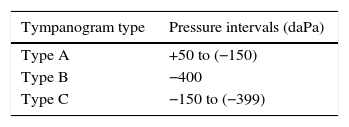
In the tympanometrical evaluation, 225Hz probe tone signals were used. The tympanogram types were evaluated in accordance with the values given in Table 2.
For the statistical analysis, SPSS version 16.0 (SPSS Inc., Chicago, IL, United States) was used. For the age average and standard deviation (SD), descriptive statistics were developed.
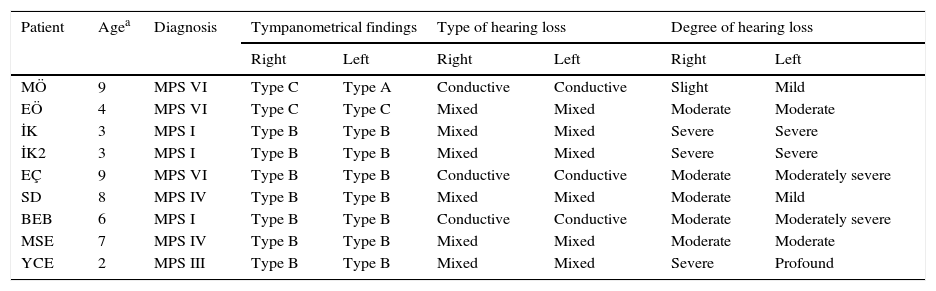
ResultsThe age average of the total of nine patients with MPS, four female (44.44%) and five male (55.55%), was determined as 5.66±2.73. There were three cases of MPS VI (33.33%), three cases of MPS I (33.33%), one case of MPS III (11.11%), and two cases of MPS IV (22.22%) that were diagnosed. Cases MÖ and EÖ are siblings; İK and İK 2 are twins. The other five patients are not related. The degree of hearing loss, its type, and tympanometrical findings are shown in Table 3. There were six ears with conductive hearing loss (33.33%) (HL one ear: slight; HL one ear: mild; HL two ears: moderate, and HL two ears: moderately severe); 12 ears with mixed hearing loss (66.66%) (HL two ears: mild; HL four ears: moderate, HL five ears: severe, and HL one ear: profound) were determined. There were 14 ears with Type B tympanogram (77.77%), three ears with Type C tympanogram (16.66%), and one ear with Type A tympanogram (5.55%). E.Ç., B.E.B., and MSE had a bilateral ventilation tube (VT) inserted. Although the other patients were advised regarding the VT application as well, it has not been carried out upon the wish of their families. With the exception of MÖ and BEB, although all patients were advised to use hearing aids, the families did not adopt the use of these devices and did not come regularly for follow-ups.
Audiometrical findings of patients with MPS.
| Patient | Agea | Diagnosis | Tympanometrical findings | Type of hearing loss | Degree of hearing loss | |||
|---|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | |||
| MÖ | 9 | MPS VI | Type C | Type A | Conductive | Conductive | Slight | Mild |
| EÖ | 4 | MPS VI | Type C | Type C | Mixed | Mixed | Moderate | Moderate |
| İK | 3 | MPS I | Type B | Type B | Mixed | Mixed | Severe | Severe |
| İK2 | 3 | MPS I | Type B | Type B | Mixed | Mixed | Severe | Severe |
| EÇ | 9 | MPS VI | Type B | Type B | Conductive | Conductive | Moderate | Moderately severe |
| SD | 8 | MPS IV | Type B | Type B | Mixed | Mixed | Moderate | Mild |
| BEB | 6 | MPS I | Type B | Type B | Conductive | Conductive | Moderate | Moderately severe |
| MSE | 7 | MPS IV | Type B | Type B | Mixed | Mixed | Moderate | Moderate |
| YCE | 2 | MPS III | Type B | Type B | Mixed | Mixed | Severe | Profound |
In cases with MPS (Table 4), the initiation of treatment in early stages carries great importance in terms of the prognosis of the disease. However, due to the late appearance of the symptoms, the definite diagnosis range is 3–4 years of age. In the follow-up of the stages of the treatments of patients with MPS, the otolaryngologist and audiologists have a significant role in multidisciplinary teamwork. Recurrent serous otitis media and hearing loss that develops in individuals within this disease group are the reasons why better, long-term follow-ups should be done. Hearing loss can be seen in various types and degrees in MPS in general.10–13 Overall, conductive hearing losses due to chronic effusion and eustachian tube dysfunction are seen more in patients with MPS; the incidence of SHL has not been determined very clearly.10
