Mouth breathing leads to negative consequences on quality of life, especially in school-age children.
ObjectiveTo determine whether the breathing pattern influences children's learning process.
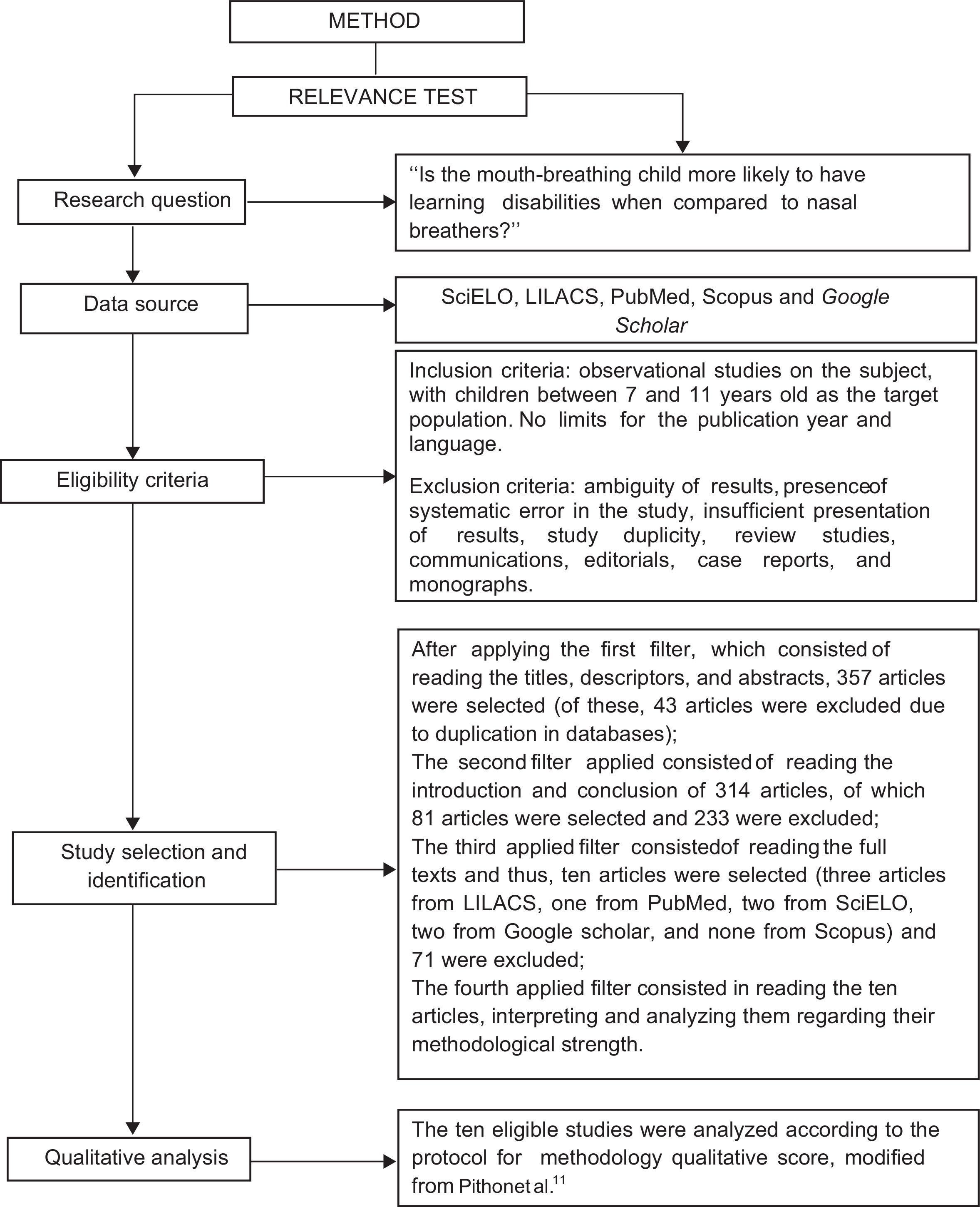
MethodsThis systematic review was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) instructions, with no restrictions regarding the year of publication and language, created based on the clinical question formulation according to the Problem/Patient/Population, Intervention/Indicator, Comparison, Outcome (PICO) strategy: “Is the mouth-breathing child more likely to have learning disabilities when compared to nasal breathers?” in the SciELO, PubMed, LILACS, and Scopus electronic databases. Google Scholar was used to search the gray literature. The keywords “learning,” “mouth breathing,” and their equivalent terms in Portuguese were used in an integrated manner. The studies included in the review were observational, conducted with schoolchildren aged 7–11 years. Afterwards, the studies were evaluated regarding their methodological quality. The research was performed by two eligible reviewers.
ResultsA total of 357 records were obtained, of which 43 records were duplicate. After applying the eligibility criteria, ten articles were included in the research scope. Half of the studies used a control group and otorhinolaryngological assessment, whereas a minority used validated (20%) and sample calculation protocols (10%). The evaluation procedures were varied. Overall, 80% of the articles showed a higher incidence of learning disabilities among mouth breathers.
