Most patients with laryngeal carcinoma present tumors in the glottis that can be treated by different treatment modalities. Some authors consider open partial laryngectomy as obsolete, while others still deem this as a viable and cost-efficient option.
ObjectivesTo compare the oncological and functional results of a series of patients undergoing partial laryngectomy vs. external radiotherapy for the treatment of glottic cancer.
MethodsHistorical cohort study with a series of glottic carcinoma patients undergoing partial laryngectomy or external radiotherapy during a period of ten years.
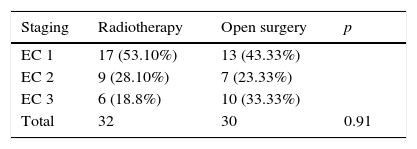
ResultsSixty-two patients with glottic carcinoma were included. Group A comprised those submitted to partial laryngectomy (n=30), and Group B, those who underwent radiotherapy (n=32). They were homogeneous in the comparison of mean age, 56.4 vs. 60.4 years (p=0.12) and distribution in pathological stage (p=0.91). With regard to oncological outcome, there were no differences in distant metastasis rates, or second primary tumor between groups (p=1.0), as well as in disease-free time, laryngeal rescue-free time, and overall five-year survival. Severe complication rates were also similar between groups.
ConclusionOpen partial laryngectomy had complication rates and oncological results similar to those of radiotherapy for patients with glottic carcinomas and should still be considered among the main available therapeutic options.
A maioria dos pacientes com carcinoma de laringe apresentam tumores na região glótica suscetíveis a diferentes modalidades de tratamento. Alguns autores consideram a laringectomia parcial aberta em desuso enquanto outros ainda a indicam como uma opção viável e custo eficiente.
ObjetivosComparar os resultados oncológicos e funcionais de uma série de pacientes submetidos à laringectomia parcial versus radioterapia externa para o tratamento do câncer glótico.
MétodoEstudo tipo coorte histórica com uma série de pacientes com carcinoma glótico submetidos à laringectomia parcial ou radioterapia externa em período de 10 anos.
ResultadosForam incluídos 62 pacientes com carcinoma glótico distribuídos em Grupo A: submetido à laringectomia parcial (n = 30) e Grupo B submetido a radioterapia (n = 32) que se mostraram homogêneos na comparação de média de idade de 56,4 vs. 60,4 (p = 0,12) e distribuição em estadios patológicos (p = 0,91). Com relação ao desfecho oncológico, não foram observadas diferenças nas taxas de metástase à distancia, ou segundo primário entre os grupos (p = 1,0) assim como no tempo livre de doença, tempo livre de resgate laríngeo e sobrevida geral em 5 anos. As taxas de complicações severas também foram semelhantes entre os grupos.
ConclusãoA laringectomia parcial aberta apresentou taxas de complicações e resultados oncológicos semelhante àqueles do tratamento radioterápico para pacientes com carcinomas glóticos e ainda deve ser considera entre as principais opções terapêuticas disponíveis.
Laryngeal carcinoma varies in incidence throughout different geographical regions, being more common in Southern Europe (10.9/100,000), Eastern Europe (9.2/100,000), and South America (7.2/100,000). This cancer is more frequent in males and corresponds to 2.5% of all tumors in men, representing the sixth most common malignancy in men in Brazil.1 Most patients with laryngeal carcinoma present their tumor in the glottic region, and 55–75% are diagnosed with early cancers, with a favorable prognosis.2–5 Therefore, in these cases whenever possible the therapy for laryngeal cancer should aim for a high rate of local control associated with preservation of function. Such results can be achieved by different approaches, including external beam radiotherapy, transoral laser microsurgery, partial open laryngectomy and, more recently, robotic transoral surgery. Each of these options has specific advantages and limitations, such as tumor extension, need for functional reconstruction, technical skill, and adequate resources.6,7
Currently, a predominance of radiotherapy and transoral laser microsurgery appear to be the treatment modalities most commonly used, particularly for early glottic carcinomas, with open partial laryngectomy considered by some authors to be falling into disfavor.8 However, others have noted that open surgery can guarantee an adequate oncological control, associated with a more accurate pathological staging for the correct indication of adjuvant therapy and risk stratification of these patients.9,10 Although surgery and radiation therapy have coexisted as a treatment for cancer of the larynx since the early 20th century, there are still conflicting results when these two therapeutic modalities are compared. The aim of this study was to evaluate the oncological and functional results of a series of patients undergoing open partial laryngectomy vs. external radiotherapy for the treatment of glottic cancer of larynx.
