Knowledge of the different imaging tests and their appropriate indications is crucial to establish the diagnosis of temporomandibular disorders, especially in patients with overlapping signs and symptoms.
ObjectiveTo present and assess the main diagnostic imaging tests for temporomandibular disorders and rationally discuss their indication criteria, advantages, and disadvantages.
MethodsLiterature review in the Web of Knowledge, PubMed and SciELO databases, as well as manual search for relevant publications in reference lists of the selected articles.
ResultsComputed tomography and magnetic resonance imaging were considered the gold standard assessments for the temporomandibular joint to evaluate hard and soft tissues, respectively. Each diagnostic method exhibited distinct sensitivity and specificity for the different subtypes of joint dysfunction.
ConclusionSelecting an evaluation examination based on its accuracy, safety, and clinical relevance is a rational decision that can help lead to an accurate diagnosis and an optimum treatment plan.
O conhecimento dos distintos exames de imagem e sua correta indicação é fundamental para elaboração do diagnóstico das disfunções temporomandibulares, principalmente em pacientes com grande sobreposição de sinais e sintomas.
ObjetivoApresentar e avaliar os principais exames de diagnóstico por imagem das disfunções temporomandibulares, além de discutir racionalmente os seus critérios de indicação, vantagens e desvantagens.
MétodoRevisão da literatura nas bases de dados Web of Knowledge, PubMed e SciELO, além de busca manual por publicações relevantes nas listas de referências dos artigos selecionados.
ResultadoOs exames de tomografia computadorizada e ressonância magnética foram considerados “padrão-ouro” para a avaliação dos tecidos duros e moles, respectivamente, da articulação temporomandibular. Cada método de diagnóstico pesquisado apresentou sensibilidade e especificidade distintas para os diferentes subtipos de disfunção da articulação.
ConclusãoConsidera-se como racional a indicação fundamentada na acurácia, segurança e relevância clínica do exame a ser solicitado, o que implica na adequada determinação do diagnóstico e do plano de tratamento.
The temporomandibular joint (TMJ) is a composite ginglymus-arthrodial joint, whose components are the condyle, glenoid cavity and articular tubercle, articular disc, retrodiscal tissue, synovial membrane, and joint capsule.1 It is the most frequently used joint of the human body and has simultaneous bilateral capacity to move the mandible.2,3
Its components often undergo remodeling and adaptation processes. In the presence of temporomandibular disorders (TMD), structural alterations and functional disorders are commonly observed.2,3
In most cases, symptoms are diffuse and imprecisely manifested as masticatory myalgia, arthralgia, headache, otalgia, and neck pain, among others.4–8 Pain in more than one area is common and often leads patients to seek evaluation from various medical and dental specialists, including otorhinolaryngologists.6,8
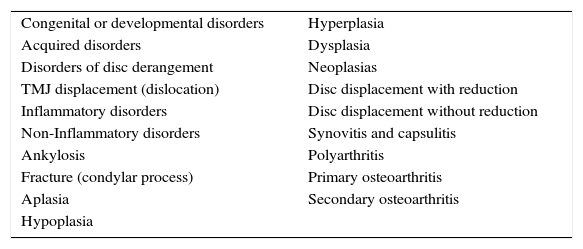
For instructional purposes, the American Academy of Orofacial Pain (AAOP) has classified TMD into two major groups: muscle and joint pain.9 It is estimated that temporomandibular joint disorders (TMJD) affect approximately 30% of the population in asymptomatic form, as internal joint derangement, comprising disc dislocation and structural changes resulting from osteoarthritis and osteoarthrosis.2,10,11 The diagnostic subtypes TMJD can be seen in Table 1.
Diagnostic classification proposed by the AAOP.12
| Congenital or developmental disorders | Hyperplasia |
| Acquired disorders | Dysplasia |
| Disorders of disc derangement | Neoplasias |
| TMJ displacement (dislocation) | Disc displacement with reduction |
| Inflammatory disorders | Disc displacement without reduction |
| Non-Inflammatory disorders | Synovitis and capsulitis |
| Ankylosis | Polyarthritis |
| Fracture (condylar process) | Primary osteoarthritis |
| Aplasia | Secondary osteoarthritis |
| Hypoplasia |
AAOP, American Academy of Orofacial Pain.
The etiology of TMJD is not fully understood6,8,12 and is related to the presence of risk factors such as trauma, parafunctional habits, postural condition, occlusal microtrauma, systemic predisposition, sleep disorders, and deleterious psychosocial alterations.6–8,11,13
The diagnosis of TMJD is achieved by evaluating the medical history and by physical examination.6,8,14 However, diagnostic TMJ imaging methods are used to assess the integrity of its components and their functional association, to confirm the extent or progression of an existing disease, and to assess and document the effects of an already established treatment.9,15 They are essential for assessment in cases of trauma, occlusal alterations and sudden limitation of mouth opening, presence of joint noises, systemic joint diseases, infection and failure of conservative treatments.13
ObjectivesThis study discusses the main imaging techniques for the assessment of TMJ and adjacent structures and their indications for the diagnosis of joint alterations, rationally evaluating their advantages and disadvantages.
MethodUsing the ISI Web of Knowledge, PubMed, and SciELO databases, a search was carried out for literature articles published and made available in the years 2004–2014, in English or Portuguese, that contained the keywords “temporomandibular joint disorder” and “diagnostic imaging test.”
There were 51 articles found in the ISI Web of Knowledge database, 117 in PubMed, and 25 in SciELO. Basic research experimental articles, letters to the editor, and isolated case reports were excluded. A total of 23 articles, characterized as clinical trials, comparative studies, reviews, and case group studies comprised the first stage of the research.
Then, based on the same inclusion criteria, a literature search was performed in the five most frequently cited radiology journals for the years 2004–2014. In this search, six new references were found in addition to the previously selected articles. Four other relevant publications cited in the selected articles’ lists of references were added, including historical ones dated prior to 2004.
According to the requirements defined in CNS Resolution 196/96, this study was submitted to the Research Ethics Committee, approved under No. 133/2009, designed to demonstrate the major changes in the TMJ as disclosed by imaging tests.