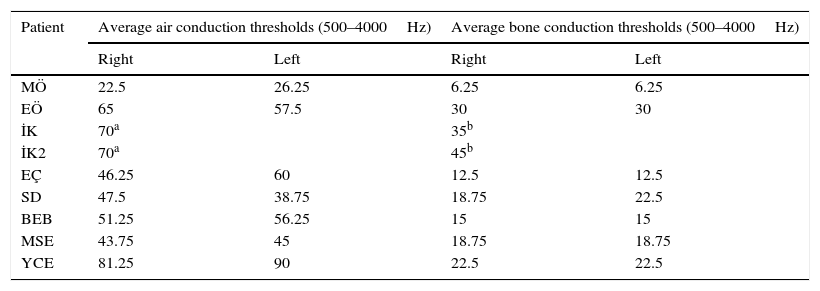
Air and bone conduction thresholds of patients with MPS (dB HL).
| Patient | Average air conduction thresholds (500–4000Hz) | Average bone conduction thresholds (500–4000Hz) | ||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| MÖ | 22.5 | 26.25 | 6.25 | 6.25 |
| EÖ | 65 | 57.5 | 30 | 30 |
| İK | 70a | 35b | ||
| İK2 | 70a | 45b | ||
| EÇ | 46.25 | 60 | 12.5 | 12.5 |
| SD | 47.5 | 38.75 | 18.75 | 22.5 |
| BEB | 51.25 | 56.25 | 15 | 15 |
| MSE | 43.75 | 45 | 18.75 | 18.75 |
| YCE | 81.25 | 90 | 22.5 | 22.5 |
Although conductive and mixed-type hearing loss were observed in the cases of the present study, SHL compatible with literature has not been determined. In the studies conducted, it was stated that the incidence of mixed hearing loss is more, and that this fact is related with age. While conductive hearing loss is determined in early ages and in patients who are diagnosed earlier, it has been stated that mixed hearing loss can be observed, and that this rate is between 33% and 71% as age increases. In the present cases, degree of hearing loss was determined from slight to severe. This difference is considered to be due to GAG's excessive accumulation in the cochlear ducts, stria vascularis, and cochlear nerve, which prevents them from functioning efficiently.14 In the present cases, the incidence of Type B and C tympanogram was determined to be high, in accordance with the literature. According to Yu Lin et al., while this rate is stated to reach 70%, the incidence of Type B tympanogram was determined as 77.77% and the incidence of Type C tympanogram was determined as 16.66% in the present study, similarly. VT application is advised to cases with similar clinical findings in different clinics as well, just as in the present study. However, a majority of the cases in this study have hindered their treatments, due to their families’ rejection of the VT application. In cases for which hearing aids are advised, while socio-economical inadequacy creates hardships in coming to follow-ups and obtaining these aids, the fact that many live in different cities prevents continuity in follow-ups.
ConclusionIn cases with MPS, since the incidence of hearing loss is high, the hearing loss should be determined in early stages. After the diagnosis, the required treatments should be started promptly and thus quality of life should be increased. However, it is considered that this is only possible as a result of regular and systematic follow-ups and with multidisciplinary studies.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Gökdoğan Ç, Altinyay Ş, Gökdoğan O, Tutar H, Gündüz B, Okur İ, et al. Audiologic evaluations of children with mucopolysaccharidosis. Braz J Otorhinolaryngol. 2016;82:281–4.