ConclusionThis systematic review has shown that mouth breathers are more likely to have learning difficulties than nasal breathers.
A respiração oral traz consequências negativas para a qualidade de vida das pessoas, principalmente para escolares.
ObjetivoVerificar se o modo respiratório influencia no processo de aprendizagem infantil.
MétodoEsta revisão sistemática foi realizada seguindo as instruções PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses), sem restrição quanto ao ano de publicação e idioma, elaborada a partir da formulação de questão clínica elaborada pela estratégia P.I.C.O.: “A criança respiradora oral tem mais chances de apresentar dificuldades de aprendizagem quando comparada à respiradora nasal?”, nas bases de dados eletrônicas SciELO, PubMed, LILACS e Scopus. Foi utilizado o Google Scholar para pesquisa da literatura cinza. As palavras-chave “aprendizagem”, “respiração bucal”, “learning” e “mouth breathing” foram utilizadas de forma integrada. Os estudos incluídos foram observacionais, realizados com escolares entre sete e onze anos. Em seguida, os estudos foram avaliados quanto à sua qualidade metodológica. Toda a pesquisa foi realizada por dois revisores de elegibilidade.
ResultadosForam obtidos 357 registros, sendo 314 blindados (43 registros em duplicidade). Após os critérios de elegibilidade, dez artigos integraram o escopo desta pesquisa. Metade dos estudos usou grupo controle e fez uso de avaliação otorrinolaringológica, a minoria fez uso de protocolos validados (20%) e de cálculo amostral (10%). Os procedimentos de avaliação foram variados. De forma geral, 80% dos artigos evidenciaram maior ocorrência de distúrbio de aprendizagem em respiradores orais.
ConclusãoEsta revisão sistemática demonstrou que indivíduos com respiração oral apresentam maior tendência de dificuldades na aprendizagem do que os nasais.
Learning disorders may occur due to multifactorial reasons, among which are auditory information processing alterations,1,2 attention deficit, interpersonal relationship difficulties, behavioral disorders, cognitive deficits, disadvantaged socioeconomic background,3 family history of learning difficulties and disabilities,4 as well as others, such as mouth breathing – which can compromise learning.5
When breathing is performed only through the mouth, it can be considered a pathological adaptation resulting from difficulty of breathing through the nose,6 and it results in the inspiration of a drier, unfiltered air, at a colder or warmer temperature than the expected, which ultimately overwhelms the tonsils and the larynx and can cause chronic inflammation. If such pathological adaptation occurs over a long period, it can result in tonsillar hypertrophy and subsequently, varying degrees of upper airway obstruction. Thus, there will be resistance to gas flow, permanent increase in energy expenditure, and adaptations that are structural (high-arched palate and dental malocclusion) and functional (orofacial muscle flaccidity, dysphonia, and sleep apnea, for instance), that can impair the quality of sleep, mood, behavior, and school performance,7 although there is no significant scientific evidence to support the association between the altered breathing pattern and learning difficulties.
Considering the high prevalence of mouth breathing in childhood8 and the possibility of its impact on learning, this study was designed in order to verify, through a systematic review of the literature, whether this breathing pattern influences children's learning process.
MethodsThe methodological approach used in this review follows, including article search strategy and eligibility criteria, the data collection phase, and analysis. This systematic review was carried out following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.9
Search strategy and eligibility criteriaThis systematic review study was conducted with no restrictions regarding the year and language of publication. The P.I.C.O strategy was used, considering schoolchildren who were mouth breathers aged 7–11 years (P=patient), assessed regarding the aspects related to learning (I=intervention) and compared with schoolchildren who were nasal breathers (C=intervention comparison or control), aiming at verifying the possibility of learning disability in those with altered breathing pattern (O=outcome), using the following guiding question: “Is the mouth-breathing child more likely to have learning disabilities when compared to nasal breathers?”.
The study design is explained in Fig. 1, with the study eligibility criteria. For the studies considered preliminarily eligible, the full text was obtained and assessed in order to verify whether they met all the inclusion criteria. The following inclusion criteria were used: observational studies (controlled, cross-sectional, prospective, or retrospective longitudinal studies) on the subject, with schoolchildren aged between 7 and 11 years.
The exclusion criteria were: ambiguous results, poor presentation of results, study duplication based on the database search, review studies, communications, case reports, scientific meeting abstracts, monographs, comments, or editorials. Studies regarding syndromic patients and those with intellectual disabilities were also excluded, as well as registries not directly related to the final outcome of this study (Fig. 1).
The keywords were selected in DeCS (VHL Health Sciences Descriptors) and MeSH (PubMed), in order to identify relevant studies in the PubMed, SciELO, LILACS, and Scopus electronic databases. The controlled descriptors were “learning” and “mouth breathing,” “aprendizagem” and “respiração bucal.” Boolean operators (OR and AND) were used for descriptor combination. This research was carried out on July 15th, 2015. The gray literature was identified by searching in Google Scholar, by consulting the first hundred records of each combination.