Temporomandibular joint imaging assessmentRadiographic examinationsTMJ radiographs provide information on the morphological characteristics of osseus components of the joint and certain functional associations between the condyle, articular tubercle and fossa, but are inefficient for evaluating the soft tissues.1,14,16
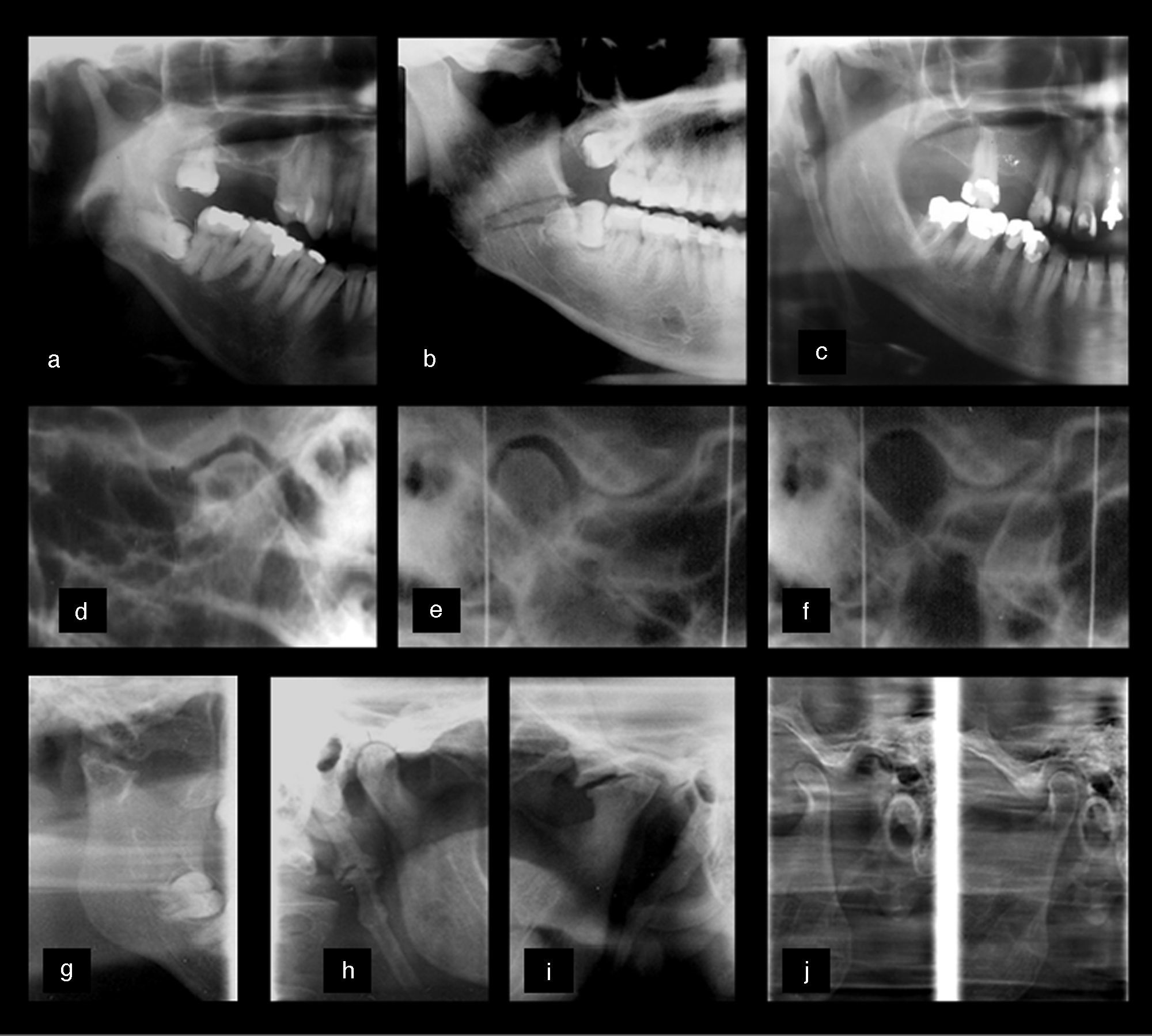
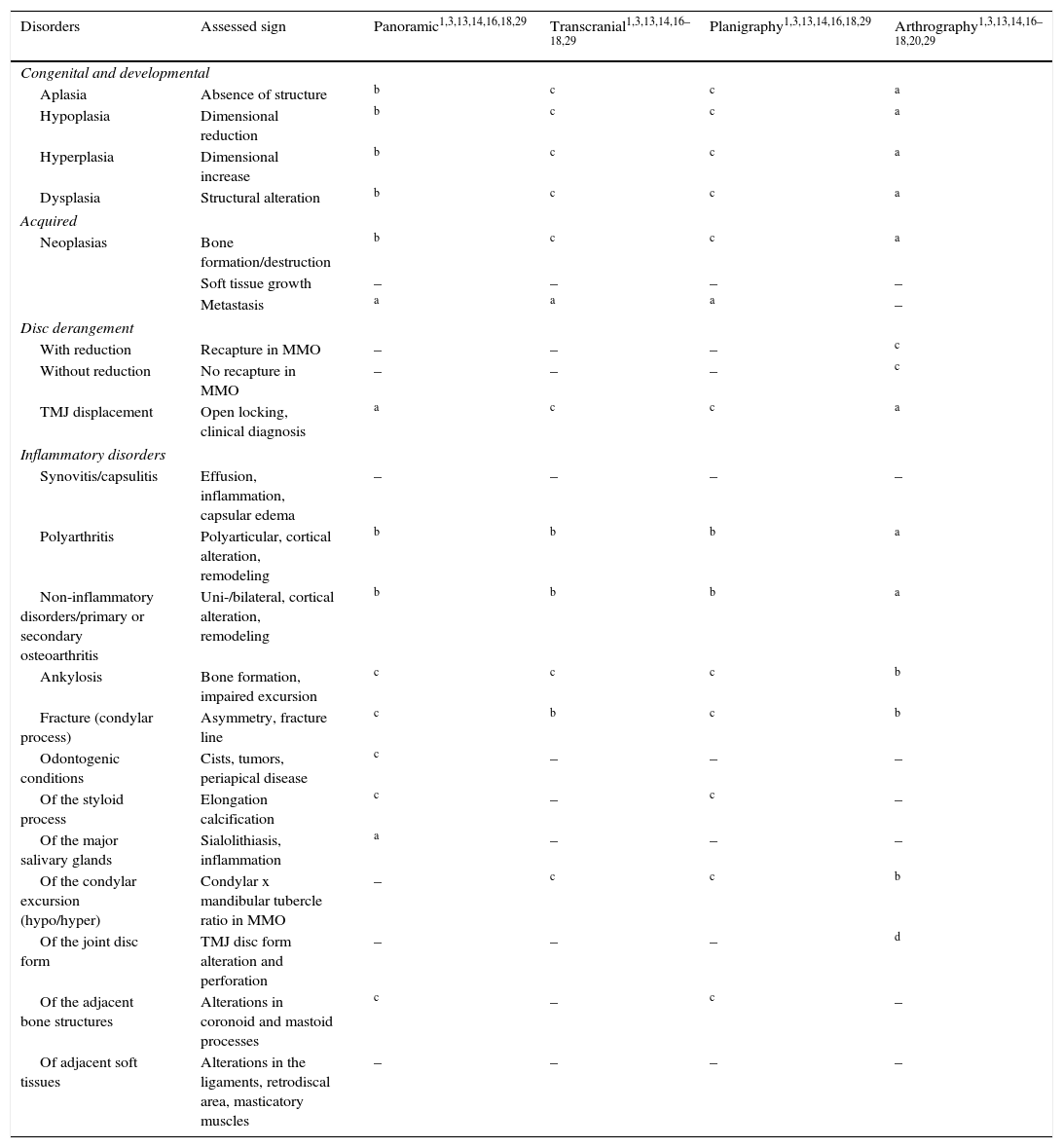
Several anatomical and technical factors can prevent a clear and unobstructed radiographic image of the TMJ.16,17 When choosing TMJ radiography, one needs to consider the identification of boney structural details, the specific suspected clinical disorder, the amount of symptomatic information clinically available for the diagnosis, the cost of these examinations, and their radiation dose.3,14 The radiographic techniques most often used in the routine management of TMJD are panoramic radiography, planigraphy, and transcranial radiography1,3,13,15 (Fig. 1).
