Hemangioma in the nose and nasal sinuses is rare,1 particularly in the maxillary sinus.2 Differentiation of hemangioma from malignant tumors is important, because both may be accompanied by bone destruction. With regard to giant hemangioma, this type has a rich blood supply, and surgical treatment requires particular care due to the high risk of massive bleeding and obstructed field of view. Although maxillary sinus hemangioma has been sporadically reported, few reports have described cases of this type diagnosed according to the 1996 classification of the International Society for the Study of Vascular Anomalies (ISSVA) and treated with arterial embolization.
Here, we report three cases of massive sinonasal heamangioma that were resected after arterial embolization.
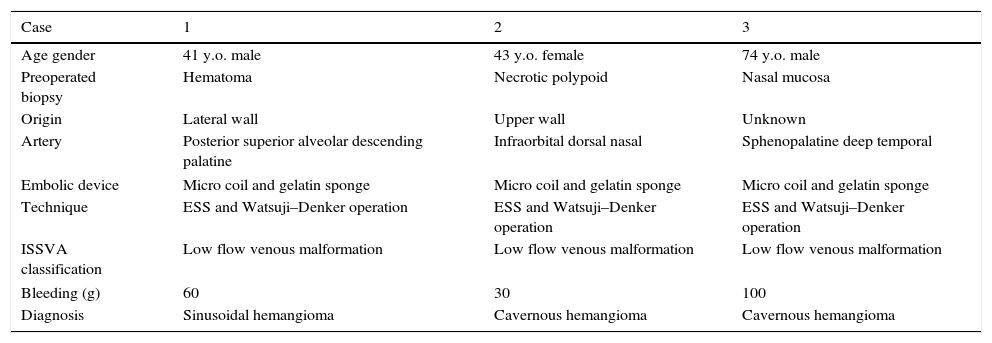
Case reportAn overview of the three cases is shown in Table 1.
An overview of the three cases.
| Case | 1 | 2 | 3 |
|---|---|---|---|
| Age gender | 41 y.o. male | 43 y.o. female | 74 y.o. male |
| Preoperated biopsy | Hematoma | Necrotic polypoid | Nasal mucosa |
| Origin | Lateral wall | Upper wall | Unknown |
| Artery | Posterior superior alveolar descending palatine | Infraorbital dorsal nasal | Sphenopalatine deep temporal |