Assessment process validity and data extractionAfter obtaining the list of the studies carried out with the chosen descriptors, the relevance test was applied and each study was carefully analyzed by two eligibility reviewers (not blinded to the authors and journals), who performed the survey independently and decided, by consensus, which studies would be selected. In case of divergence of results, a third reviewer was consulted to resolve the question regarding whether the study should be included, as suggested by the literature.10
Initially, article titles, descriptors, and abstracts were identified; the first research filter was applied to select them. Subsequently, based on the obtained results, the second filter was applied by reading the study introduction and conclusion. If the article was considered eligible, the article was read in full and, thus, the third filter was applied.
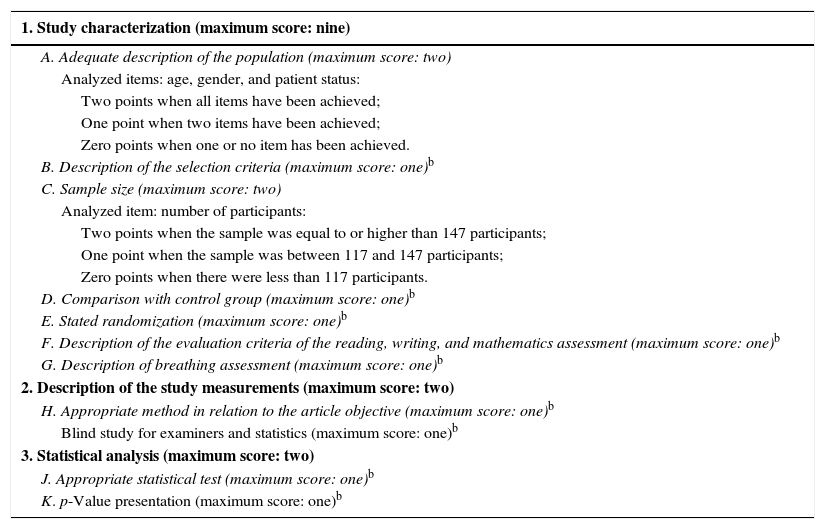
In this preliminary phase, the eligible texts were assessed for their methodological strength, representing the fourth and final relevance test filter used. The methodology qualitative score protocol, modified from Pithon et al., was used for this evaluation11; it allows a maximum score of 13 points (Table 1). At this time, the review was blinded to the authors and journals, to avoid any selection bias and possible conflicts of interest.
| 1. Study characterization (maximum score: nine) |
|---|
| A. Adequate description of the population (maximum score: two) |
| Analyzed items: age, gender, and patient status: |
| Two points when all items have been achieved; |
| One point when two items have been achieved; |
| Zero points when one or no item has been achieved. |
| B. Description of the selection criteria (maximum score: one)b |
| C. Sample size (maximum score: two) |
| Analyzed item: number of participants: |
| Two points when the sample was equal to or higher than 147 participants; |
| One point when the sample was between 117 and 147 participants; |
| Zero points when there were less than 117 participants. |
| D. Comparison with control group (maximum score: one)b |
| E. Stated randomization (maximum score: one)b |
| F. Description of the evaluation criteria of the reading, writing, and mathematics assessment (maximum score: one)b |
| G. Description of breathing assessment (maximum score: one)b |
| 2. Description of the study measurements (maximum score: two) |
| H. Appropriate method in relation to the article objective (maximum score: one)b |
| Blind study for examiners and statistics (maximum score: one)b |
| 3. Statistical analysis (maximum score: two) |
| J. Appropriate statistical test (maximum score: one)b |
| K. p-Value presentation (maximum score: one)b |
It should be noted that the adaptation occurred only when establishing the number of subjects that should participate in the studies (n), as a basis for the sample size calculation related to the study subject, using an “n” of 147 subjects based on the study by Menezes et al.,12 who used this number as the minimum one for performing a study with mouth breathers between the ages between 8 and 10 years old, i.e., within the mean age of the studies included in this research.
The studies were synthesized and distributed in a chart, containing the following information: year of publication, type of study, diagnosis and tools for data collection, sample characterization, main findings, and conclusion of the study, reported in the results session.
Data analysisData analysis was performed qualitatively, as the methods used in the studies were heterogeneous.
ResultsResearch strategy and methodological assessmentUsing the keywords “respiração bucal” AND “aprendizagem,” seven articles from the LILACS database were obtained, 2440 articles from the Google Scholar database (of these, the first hundred were analyzed), six articles from Scopus, and one from SciELO. Using the keywords “mouth breathing” AND “learning,” eight articles from LILACS, 147,000 from Google Scholar (of these, the first hundred were analyzed), five from SciELO, and 30 from the PubMed database were obtained. Thus, the initial sample comprised 357 articles.