Radiographic assessments of different TMDs. (a–c) Close-up in panoramic image showing mandibular condyle hypoplasia (a), horizontal impaction of the third molar (a, b) fracture line in the region of gonial angle (b) and elongated styloid process. The transcranial images (d–f) show the presence of osteophytes (d), preservation of joint spaces in maximum habitual intercuspation (MHI) (e) and the identification of condylar hyperexcursion (f). The planography techniques (g–j) demonstrate: mandibular neck fracture and ankylosis (g) elongated styloid process (h), advanced remodeling process, superior-anterior flattening, cortical irregularities, and osteophyte formation (i) in addition to mandibular head hyperexcursion, defining TMJ hypermobility (j).
As it provides a maxillary overview, it is useful in the differential diagnosis of odontogenic alterations whose symptoms overlap with TMJD.13,18 It can reveal advanced bone alterations in the condyle, such as asymmetries, erosions, osteophytes, fractures, changes in size and shape, degenerative and inflammatory processes, growth alterations, maxillary tumors, metastases, and ankylosis.1,13,15,16 However, it does not provide functional information on condylar excursion.14 Also, only gross alterations in the articular tubercle morphology can be seen because of the superimposition of images of the skull base and the zygomatic arch.3,14,16,18 This technique is useful as a screening tool, as it allows the initial diagnosis and assessment of TMJ alterations that are not so subtle.15 It is also indicated when the patient has reduced mouth opening and the differential diagnosis of fracture is considered.1,3
Planigraphy (or panoramic radiography with programs for TMJ)This method provides considerable accuracy and produces images without much overlap. It visualizes the articular boney detail and reveals any anatomical abnormalities in structures adjacent to the TMJ, such as the styloid process, mastoid process, and zygomatic arch.3,15 It can be obtained in the sagittal and coronal planes, documenting the relationship of the condyle with the articular fossa in maximum habitual intercuspation (MHI) and the excursion extension during maximal mouth opening (MMO). It provides a direct comparison of both sides regarding the hypo-, normo-, or hyperexcursion of the condyle, which is useful in confirming a clinical suspicion of hypermobility.1,3
In spite of the relative identification of the TMJ boney structures, it does exhibit some magnification that is inherent to the technique. However, it is useful for functional assessment of mouth opening, evaluation of morphological alteration and the joint spaces, analysis of dimension, fractures, and ankylosis.3
Transcranial radiographySimilarly to the planigraphy, this evaluation provides good anatomical assessment of the condyle, fossa, and articular tubercle.1,14,17 In this technique, an X-ray beam is obliquely directed through the skull to the contralateral TMJ, producing a sagittal view.17 Thus, the central and medial portions of the condyle are projected inferiorly and only the lateral joint contour is displayed.17 It is useful to identify bone alterations and displaced fractures of the head and neck of the mandibular condyle, as well as to assess excursion and to determine radiographic joint spaces.3,14,17
This type of projection is limited by the fact that it produces an image with a large overlap of the skull bones; it also requires the use of a specific cephalostat for standardization, usually requiring complex positioning.1,13,14,17
ArthrographyArthrography is a variant of the radiographic technique for TMJ, which aims to assess the TMJ soft tissues. In the 1970s and 1980s, arthrography was the method of choice for the identification of disc displacement.14,15,19 Disc morphology, positioning, and function were indirectly identified by contrast injection into the superior and/or inferior joint spaces.14 After the injection, dynamic images were obtained, recording mandibular movements.20