| Embolic device | Micro coil and gelatin sponge | Micro coil and gelatin sponge | Micro coil and gelatin sponge |
| Technique | ESS and Watsuji–Denker operation | ESS and Watsuji–Denker operation | ESS and Watsuji–Denker operation |
| ISSVA classification | Low flow venous malformation | Low flow venous malformation | Low flow venous malformation |
| Bleeding (g) | 60 | 30 | 100 |
| Diagnosis | Sinusoidal hemangioma | Cavernous hemangioma | Cavernous hemangioma |
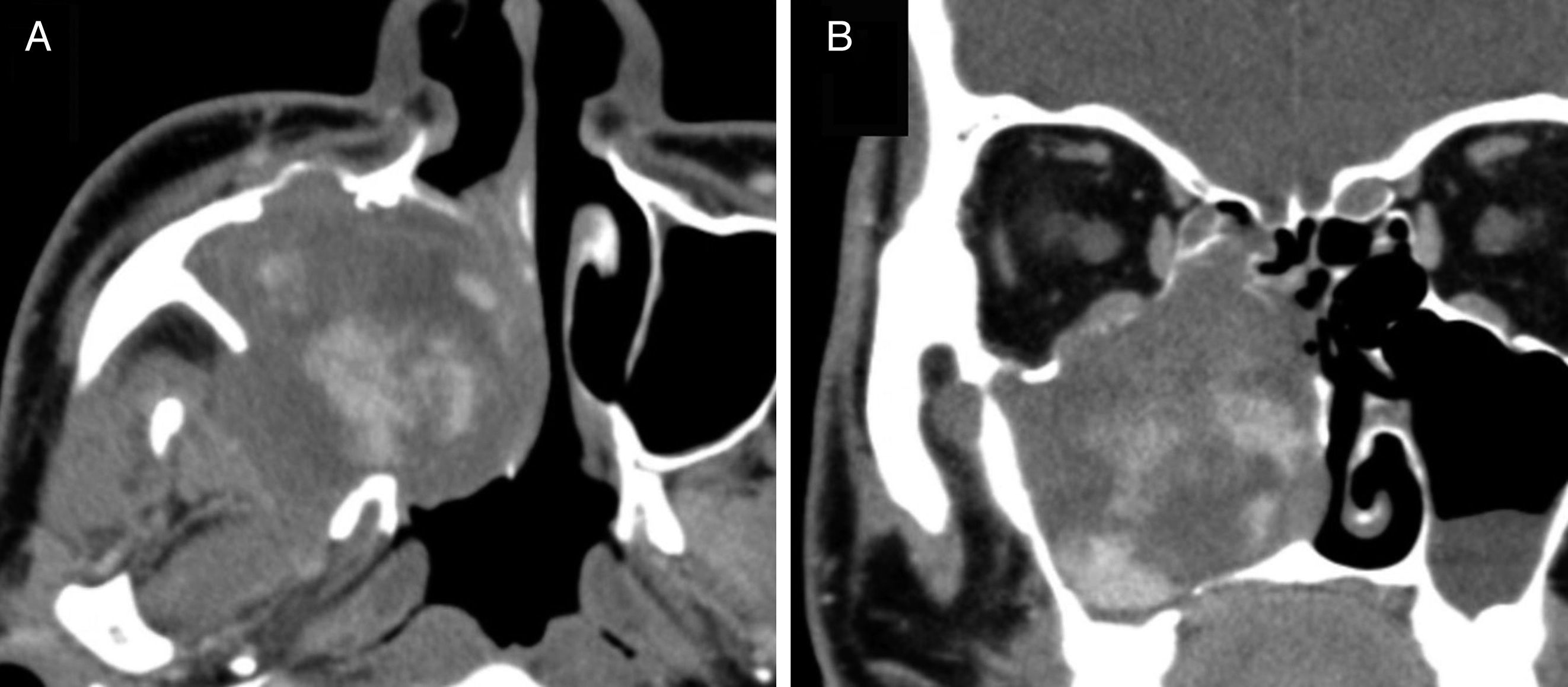
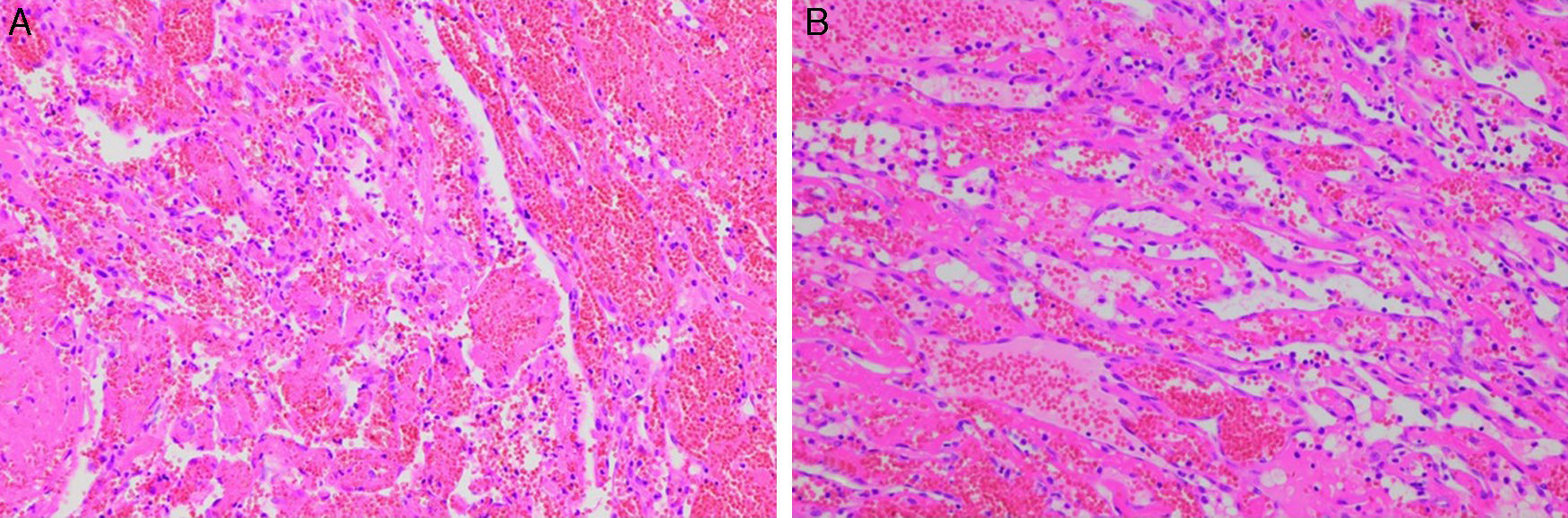
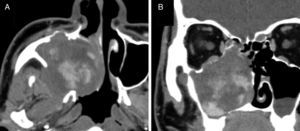
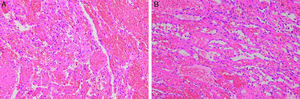
A 43-year-old man presented with recurrent right nasal bleeding and nasal obstruction for six months. Mucosal swelling was observed from the maxillary sinus to the nasal septum in the right inferior and middle nasal meatuses. Sinus computed tomography (CT) revealed a soft tissue density shadow, with a contrast-enhanced interior in a scattered and gradually increasing pattern (Fig. 1). No calcification was observed. Gadolinium contrast magnetic resonance imaging (MRI) showed that the inside of the mass was markedly contrast-enhanced, suggesting a vascular tumor. Sphenopalatine arteriography showed tumor staining with a collection of thin, meandering arteries extending from the posterior superior alveolar artery and descending palatine artery. The tumor, which was contrast-enhanced during the arterial phase, was a slow-flow vascular lesion, from which the contrast medium was partially washed out in the late phase, and was diagnosed as venous malformation according to the ISSVA classification. Both arteries were embolized. Three days later, the patient underwent combined surgery with an endoscopic procedure and the Watsuji–Denker operation. Intraoperative blood loss was 30mL. Sinusoidal hemangioma, a variant of cavernous hemangioma, was diagnosed by histopathology (Fig. 2A). In 24 months of follow-up conducted every three months, however, we have yet to recognize recurrence.
Pathological findings in Case 1 (A) and Case 3 (B). (A) The submitted material consisted of abundant coagulation with intermingling fibrous capsule and aggregation of vessel structures. The vessels are thin and delicate, with an anastomosing structure. (B) The submitted materials contained thick fibrous capsule and vessel structures. Morphological features of the vessel structure are consistent with cavernous hemangioma.