After applying the filters designed in the method, 43 articles were excluded after the first filter was applied due to duplication in the databases and 304 for addressing other subjects such as prevalence, behavioral assessment, posture, hearing skills, malocclusion, adult studies, and studies in animals and treatment (233 after the second filter and 71 after the third), as shown in Fig. 1. Thus, the sample consisted of ten articles.
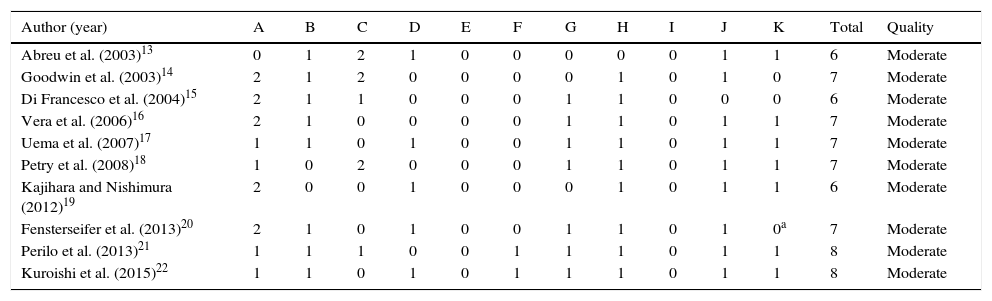
As for the methodological strength, all (100%) of the included studies13–22 showed moderate methodological strength (Table 2).
Scores obtained after applying the Methodology Qualitative Score Protocol, adapted from Pithon et al.11
| Author (year) | A | B | C | D | E | F | G | H | I | J | K | Total | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abreu et al. (2003)13 | 0 | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 6 | Moderate |
| Goodwin et al. (2003)14 | 2 | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 7 | Moderate |
| Di Francesco et al. (2004)15 | 2 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 6 | Moderate |
| Vera et al. (2006)16 | 2 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 | Moderate |
| Uema et al. (2007)17 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 | Moderate |
| Petry et al. (2008)18 | 1 | 0 | 2 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 | Moderate |
| Kajihara and Nishimura (2012)19 | 2 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 6 | Moderate |
| Fensterseifer et al. (2013)20 | 2 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0a | 7 | Moderate |
| Perilo et al. (2013)21 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 8 | Moderate |
| Kuroishi et al. (2015)22 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 8 | Moderate |
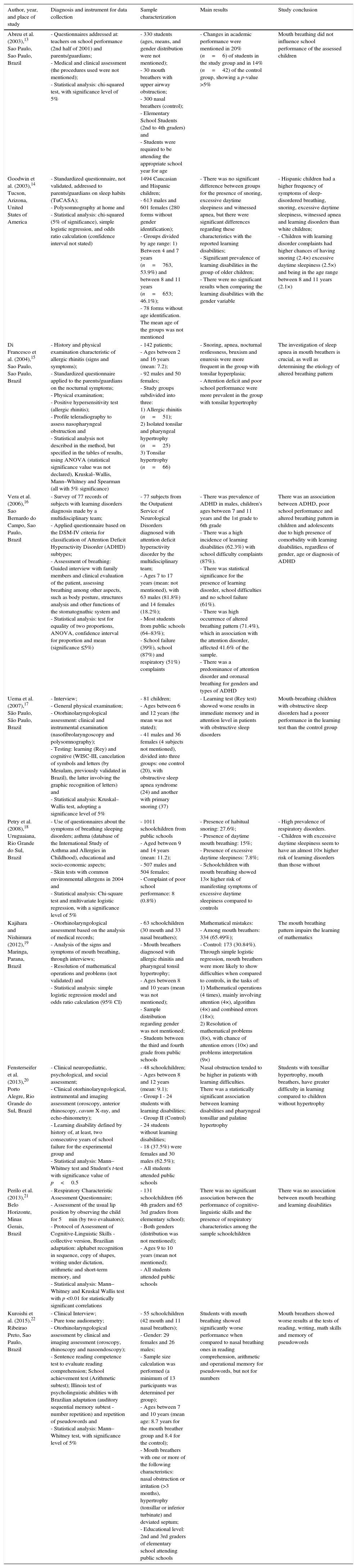
Of the ten included studies, half (50%) used a control group.13,17,19,20,22 The studies were published between 2003 and 2015, with peak concentrations in 2003 (two studies, 20%)13,14 and in 2013 (two studies, 20%).20,21 The use of sample size calculation was achieved in one study (10%).22Table 3 shows the main characteristics of the selected studies.