Even though it is useful for disc position identification, arthrography is not currently recommended as it is an invasive procedure and carries a risk of iatrogenic disc perforation and facial nerve damage.14 There are also the risks of radiation to radiosensitive structures (crystalline and thyroid), pain and limitation of movement after the injections, infections, allergies to the injected dye, and it is an examination that is considered difficult to perform.1,14,15,20
Other combined radiographic techniquesDue to the two-dimensional radiographic visualization of the TMJ, the combined use of different techniques is necessary to provide an accurate diagnosis and location of the alterations. The evaluation of the structures in different planes illuminates fracture extension, degenerative joint disease, postoperative status, ankylosis, and neoplasms.3 Additionally, the anatomic relations of areas adjacent to the lesion can be studied with greater diagnostic accuracy, providing more efficient surgical and therapeutic planning.15 The main combined views are submental (or submento-vertex), transpharyngeal, transmaxillary, reverse Towne, posterior–anterior, and lateral teleradiography.3,13,15
Despite their lower cost, technical simplicity, and lower levels of radiation, the use of combined radiographic images has become less common due to increasing use and availability of accurate images such as cone-beam computed tomography, which assess hard tissues in the three anatomical planes and are widely used in dental diagnosis.13,15
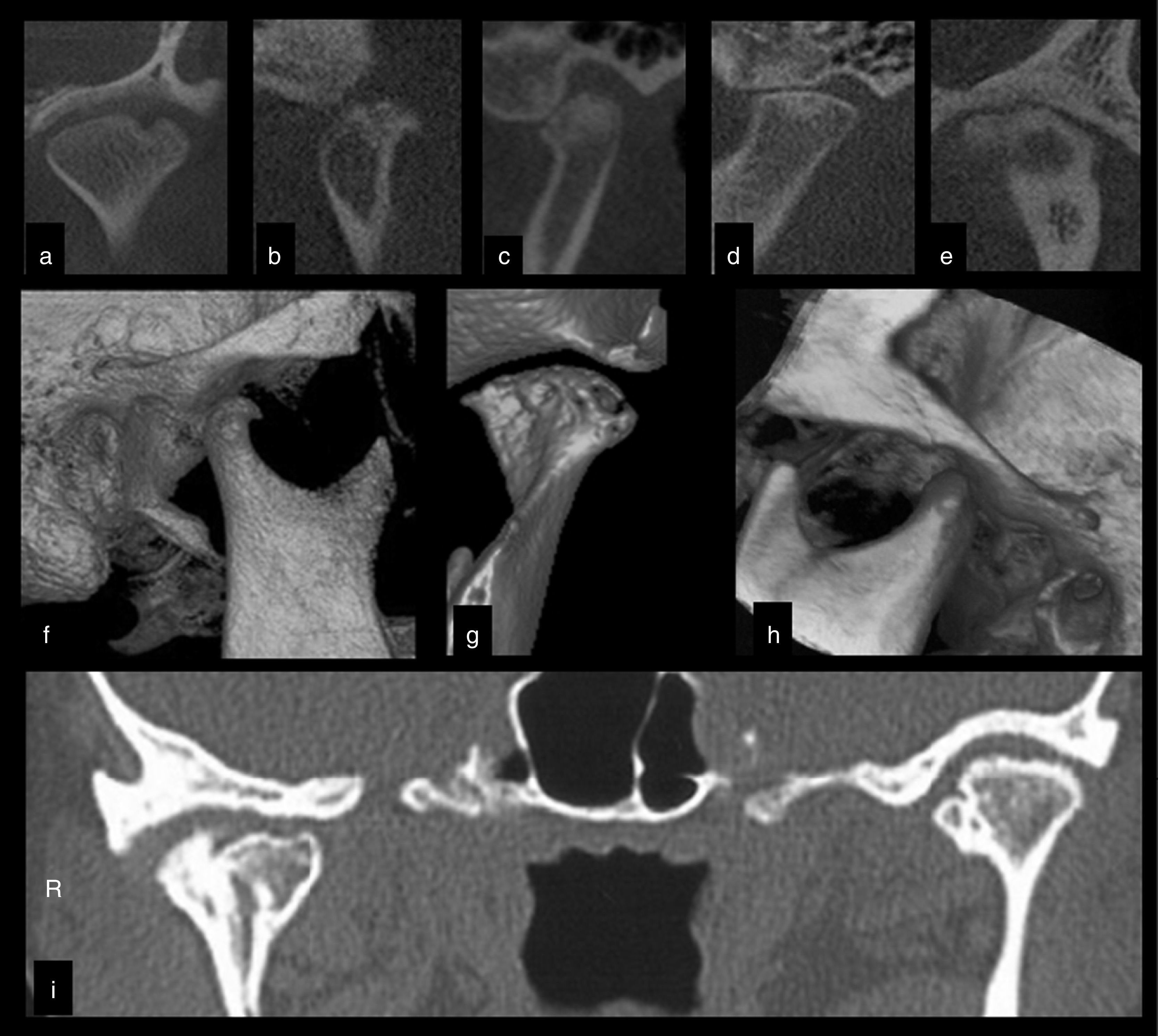
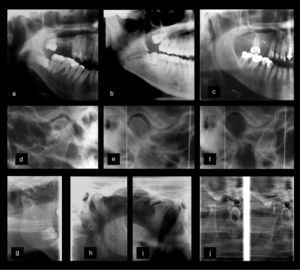
Computed tomography (CT)CT comprises a set of images obtained through a sophisticated and highly accurate technique, compared to plane radiographs.2 Recently, cone-beam computed tomography (CBCT) technology has been used for dental diagnosis due to its specific use for the maxillofacial region.3,21 Its main advantage is the observation of boney joint structures in the sagittal, coronal, and axial planes,1,21 in addition to the possible image manipulation at different depths and three-dimensional reconstruction14,21 through specific software. The examination time varies between 10 and 70s, and the radiation dose is much lower compared to the helical technique.3,21
The main indications of CBCT include structural assessment of bone components of the TMJ, which precisely determines the location and extent of boney alterations: fractures, neoplasms, and ankylosis; erosive degenerative, pseudocystic, and osteophytic alterations; presence of asymptomatic bone remodeling; evaluation of post-surgical conditions; hyperplasia of condylar, coronoid, and styloid processes; persistent foramen of Huschke; as well as intraarticular calcification derived from synovial chondromatosis or metabolic arthritis.2,14,15
Hard tissues, teeth, and bones are well demonstrated and measured in their real morphological condition, with minimal noise and artifacts.1,18,22 However, few details are provided on soft tissue and it is not possible to evaluate the joint disc.3,22
Significant disadvantages are the cost of the examination and exposure to significant levels of radiation compared to conventional radiographic techniques.1,14,15,18
Fig. 2 shows morphological alterations in joint bone components diagnosed by the CBCT technique.
Cone-beam computed tomography (CBCT) assessment of different TMJs in the coronal (a, e) and parasagittal (b–d) views. (a) Coronal view showing extensive erosion. Note the presence of bone sclerosis, cortical irregularities, and osteophytic formation in (b), (c), and (e). The presence of subchondral cysts can be observed in (c) and (e). Advanced flattening of bone components and decreased joint space are recorded in (d). Advanced degenerative osteoarthritis alteration is observed in e. Three-dimensional reconstructions (f–h) show osteophytes (f, g), advanced erosion (g) and hyperexcursion of the mandibular condyle (h). (i) The coronal view of the right and left TMJ shows alteration of the mandibular condyle and hyperdense images in the joint spaces compatible with synovial chondromatosis.