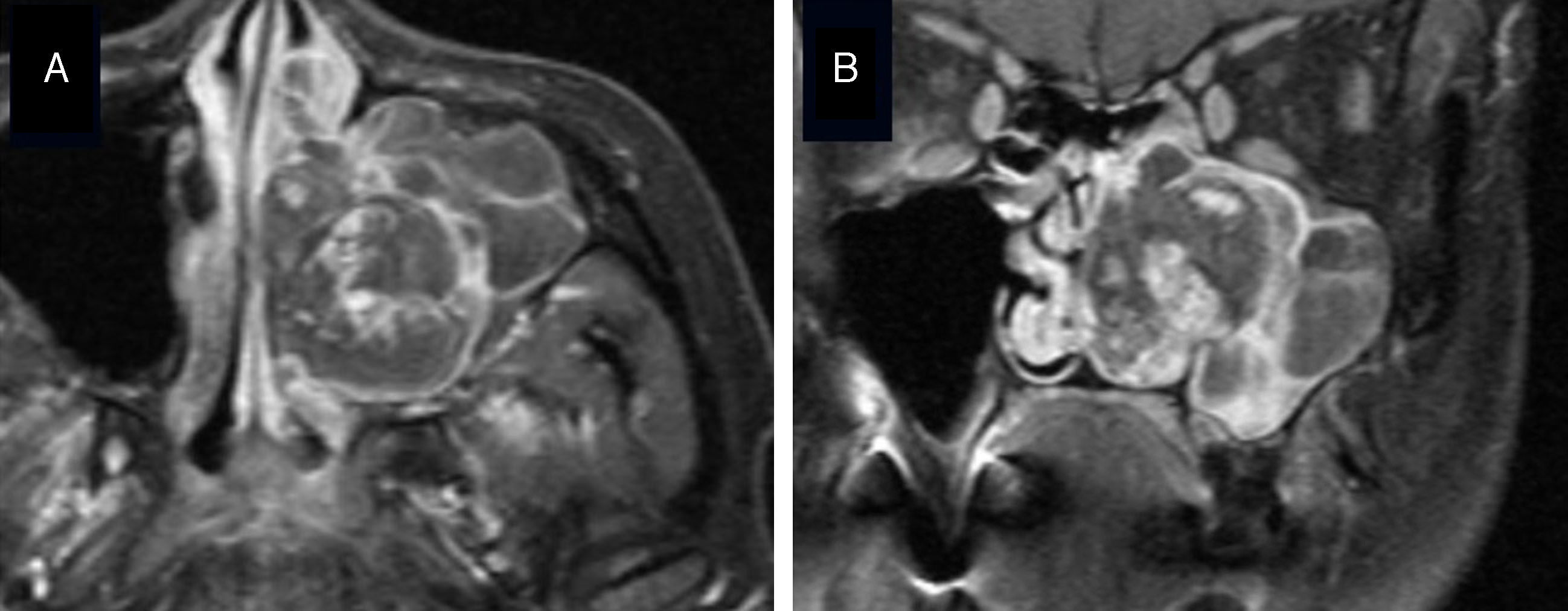
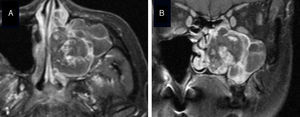
A 41-year-old woman presented with recurrent left nasal bleeding and nasal obstruction for a month. Her left common nasal meatus was filled with edematous mucosa. Sinus CT revealed a soft tissue density shadow occupying the left maxillary sinus, ethmoid sinus, frontal sinus, and nasal cavity, with a bone defect on the medial wall of the left maxillary sinus. In addition, CT showed a soft tissue density shadow including blood retention that filled the left maxillary sinus. The medial wall of the maxillary sinus showed destruction and was increasingly contrast-enhanced. A 30mm heterogeneously enhanced vascular tumor was suspected, based on gadolinium-enhanced MRI (Fig. 3). Facial arteriography showed tumor staining from the infraorbital artery on the upper wall of the left maxillary sinus, and the artery was embolized. In addition, the dorsal nasal artery was embolized. The tumor was a slow-flow vascular lesion, and venous malformation was diagnosed according to the ISSVA classification. Four days later, the patient underwent combined surgery with an endoscopic procedure and the Watsuji–Denker operation, and the entire lesion was extracted. Intraoperative blood loss was 30mL. The postoperative pathological diagnosis was cavernous hemangioma. In 18 months of follow-up conducted every three months, however, we have yet to recognize recurrence.