Summary of the ten articles that comprised the study sample on the subject “mouth breathing and learning”.
| Author, year, and place of study | Diagnosis and instrument for data collection | Sample characterization | Main results | Study conclusion |
|---|---|---|---|---|
| Abreu et al. (2003),13 Sao Paulo, Sao Paulo, Brazil | - Questionnaires addressed at: teachers on school performance (2nd half of 2001) and parents/guardians; - Medical and clinical assessment (the procedures used were not mentioned); - Statistical analysis: chi-squared test, with significance level of 5% | - 330 students (ages, means, and gender distribution were not mentioned); - 30 mouth breathers with upper airway obstruction; - 300 nasal breathers (control); - Elementary School Students (2nd to 4th graders) and - Students were required to be attending the appropriate school year for age | - Changes in academic performance were mentioned in 20% (n=6) of students in the study group and in 14% (n=42) of the control group, showing a p-value >5% | Mouth breathing did not influence school performance of the assessed children |
| Goodwin et al. (2003),14 Tucson, Arizona, United States of America | - Standardized questionnaire, not validated, addressed to parents/guardians on sleep habits (TuCASA); - Polysomnography at home and - Statistical analysis: chi-squared (5% of significance), simple logistic regression, and odds ratio calculation (confidence interval not stated) | 1494 Caucasian and Hispanic children; - 613 males and 601 females (280 forms without gender identification); - Groups divided by age range: 1) Between 4 and 7 years (n=763, 53.9%) and between 8 and 11 years (n=653; 46.1%); - 78 forms without age identification. The mean age of the groups was not mentioned | - There was no significant difference between groups for the presence of snoring, excessive daytime sleepiness and witnessed apnea, but there were significant differences regarding these characteristics with the reported learning disabilities; - Significant prevalence of learning disabilities in the group of older children; - There were no significant results when comparing the learning disabilities with the gender variable | - Hispanic children had a higher frequency of symptoms of sleep-disordered breathing, snoring, excessive daytime sleepiness, witnessed apnea and learning disorders than white children; - Children with learning disorder complaints had higher chances of having snoring (2.4×) excessive daytime sleepiness (2.5×) and being in the age range between 8 and 11 years (2.1×) |
| Di Francesco et al. (2004),15 Sao Paulo, Sao Paulo, Brazil | - History and physical examination characteristic of allergic rhinitis (signs and symptoms); - Standardized questionnaire applied to the parents/guardians on the nocturnal symptoms; - Physical examination; - Positive hypersensitivity test (allergic rhinitis); - Profile teleradiography to assess nasopharyngeal obstruction and - Statistical analysis not described in the method, but specified in the tables of results, using ANOVA (statistical significance value was not declared), Kruskal–Wallis, Mann–Whitney and Spearman (all with 5% significance) | - 142 patients; - Ages between 2 and 16 years (mean: 7.2); - 92 males and 50 females; - Study groups subdivided into three: 1) Allergic rhinitis (n=51); 2) Isolated tonsilar and pharyngeal hypertrophy (n=25) 3) Tonsilar hypertrophy (n=66) | - Snoring, apnea, nocturnal restlessness, bruxism and enuresis were more frequent in the group with tonsilar hyperplasia; - Attention deficit and poor school performance were more prevalent in the group with tonsilar hypertrophy | The investigation of sleep apnea in mouth breathers is crucial, as well as determining the etiology of altered breathing pattern |
| Vera et al. (2006),16 Sao Bernardo do Campo, Sao Paulo, Brazil | - Survey of 77 records of subjects with learning disorders diagnosis made by a multidisciplinary team; - Applied questionnaire based on the DSM-IV criteria for classification of Attention Deficit Hyperactivity Disorder (ADHD) subtypes; - Assessment of breathing: Guided interview with family members and clinical evaluation of the patient, assessing breathing among other aspects, such as body posture, structures analysis and other functions of the stomatognathic system and - Statistical analysis: test for equality of two proportions, ANOVA, confidence interval for proportion and mean (significance ≤5%) | - 77 subjects from the Outpatient Service of Neurological Disorders diagnosed with attention deficit hyperactivity disorder by the multidisciplinary team; - Ages 7 to 17 years (mean: not mentioned), with 63 males (81.8%) and 14 females (18.2%); - Most students from public schools (64–83%); - School failure (39%), school (87%) and respiratory (51%) complaints | - There was prevalence of ADHD in males, children's ages between 7 and 11 years and the 1st grade to 6th grade - There was a high incidence of learning disabilities (62.3%) with school difficulty complaints (87%). - There was statistical significance for the presence of learning disorder, school difficulties and no school failure (61%). - There was high occurrence of altered breathing pattern (71.4%), which in association with the attention disorder, affected 41.6% of the sample. - There was a predominance of attention disorder and oronasal breathing for genders and types of ADHD | There was an association between ADHD, poor school performance and altered breathing pattern in children and adolescents due to high presence of comorbidity with learning disabilities, regardless of gender, age or diagnosis of ADHD |
| Uema et al. (2007),17 São Paulo, São Paulo, Brazil | - Interview; - General physical examination; - Otorhinolaryngological assessment: clinical and instrumental examination (nasofibrolaryngoscopy and polysomnography); - Testing: learning (Rey) and cognitive (WISC-III, cancelation of symbols and letters (by Mesulam, previously validated in Brazil), the latter involving the graphic recognition of letters) and - Statistical analysis: Kruskal–Wallis test, adopting a significance level of 5% | - 81 children; - Ages between 6 and 12 years (the mean was not stated); - 41 males and 36 females (4 subjects not mentioned), divided into three groups: one control (20), with obstructive sleep apnea syndrome (24) and another with primary snoring (37) | - Learning test (Rey test) showed worse results in immediate memory and in attention level in patients with obstructive sleep disorders | Mouth-breathing children with obstructive sleep disorders had a poorer performance in the learning test than the control group |