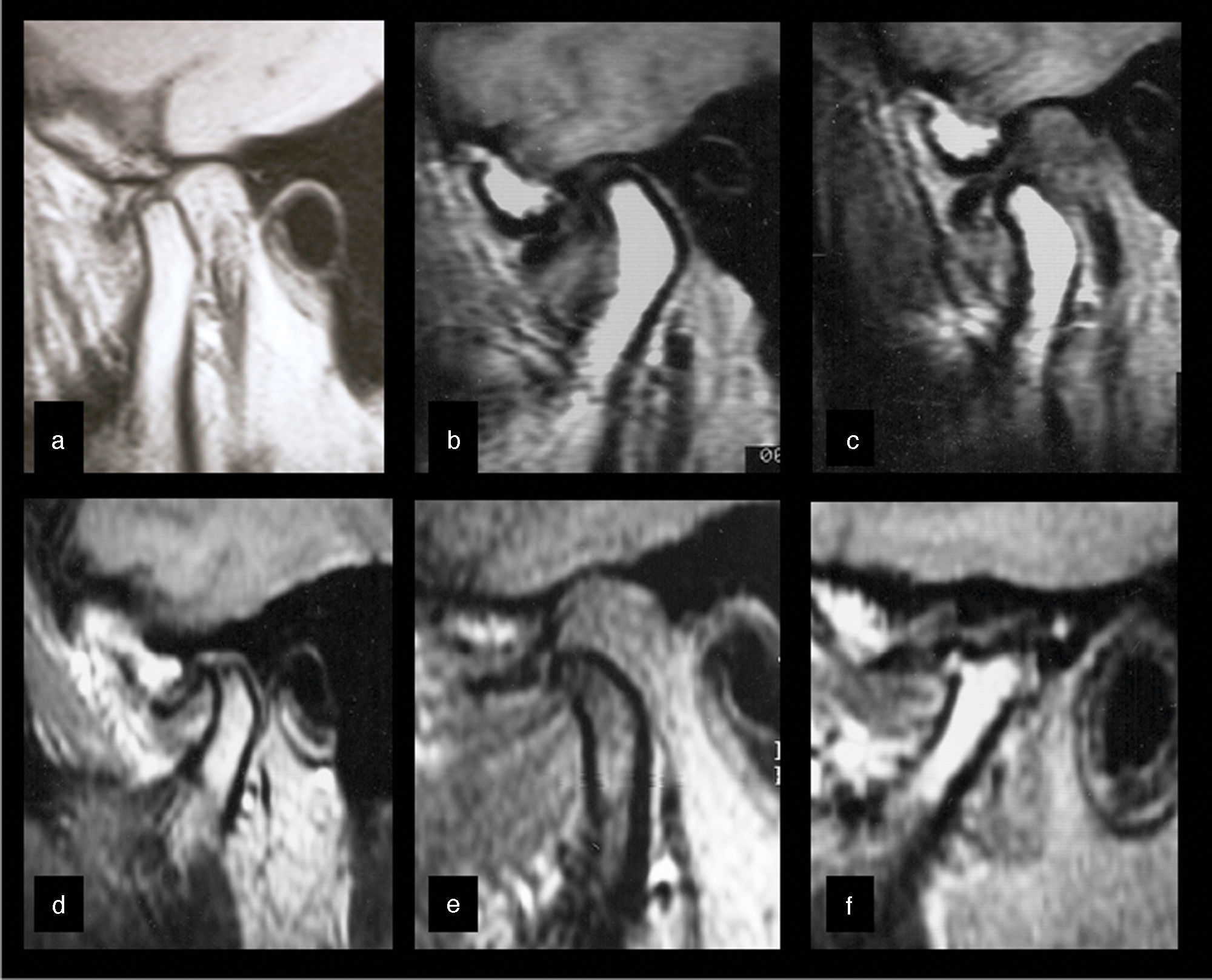
MRI has been the method of choice to study disease processes involving the TMJ soft tissues,2,20,23 such as the articular disc, ligaments, retrodiscal tissues, intracapsular synovial content, adjacent masticatory muscles, as well as cortical and medullary integrity of bone components.1,3,15,22
The technique allows three-dimensional analysis in the axial, coronal, and sagittal planes. It is considered the gold standard for assessing disc position and is highly sensitive for intraarticular degenerative alterations.3,20,23
The clinical conditions that suggest its use include persistent symptoms of joint or pre-auricular pain, presence of clicking and crepitation noises, functional alterations such as lateral projections of the condyle during mouth opening, frequent subluxations and dislocations, limited mouth opening movement with terminal stiffness, suspected neoplastic processes, and presence of osteoarthritic symptoms or asymptomatic osteoarthrosis.1,2,13,15
This diagnostic test protocols usually include the recording in the MHI and MMO position, using weighted T1, T2, and proton density (PD), in the sagittal and coronal planes.15 With T1-weighted images, it is possible to obtain excellent anatomic detail; proton density results in satisfactory spatial resolution of joint disc injuries, and is an excellent choice for the evaluation of medial and lateral disc displacements.20 T2-weighted images record the presence of joint effusion and medullary bone edema.2,3,20
The main advantages include detecting soft tissue alterations, necrosis, edema, presence or absence of invasion, and lack of exposure to ionizing radiation.2,3,15,16,20
MRI is also indicated for the assessment of the integrity and anatomical relation of neural structures, which, when compressed by tumor or vascular processes, can produce orofacial pain by demyelination and deafferentation.2,3,13,14,16
Its disadvantages are related to the high cost and the need for sophisticated facilities. It is contraindicated in claustrophobic patients, those with pacemakers and metallic heart valves, ferromagnetic foreign bodies, and pregnant women.14,15,23
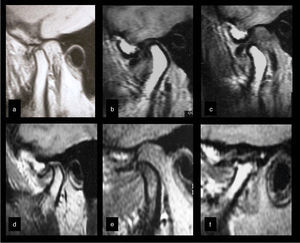
Fig. 3 illustrates morphological joint disc and bone structures alterations diagnosed by MRI.