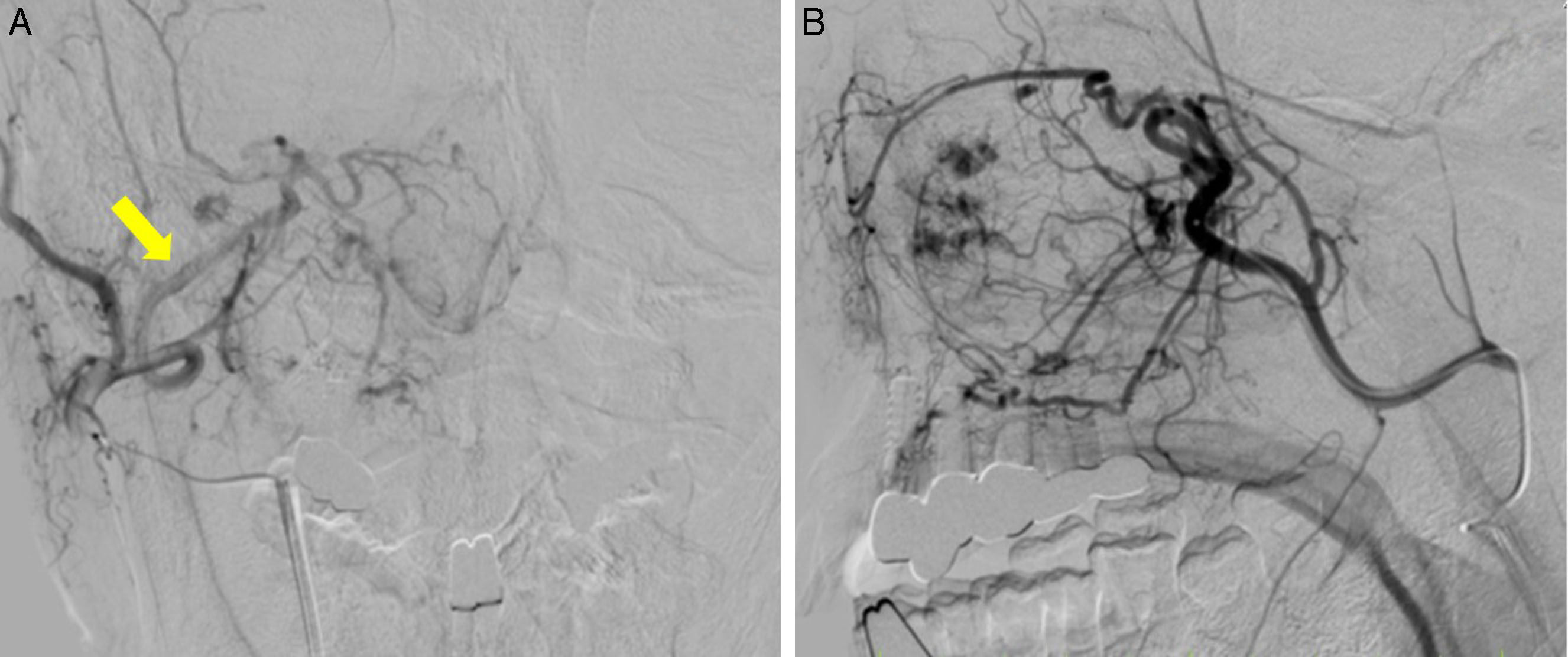
Case 3A 74-year-old man presented with right nasal bleeding and nasal obstruction. Two years before, the patient had experienced right nasal bleeding lasting a few hours. Myelodysplastic syndrome was diagnosed. An edematous polyp occupying the right common nasal meatus was observed. Sinus CT showed a soft tissue density shadow occupying the right maxillary sinus, ethmoid sinus, and frontal sinus to the left nasal cavity, with bone destruction on the medial wall of the right maxillary sinus. Contrast CT showed a lobulated tumorous lesion that was gradually contrast-enhanced from the maxillary sinus to the common nasal meatus, as well as microvascular development in the tumor. Gadolinium-enhanced MRI showed a heterogeneously enhanced lesion, raising suspicion of a vascular tumor. Tissue biopsy showed only nasal mucosa. External carotid arteriography showed tumor staining in the area corresponding to the entire right maxillary sinus. Sphenopalatine arteriography showed that the infraorbital artery, descending palatine artery, and a number of small medial/lateral posterior nasal branches were involved as feeders. The main trunk of the sphenopalatine artery and branches of the deep temporal artery were embolized (Fig. 4). The tumor was a slow-flow vascular lesion diagnosed as venous malformation according to the ISSVA classification. Four days later, the patient underwent combined surgery with an endoscopic procedure and the Watsuji–Denker operation, and the entire lesion was extracted. Intraoperative blood loss was 100mL. The postoperative pathological diagnosis was cavernous hemangioma (Fig. 2 B). In 18 months of follow-up conducted every three months, however, we have yet to recognize recurrence.