| Petry et al. (2008),18 Uruguaiana, Rio Grande do Sul, Brazil | - Use of questionnaires about the symptoms of breathing sleeping disorders; asthma (database of the International Study of Asthma and Allergies in Childhood), educational and socio-economic aspects; - Skin tests with common environmental allergens in 2004 and - Statistical analysis: Chi-square test and multivariate logistic regression, with a significance level of 5% | - 1011 schoolchildren from public schools - Aged between 9 and 14 years (mean: 11.2); - 507 males and 504 females; - Complaint of poor school performance: 8 (0.8%) | - Presence of habitual snoring: 27.6%; - Presence of daytime mouth breathing: 15%; - Presence of excessive daytime sleepiness: 7.8%; - Schoolchildren with mouth breathing showed 13× higher risk of manifesting symptoms of excessive daytime sleepiness compared to controls | - High prevalence of respiratory disorders. - Children with excessive daytime sleepiness seem to have an almost 10× higher risk of learning disorders than those without |
| Kajihara and Nishimura (2012),19 Maringa, Parana, Brazil | - Otorhinolaryngological assessment based on the analysis of medical records; - Analysis of the signs and symptoms of mouth breathing, through interviews; - Resolution of mathematical operations and problems (not validated) and - Statistical analysis: simple logistic regression model and odds ratio calculation (95% CI) | - 63 schoolchildren (30 mouth and 33 nasal breathers); - Mouth breathers diagnosed with allergic rhinitis and pharyngeal tonsil hypertrophy; - Ages between 8 and 10 years (mean was not mentioned); - Sample distribution regarding gender was not mentioned; - Students between the third and fourth grade from public schools | Mathematical mistakes: - Among mouth breathers: 334 (65.49%); - Control: 173 (30.84%). Through simple logistic regression, mouth breathers were more likely to show difficulties when compared to controls, in the tasks of: 1) Mathematical operations (4 times), mainly involving attention (4×), algorithm (4×) and combined errors (18×); 2) Resolution of mathematical problems (8×), with chance of attention errors (10×) and problems interpretation (9×) | The mouth breathing pattern impairs the learning of mathematics |
| Fensterseifer et al. (2013),20 Porto Alegre, Rio Grande do Sul, Brazil | - Clinical neuropediatric, psychological, and social assessment; - Clinical otorhinolaryngological, instrumental and imaging assessment (oroscopy, anterior rhinoscopy, cavum X-ray, and echo-rhinometry); - Learning disability defined by history of, at least, two consecutive years of school failure for the experimental group and - Statistical analysis: Mann–Whitney test and Student's t-test with significance value of p<0.5 | - 48 schoolchildren; - Ages between 8 and 12 years (mean: 9.1); - Group I - 24 students with learning disabilities; - Group II (Control) - 24 students without learning disabilities; - 18 (37.5%) were females and 30 males (62.5%); - All students attended public schools | Nasal obstruction tended to be higher in patients with learning difficulties. There was a statistically significant association between learning disabilities and pharyngeal tonsillar and palatine hypertrophy | Students with tonsillar hypertrophy, mouth breathers, have greater difficulty in learning compared to children without hypertrophy |
| Perilo et al. (2013),21 Belo Horizonte, Minas Gerais, Brazil | - Respiratory Characteristic Assessment Questionnaire; - Assessment of the usual lip position by observing the child for 5min (by two evaluators); - Protocol of Assessment of Cognitive-Linguistic Skills - collective version, Brazilian adaptation: alphabet recognition in sequence, copy of shapes, writing under dictation, arithmetic and short-term memory, and - Statistical analysis: Mann–Whitney and Kruskal Wallis test with p <0.01 for statistically significant correlations | - 131 schoolchildren (66 4th graders and 65 3rd graders from elementary school); - Both genders (distribution was not mentioned); - Ages 9 to 10 years (mean not mentioned); - All students attended public schools | There was no significant association between the performance of cognitive-linguistic skills and the presence of respiratory characteristics among the sample schoolchildren | There was no association between mouth breathing and learning disabilities |
| Kuroishi et al. (2015),22 Ribeirao Preto, Sao Paulo, Brazil | - Clinical Interview; - Pure tone audiometry; - Otorhinolaryngological assessment by clinical and imaging assessment (oroscopy, rhinoscopy and nasoendoscopy); - Sentence reading competence test to evaluate reading comprehension; School achievement test (Arithmetic subtest); Illinois test of psycholinguistic abilities with Brazilian adaptation (auditory sequential memory subtest - number repetition) and repetition of pseudowords and - Statistical analysis: Mann–Whitney test, with significance level of 5% | - 55 schoolchildren (42 mouth and 11 nasal breathers); - Gender: 29 females and 26 males; - Sample size calculation was performed (a minimum of 13 participants was determined per group); - Ages between 7 and 10 years (mean age: 8.7 years for the mouth breather group and 8.4 for the control); - Mouth breathers with one or more of the following characteristics: nasal obstruction or irritation (>3 months), hypertrophy (tonsillar or inferior turbinate) and deviated septum; - Educational level: 2nd and 3rd graders of elementary school attending public schools | Students with mouth breathing showed significantly worse performance when compared to nasal breathing ones in reading comprehension, arithmetic and operational memory for pseudowords, but not for numbers | Mouth breathers showed worse results at the tests of reading, writing, math skills and memory of pseudowords |
The age of the samples ranged between 2 and 16 years, with a mean of 9.28 years. Regarding gender (from the studies that reported it), most subjects were males (52.28%).