Different MRI assessments disclosing previous joint disc displacement, with no reduction in the parasagittal views. One can observe compressive deformation of the joint disc in (a), also during dynamic comparison of the mandibular condylar movement in (b) and (c). Osteophytic formations (d–f), subchondral cyst (d), and severe change in form (f) define the diagnosis of osteoarthritis degenerative alterations in bone components. The presence of hyperintense T2-weighted images defines the diagnosis of effusion in (b–f).
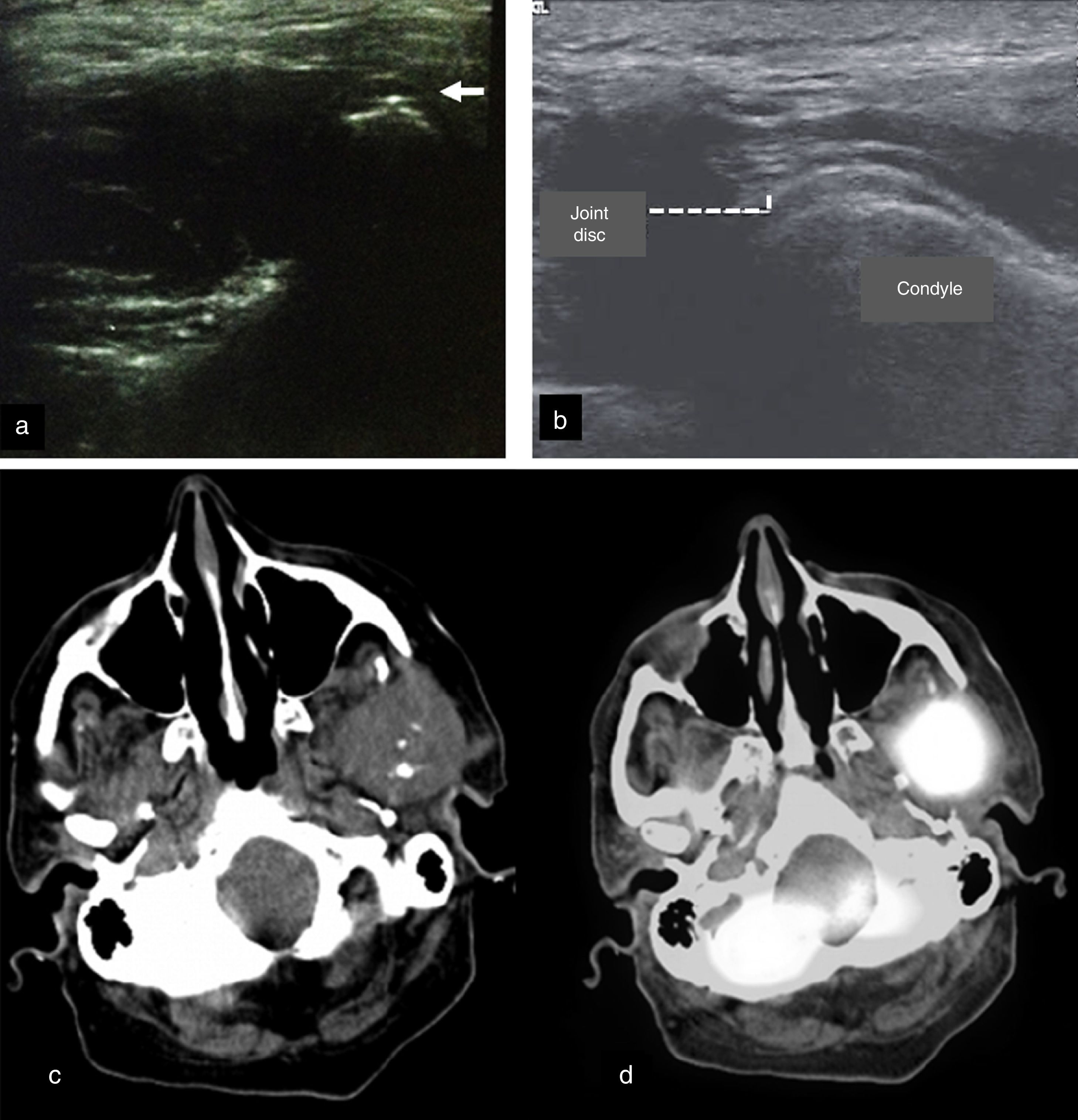
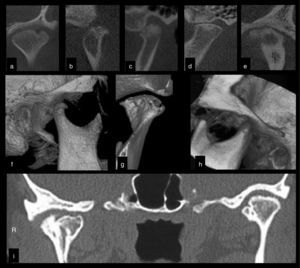
The use of US examination, especially by high-resolution imaging equipment, can be a useful option in the assessment of disc position in internal TMJ disorders.4,23 Although it has considerable diagnostic sensitivity, it has insufficient specificity to identify osteoarthrosis. The findings related to morphological alterations show that the method still does not have accuracy for the cortical and articular disc morphological diagnosis.24 However, the method is able to identify effusion in patients with inflammatory condition associated with pain, verified by MRI.23,24
Even with limitations, it can become a useful option for the initial study of the internal dysfunctions of the TMJ,15,23 particularly in patients with contraindications to MRI.14 Moreover, it is less expensive, allows real-time visualization without the use of ionizing radiation, and is quick and comfortable.4,23,24
US assessment is commonly used in the differential diagnosis of glandular and adjacent structures alterations, such as the TMJ and the masseter muscle. The symptoms present in cases of sialadenitis and sialolithiasis can be mistaken for Eagle syndrome, TMD, myofascial pain, nerve pain, and other orofacial pain conditions.
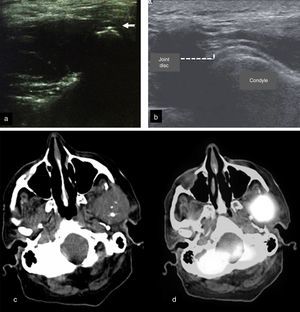
Another indication of the US assessment is the correct location of joint spaces for infiltrative therapies, arthrocentesis, and viscosupplementation (Fig. 4a and b). It shows, dynamically and in realtime, the location of joint components, providing adequate lubrication and washing, which are verified by the increase in joint space after treatment.25
Other imaging techniques. (a) Ultrasound examination of the TMJ25 used during the arthrocentesis assessment. Note the arthrocentesis needle as a hyperechoic point (white arrow). (b) Ultrasound examination of the TMJ showing the joint disc and condyle. (c) Tomographic axial view28 showing mass of soft tissue growth in the left TMJ region extending to the ipsilateral pterygoid region. Infra-temporal space with absence of condylar process, the presence of hyperdense areas, swelling, and asymmetry. (d) PET/CT assessment in axial view28 showing high metabolic activity in the left TMJ region. Images reproduced with permission of the authors’ copyrights25,28 by Elsevier.