DiscussionIn a report of 281 cases of hemangioma, 55 percent occurred on the face and extracranial head, and 5 percent occurred on the neck,3 with these lesions only rarely occurring in the nose or nasal sinuses.1 Of those which do occur in the nose and nasal sinuses, about 80 percent occur on the nasal septum, in Kiesselbach's area in particular, and 15 percent on the lateral wall of the nasal cavity. Hemangioma occurring in the sinus cavity is even rarer. Cavernous hemangioma occurs far less frequently than capillary hemangioma, usually developing on turbinate bone and rarely on the bony tissue of the maxillary sinus wall.4
Sinusoidal hemangioma,5,6 diagnosed on histopathology in Case 1, is a markedly rare histological type (Fig. 4) which is relatively unknown among pathologists. Because only a few cases of sinusoidal hemangioma have been reported since the initial description by Calonje and Fletcher in 1991, a clear recognition of the clinicopathological characteristics of this type will avoid diagnostic pitfalls. Patient follow-up has revealed no tendency toward either local recurrence or metastasis5; however, Ciurea et al. reported three reoperations for recurrence.7 In our cases, the preoperative CT showed bone destruction. Given the rarity of sinusoidal hemangioma and the possibility that other vascular neoplastic lesions might also be present, a high risk of local recurrence and metastasis lesions with similar CT and MRI findings, such as hemangiopericytoma and hemangiosarcoma in these cases, cannot be denied.
Hemangioma is commonly diagnosed radiographically, according to the classification adopted at the 1996 ISSVA meeting. In the ISSVA classification, conventionally diagnosed hemangiomas are divided into vascular tumors and vascular malformations.8 Vascular malformations, conventionally classified as cavernous hemangiomas, do not regress spontaneously and sometimes require treatment when they gradually increase in size. They may be further subdivided into slow- and fast-flow lesions; fast-flow lesions can be treated with semipermanent and reliable embolization, such as via micro coils. Knowing the flow speed helps to determine the embolization method and is a useful reference for intravascular treatment.
We considered that our surgical method was effective on the basis of two criteria: the low rate of perioperative hemorrhage and the reported successful postoperative management. We were able to limit intraoperative bleeding to 60mL, 30mL, and 100mL for Cases 1–3, respectively. Further, postoperative bleeding was sufficiently controlled by the placement of gauze tampons. In a previous report, a patient who did not undergo arterial embolization required two emergency room visits for the treatment of postoperative bleeding.9 Another study reported that massive sinonasal hemangioma was able to be resected endoscopically, albeit with effort, including preoperative arterial embolization and an increase in surgical access to the tumor via the construction of a control hole at the canine fossa.10 For our three patients, in contrast, we chose the combination of an endoscopic procedure and the Watsuji–Denker operation with preoperative arterial embolization, which facilitated our investigation and care of the postoperative lesion.
ConclusionThese three cases were diagnosed as slow-flow venous malformations, in accordance with the ISSVA classification. Angiography and arterial embolization both aided accurate diagnosis of the primary site and the control of bleeding. These very rare cases are amenable to relatively routine treatment following careful assessment and a planned approach.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Hasegawa H, Matsuzaki H, Furusaka T, Oshima T, Masuda S, Unno T, et al. Maxillary sinus hemangioma: usefulness of embolization according to classification. Braz J Otorhinolaryngol. 2017;83:490–3.
Peer Review under the responsibility of Associaçao Brasileira de Otorrinolaringologia e Cirurgia Cervico-Facial.