The procedures used for the assessment of the participants were: analysis of records/files: two (20%)16,20; interview: four (40%)16,17,19,22; questionnaires: six (60%)13–16,18,21; clinical evaluation or observation: six (60%)13,15–17,20,21; otorhinolaryngological assessment disclosing mouth breathing: five (50%),15,17,19,20,22 specific tests: six (60%)15,17–19,21,22; and pure tone audiometry: two (20%).17,22
Regarding the data collection tools, the use of validated protocols was attained in two studies17,22 (20% of the sample) and Uema et al.17 used, among several tests, a grapheme recognition task, through the letter cancelation test, while Kuroishi et al.22 used the Academic Performance Test, in partial form.
Mouth breathers showed greater difficulty in solving mathematical operations than nasal breathers.19,22 However, some researchers21 found no difficulty regarding mathematical operations in their study.
Reading comprehension was considered worse in the mouth breathers,22 as well as writing.21
Overall, eight studies (80%)14–20,22 reported learning disabilities in mouth breathers, with three (30%) related to tonsillar or inferior turbinate hypertrophy,15,19,22 three (30%) due to sleep-disordered breathing,14,17,18 two (20%) to nasal obstruction20,22 and allergic rhinitis (20%),15,19 one (10%) associated with attention deficit hyperactivity disorder (ADHD),16 one (10%) due to asthma,18 and one (10%) to septal deviation.22 Of the studies that found no association between mouth breathing and learning disability (n=2; 20%),13,21 one was related to nasal obstruction13 and another21 did not divide the groups between mouth and nasal breathers, classifying the participants as having respiratory impairment features, without specifying the cause.
DiscussionSchool failures occur for different reasons; according to the last census, conducted by Instituto Nacional de Estudos e Pesquisas Educacionais Anísio Teixeira23 (INEP, BRASIL, 2013), in 2013, 6.1% of students fail to pass on to the following grade, with one of the reasons being the presence of learning disabilities. Literature has described several factors for its emergence, such as hearing,1,2 attention, interpersonal relationships, behavior and cognition disabilities, socioeconomic status,3 family history,4 as well as mouth breathing.5
This respiratory pattern is considered a pathological adaptation6, which can affect the quality of sleep, mood, behavior, and school performance7; however, there are few studies that show such interrelation. Moreover, the prevalence of mouth breathing is considered high in childhood8 and, thus, the present systematic review was carried out.
As shown by the sample composition, little has been investigated on the subject (2.8% of 357 studies), demonstrating the need for further studies in this area.
Half of the studies in the sample used a control group,13,17,19,20,22 and it is noteworthy that Kajihara and Nishimura19 compared their results with the control group of another study, although they belonged to the same research group. Thus, it is suggested that studies on the subject with control groups be performed to attain greater result reliability. Additionally, for evidence-based practice, that is, for a professional decision to be made based on the obtained scientific results, according to Muir Gray24 it is ideal when such studies show high evidence strength, which are usually controlled and randomized studies; such randomized controlled studies were not identified in our sample.
As for the nosological diagnosis confirming the etiology of mouth breathing, half of the researchers we studied15,17,19,20,22 submitted their sample groups to otorhinolaryngological assessment, demonstrating obstructive mouth breathing, although with different etiologies. It should also be noted that Abreu et al.13 stated that the study group underwent medical assessment, but did not mention which specialty performed such assessment or what procedures were performed.
Perilo et al.21 sent a Questionnaire for Assessment of Respiratory Characteristics, consisting of 22 closed questions with yes/no answers to the parents/guardians. However, the authors’ study, due to the absence of the otorhinolaryngological evaluation to confirm the etiology of the altered breathing pattern, did not mention the number of affirmative questions that should have been marked in order to consider the subject a possible mouth breather. Such bias was minimized by observing labial sealing for 5min, observed by two evaluators during a distractor task. Thus, they did not divide the sample into mouth and nasal breathers, analyzing the respiratory characteristics of the sample and comparing them with the cognitive-linguistic skills.