Nuclear medicine facilitates establishing a diagnosis by detecting minute concentrations of radioactive pharmacological substances that determine osteometabolic alterations expressed in imaging exams.26
Bone scintigraphy is indicated to define neoplastic activity, metabolic disorders, and bone growth,14,26,27 as well as to evaluate synovitis and osteoarthritis.18 It is an examination with considerable sensitivity, low invasiveness, and high organ specificity, with low levels of radiation.27 It has some advantages over radiographies, conventional CT, and MRI because it provides an estimate of metabolic and inflammatory activity.26,27 It can facilitate an early diagnosis and is less costly than CT and MRI. However, it does not differentiate among bone scar disorders, infections, osteoarthritic manifestations, or tumors.15
Positron-emission tomography (PET) is usually indicated for the assessment and staging of metastatic tumors. It is able to provide accurate functional, morphological, and metabolic information.28 Three-dimensional images facilitate anatomical visualization and can significantly reduce the time required for diagnosis, in addition to properly direct treatments by ensuring that the therapies are appropriate.15
Currently, single photon emission computed tomography with technetium-99m methylene diphosphate (SPECT/CT with 99m Tc-MDP) is largely employed.26 This technology allows for multiplane image acquisition and 3-D display. The radiotracer 99m Tc is able to reflect the local osteometabolic rate, while the anatomic mapping is obtained by tomographic technique.26 As in the PET, anatomical and functional data are fused into a single image28 (Fig. 4c and d). Its main advantage is its sensitivity and specificity.26,28
Nuclear medicine examinations differ by the radiotracers/radioisotopes used, image capture technique, radiation dose, sensitivity, and presentation of results.15
Imaging test indication criteria in the diagnosis of temporomandibular joint disordersOne of the failures in diagnosis and treatment planning is an incorrect or unnecessary selection of unsuitable diagnostic tests. This occurs because of a lack of knowledge on the part of the professionals regarding the indications of the applicable tests.29
The correct indication of an imaging study should be based on the patient's need for legal documentation, his/her individual complaints, and the identified clinical signs and symptoms obtained during history-taking and physical examination.15,29,30 The basic principle that should guide the professional is that supplementary tests are only indicated when the clinical assessment is not sufficient to arrive at a diagnosis and devise a treatment plan.21
For TMJD, the physical examinations of palpation, measurement of movement, functional testing and evaluation of joint noises are instruments of great diagnostic validity when performed by trained and experienced professionals.6 However, the overlapping of muscle and joint symptoms can impair diagnostic accuracy, as both conditions show functional impairment. In this case and in cases of non-specific symptoms (from, for example, inflammation, neoplasia, and trauma), complementary imaging tests are essential for diagnostic clarification and delineation of the appropriate therapy.2,6
Imaging tests, from the simplest to the most complex, have varying degrees of sensitivity and specificity, properties that give them their diagnostic power.31
In general, MRI and CT are methods with higher accuracy when compared to conventional radiology, due to the higher anatomical resolution they provide. CT is considered the gold standard for the assessment of boney structures and the method of choice for facial trauma, whereas MRI is similarly regarded for the study of soft tissues.1,2,16,23,29 The two methods often complement each other in the study of TMJ alterations, constituting important tools for muscle and joint differential diagnosis.4 Although able to diagnose all bone alterations of the TMJ, MRI is considered limited when compared to the high accuracy of CT for hard tissue.19,22
However, low-technical-complexity tests may possess high diagnostic accuracy,18 as in the case of radiographic records of condylar hyperexcursion in patients with the clinical presentation of terminal joint clicking. These characteristics suggest a diagnosis of joint hypermobility, verified by a simple transcranial or planigraphy image.3 In this example, the image has great sensitivity, while clinical data confer specificity, ruling out other diagnostic possibilities.
Similarly, morphological alterations of the styloid, coronoid, and condylar processes can be evaluated with high diagnostic accuracy through low-cost and easy-to-perform radiographic examinations, such as planigraphy and panoramic X-rays,29 even though the CT is the gold standard for assessment of these alterations.2
The decision in choosing the examination must consider its influence on the proposed diagnosis and therapy. If the clinical indication is a conservative therapy that can control symptoms in the short term, image requests can be considered.1,15 Moreover, when conservative therapy has failed and an invasive therapy is indicated, highly sensitive diagnostic tests, such as CT and MRI are selected.15,31
Elaborate treatment plans also require complete and accurate images,29,31 for example, suspected fractures, where the CT, in addition to establishing the diagnosis, illustrates the exact location and size, and allows for the selection of the appropriate surgical therapy.2
Similar reasoning is used for the assessment of neoplastic conditions. A study32 that compared the accuracy of imaging tests for bone tumor detection showed that the nuclear medicine diagnostic tests had greater sensitivity and specificity than CT scans, MRI, and radiographic assessment, although the latter are useful in the initial clinical investigations.26,28,29,32
Especially for non-surgical joint conditions, one should consider the risk of injuries and the safety of diagnostic techniques.15 Although arthrography can effectively determine disc position and perforation,33 it is considered an invasive and potentially hazardous method. Thus, MRI has become the method of choice for such conditions.1
Similarly, recent studies4,5,23–25,30 have recommended US as a safe, noninvasive diagnostic technique with considerable accuracy for joint disc positioning, especially for patients with contraindication to MRI or submitted to real-time interventions, such as arthrocentesis and viscosupplementation. In these techniques, the US examination is especially appropriate for the identification of the inferior joint space. Its precise identification and correct access are factors that contribute to the technique's success.11
Long-term risks and tissue damage should also be considered for radiation exposure. As in conventional radiographs, CT should only cautiously be chosen because of its higher radiation absorption,15,29 although CBCT has shorter radiation exposure time when compared to helical CT.21
Even if they pose some risk, tests that use higher doses of radiation are needed for disease staging and are essential for defining the treatment plan. Nuclear medicine examinations, for instance, are indicated to assess metabolic alterations of growth and assessment of metastases.26–28 However, they still require confirmation of the type of growth through specific tests, such as histopathological or immunohistochemical analysis.15
Table 2 lists and classifies information that can be obtained by several examination techniques through TMJ images, based on their indications, risks, and diagnostic power.
Indication of imaging tests to diagnose joint TMD and alterations in structures adjacent to the stomatognathic system.
| Disorders | Assessed sign | Panoramic1,3,13,14,16,18,29 | Transcranial1,3,13,14,16–18,29 | Planigraphy1,3,13,14,16,18,29 | Arthrography1,3,13,14,16–18,20,29 |
|---|---|---|---|---|---|
| Congenital and developmental | |||||
| Aplasia | Absence of structure | b | c | c | a |
| Hypoplasia | Dimensional reduction | b | c | c | a |
| Hyperplasia | Dimensional increase | b | c | c | a |
| Dysplasia | Structural alteration | b | c | c | a |
| Acquired | |||||
| Neoplasias | Bone formation/destruction | b | c | c | a |
| Soft tissue growth | – | – | – | – | |
| Metastasis | a | a | a | – | |
| Disc derangement | |||||
| With reduction | Recapture in MMO | – | – | – | c |
| Without reduction | No recapture in MMO | – | – | – | c |
| TMJ displacement | Open locking, clinical diagnosis | a | c | c | a |
| Inflammatory disorders | |||||
| Synovitis/capsulitis | Effusion, inflammation, capsular edema | – | – | – | – |
| Polyarthritis | Polyarticular, cortical alteration, remodeling | b | b | b | a |
| Non-inflammatory disorders/primary or secondary osteoarthritis | Uni-/bilateral, cortical alteration, remodeling | b | b | b | a |
| Ankylosis | Bone formation, impaired excursion | c | c | c | b |
| Fracture (condylar process) | Asymmetry, fracture line | c | b | c | b |
| Odontogenic conditions | Cists, tumors, periapical disease | c | – | – | – |
| Of the styloid process | Elongation calcification | c | – | c | – |
| Of the major salivary glands | Sialolithiasis, inflammation | a | – | – | – |
| Of the condylar excursion (hypo/hyper) | Condylar x mandibular tubercle ratio in MMO | – | c | c | b |
| Of the joint disc form | TMJ disc form alteration and perforation | – | – | – | d |
| Of the adjacent bone structures | Alterations in coronoid and mastoid processes | c | – | c | – |
| Of adjacent soft tissues | Alterations in the ligaments, retrodiscal area, masticatory muscles | – | – | – | – |
| Disorders | Assessed sign | CT1,15,16,18,21–23,29,32 | MRI1–3,12,14,15,19,20,24,29,31–33 | US4,5,15,23–25,30,33 | Nuclear medicine 13,14,26,28 |
|---|---|---|---|---|---|
| Congenital and developmental | |||||
| Aplasia | Absence of structure | d | c | a | a |
| Hypoplasia | Dimensional reduction | d | c | a | a |
| Hyperplasia | Dimensional increase | d | c | a | a |
| Dysplasia | Structural alteration | d | c | a | a |
| Acquired | |||||
| Neoplasias | Bone formation/destruction | d | d | a | d |
| Soft tissue growth | a | d | c | d | |
| Metastasis | c | c | a | d | |
| Disc derangement | |||||
| With reduction | Recapture in MMO | – | d | c | – |
| Without reduction | No recapture in MMO | – | d | c | – |
| TMJ displacement | Open locking, clinical diagnosis | d | c | a | – |
| Inflammatory disorders | |||||
| Synovitis/capsulitis | Effusion, inflammation, capsular edema | – | d | c | a |
| Polyarthritis | Polyarticular, cortical alteration, remodeling | d | c | – | a |
| Non-inflammatory disorders/primary or secondary osteoarthritis | Uni-/bilateral, cortical alteration, remodeling | d | c | – | a |
| Ankylosis | Bone formation, impaired excursion | d | c | – | – |
| Fracture (condylar process) | Asymmetry, fracture line | d | c | – | – |
| Odontogenic conditions | Cists, tumors, periapical disease | d | a | a | c |
| Of the styloid process | Elongation calcification | d | b | – | – |
| Of the major salivary glands | Sialolithiasis, inflammation | b | d | d | – |
| Of the condylar excursion (hypo/hyper) | Condylar x mandibular tubercle ratio in MMO | d | c | – | – |
| Of the joint disc form | TMJ disc form alteration and perforation | – | c | – | – |
| Of the adjacent bone structures | Alterations in coronoid and mastoid processes | d | b | – | b |
| Of adjacent soft tissues | Alterations in the ligaments, retrodiscal area, masticatory muscles | – | d | c | a |
Individually, the several imaging tests have specific indications for the diagnosis of TMJD.
Despite their lower sensitivity, radiographic techniques have lower cost and employ lower radiation doses. They are indicated for the early assessment of less complex symptoms and the differential diagnosis between TMD and inflammatory dental-maxillofacial conditions.
Morphological, degenerative bone abnormalities, and fractures are precisely diagnosed, identified, and measured by CT. Mainly, CBCT has a lower radiation dose and artifact reduction, and is considered the gold standard for the assessment of maxillofacial hard tissues. Inflammatory alterations, joint disc position, and other soft tissue structures are clearly identified and evaluated by MRI, that is safer than arthrography.
US examination accurately identifies the joint disc, mainly when the MRI assessment is contraindicated. It is indicated for the differential diagnosis between TMD and painful conditions of major salivary glands, as well as pre- and post-evaluation of infiltration therapies, such as viscosupplementation and arthrocentesis.
Nuclear medicine assessments are primarily indicated for the assessment of metabolic and growth alterations, such as tumors and metastases.
Arthrography is an invasive intra-articular examination; its usual indication is the visualization of joint disc alterations. Due to the risk inherent to the technique, it has been replaced by MRI assessment.
Factors that need to be evaluated for the selection of TMJ imaging tests include the following: the need to determine the presence of the disease and its prognosis, the quality and quantity of available clinical information; uncertainty in the differential diagnosis; determining the stage of disease development; need for legal documentation; preoperative preparation; evaluation of treatment evolution; and the safety and accuracy of the proposed examination.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Ferreira LA, Grossmann E, Januzzi E, de Paula MVQ, Carvalho ACP. Diagnosis of temporomandibular joint disorders: indication of imaging exams. Braz J Otorhinolaryngol. 2016;82:341–52.