The assessed studies that comprised the sample used non-probabilistic samples, chosen intentionally or by convenience, that can result in bias in data interpretation as it depends on the researcher's appraisal. Despite the abovementioned fact, Kuroishi et al.22 carried out a sample calculation study to determine the sample size that would provide a more representative population and more accurate results.25
Although school failure is a complex analysis variable since other aspects can influence its occurrence, it is inferred that students with learning disorders have a greater chance for failure. Therefore, it would be worthwhile for studies to show whether the sample consisted of students that did or did not fail school. The research by Fensterseifer et al.20 established a minimum of two years, and the study by Vera et al.16 reported complaints (by most of the family members of mouth breathers) of learning difficulties, while 39% had failed (from one to three times), more often in elementary school. Other studies14,15,17–19,21,22 did not mention school failure, and in the study by Abreu et al.,13 the students were required to be at the appropriate school year for age, i.e., those students who failed were not included in the study, which may be considered a weakness.
Another important factor for analysis is the place where the selected studioes occurred and the time period during which the studies were performed, since climate change must be taken into account.26 Most studies in our sample were carried out by Brazilian researchers,13,15–22 which justifies our interest in the subject. Only four studies (40%)13,15,17,20 indicated the period (in months or years) during which the sample selection was obtained.
Researchers27 have emphasized the impact of climate change on upper airway (UA) disorders in children younger than 13 years in the metropolitan region of São Paulo, in the months that correspond to the start of winter. They added that the peak of respiratory disease morbidity occurs in May, possibly due to thermoregulation problems in subjects adapted to the milder climate/weather of April, explaining that people with thermoregulation problems are more sensitive to respiratory and cardiovascular diseases, especially the pediatric population.
There is an increase in hospital consultations27 during this period and, consequently, a higher probability of school absenteeism, which can impair academic performance, depending on the chronicity of the condition.
In Brazil, respiratory diseases accounted for 5% of the years of life lost due to premature death,28 emphasizing the importance of public health measures to reduce this percentage.
Another analysis variable concerns the impact of urbanization on the living conditions and health of the Brazilian population. It can be observed that of the ten selected studies, half were performed in capital cities13,15,17,20,21 and the other half14,16,18,19,22 in well-developed cities. In large Brazilian cities, according to Maricato,29 there has been an increase in ecological social inequality, a situation in which there is an uncontrolled growth of cities, with population increase in the outskirt regions. Usually, the individuals living in the outskirts of Brazilian cities have a low socioeconomic status (as demonstrated by research)30 and, thus, are more vulnerable to factors that can compromise quality of life and health.
In addition to the aforementioned facts, it can be observed that school failure is higher in boys than in girls, predominantly among African-descendants and/or those from low-income families.30 This study sample was mostly comprised of boys, confirming what literature has shown, both with respect to school failure and the possibility of the presence of a comorbidity factor, such as ADHD.16
Thus, it is possible to conclude that the understanding of the determinants of learning and its failure are multifactorial and complex; moreover, there are few validated tools to investigate learning disorders, and that creates difficulty when comparing the procedures. Only two studies22 used validated tools, another21 used a published protocol that was adapted to Brazilian students, and another19 applied an evaluation test that was used in a different non-validated study; the remaining studies13–16,18,20 did not use assessment protocols with the students, but instead used school failure records or questionnaires applied to family members or teachers, increasing the analysis bias in such studies.
The School Achievement Test (Teste de Desempenho Escolar – TDE), developed by Lilian Stein,31 was partially used in one study (10%).22 The study compared the experimental group with a control group and the subjects were matched for age and educational level, with part of the sample showing mouth breathing. It was verified that such students had lower school performance than the control group in reading comprehension, arithmetic, and working memory tasks (except for numbers).
Regarding the assessment of mathematical skills, two19,22 of the studies that applied tests found results indicating difficulties in mouth breathers, while the other one did not.21 Reading comprehension was considered worse in mouth breathers,22 as well as writing skills in subjects with respiratory disorder characteristics, when compared with those without such disorders.21
Therefore, in general, most researchers reported learning difficulties in subjects with abnormal breathing pattern.
Thus, studies involving mouth breathing and learning require further investigation, since the number of studies for analysis was small and showed diverse evaluation procedures. Controlled, interdisciplinary studies, with the inclusion of standardized assessments, using validated tools and uniform sample groups must be performed so that a systematic meta-analysis review study can be carried out and, thus, more scientific evidence will become available, both for clinical practice and for the implementation of public health and education policies.
ConclusionsThere is evidence that the breathing pattern can influence the learning process. This systematic review showed that mouth breathers are more likely to have learning difficulties than nasal breathers. Further studies are needed in order to increase the scientific evidence for clinical practice, and for the implementation of public health and education policies.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Ribeiro GCA, dos Santos ID, Santos ACN, Paranhos LR, César CPHAR. Influence of the breathing pattern on the learning process: a systematic review of literature. Braz J Otorhinolaryngol. 2016;82:466–78.