MethodsThis was a longitudinal historical cohort study approved by the local Research Ethics Committee under No. 20538013.2.0000.5362 and based on data collection of medical records from patients with squamous cell carcinoma in a glottal laryngeal site, confirmed by the pathology service and submitted to partial laryngectomy or external beam radiation therapy at a tertiary center from 2002 to 2012. Patients with selected T1/T2 and T3 early glottic carcinoma limited to the glottis without massive extension to the supraglottis, infraglottis or to the paraglottic space, and who were suitable for treatment with organ preservation, were considered for inclusion criteria in the study. Patients with bulky T3 glottic carcinoma not suitable for conservative surgical treatment and patients with advanced T4 carcinoma, as well as patients with minimal clinical follow-up (less than 24 months) were excluded from the study.
All patients were informed about treatment options by a multidisciplinary team involving surgeons, radiation oncologists, and medical oncologists, and after counseling underwent partial laryngectomy or radiation therapy with a total dose of 70Gy (fractionated at 2Gy/day, five days per week) as initial treatment, depending on the patient's preference. Chemotherapy with cisplatin 20mg/m2/day in combination with 5-fluorouacil 1000mg/m2/day by intravenous infusion on days 1–4 and 22–25 was performed concomitantly with radiation for patients with T2 or T3 tumors (thus excluding patients with T1 glottic carcinoma) according to institutional protocol. Adjuvant radiotherapy after surgery was indicated for patients who presented narrow-compromised surgical margins, vascular/perineural invasion, and/or regional metastasis. After the selection of patients, an evaluation of homogeneity between the groups was conducted, and the comparability of samples was determined. The epidemiological characteristics, initial treatment type, need for a temporary (during the treatment period) or permanent (patients who were unable to maintain ventilation without tracheostomy after the end of treatment) tracheostomy, use of enteral nutrition via nasogastric tube or gastrostomy, complications during treatment (aspiration pneumonia, blood transfusion, salivary fistula), and need for adjuvant treatment (radiotherapy and/or chemotherapy) were evaluated. An evaluation of oncological results for three-year disease-free time, local-regional recurrence-free time, and overall five-year survival was conducted.
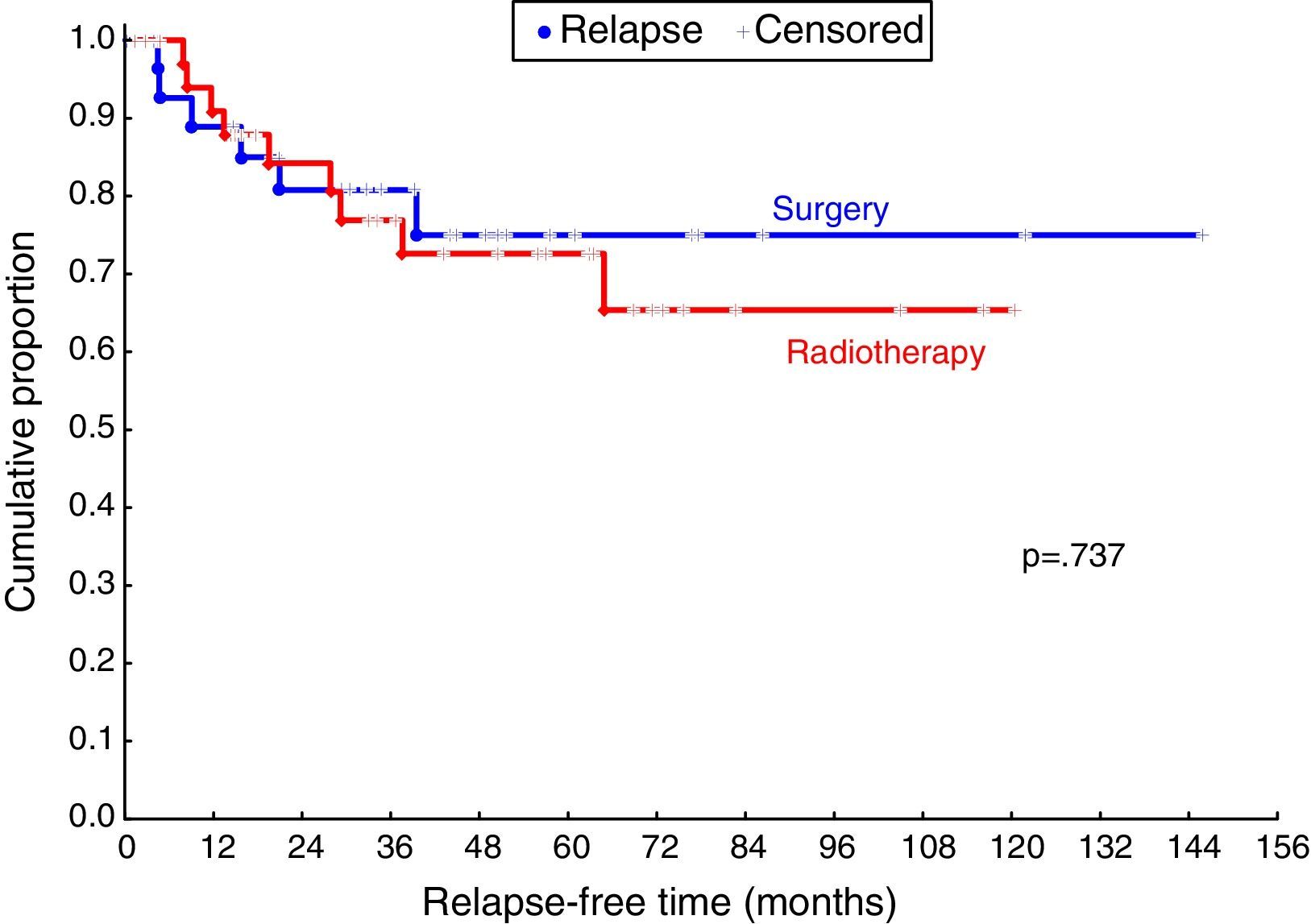
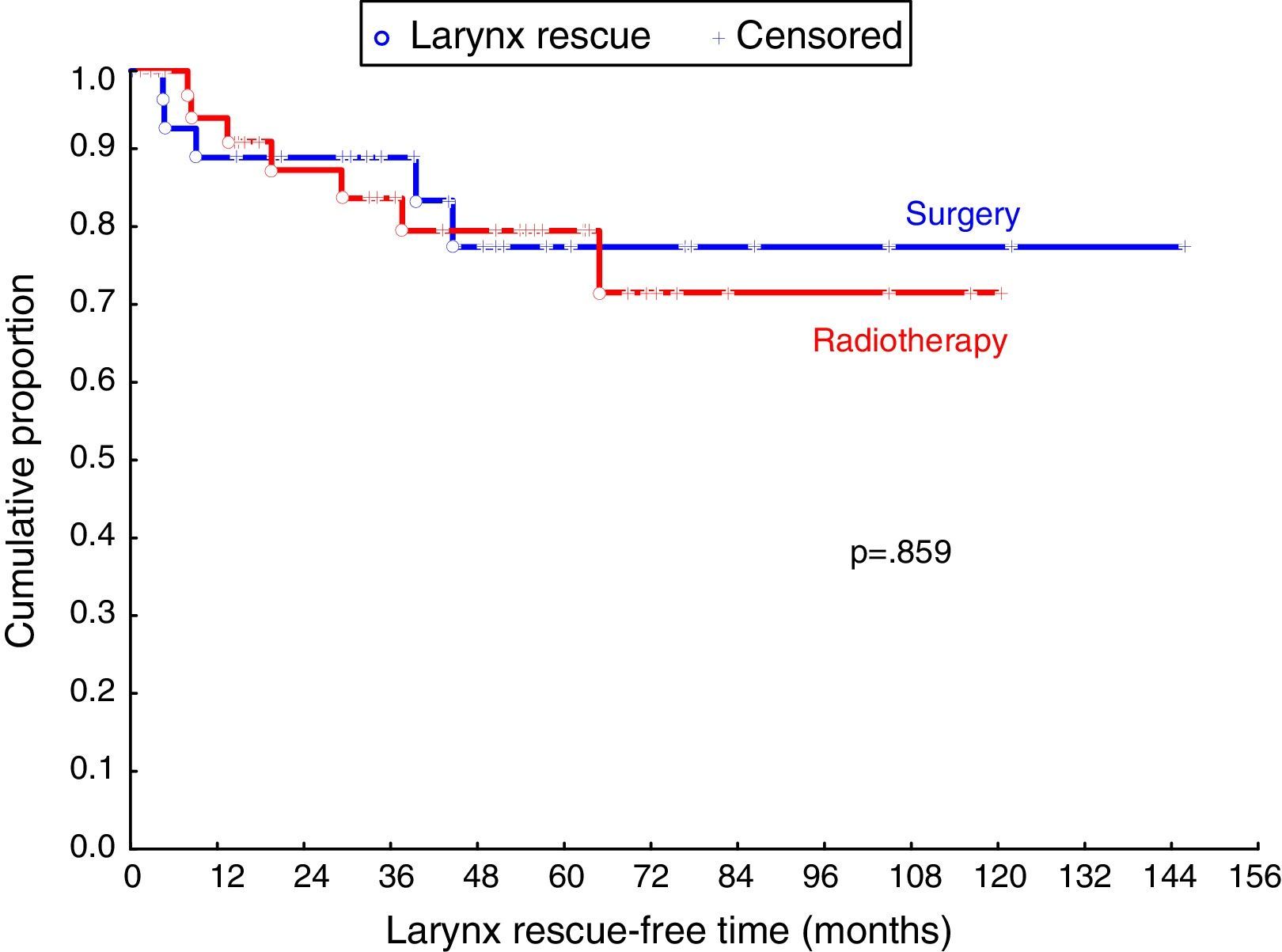
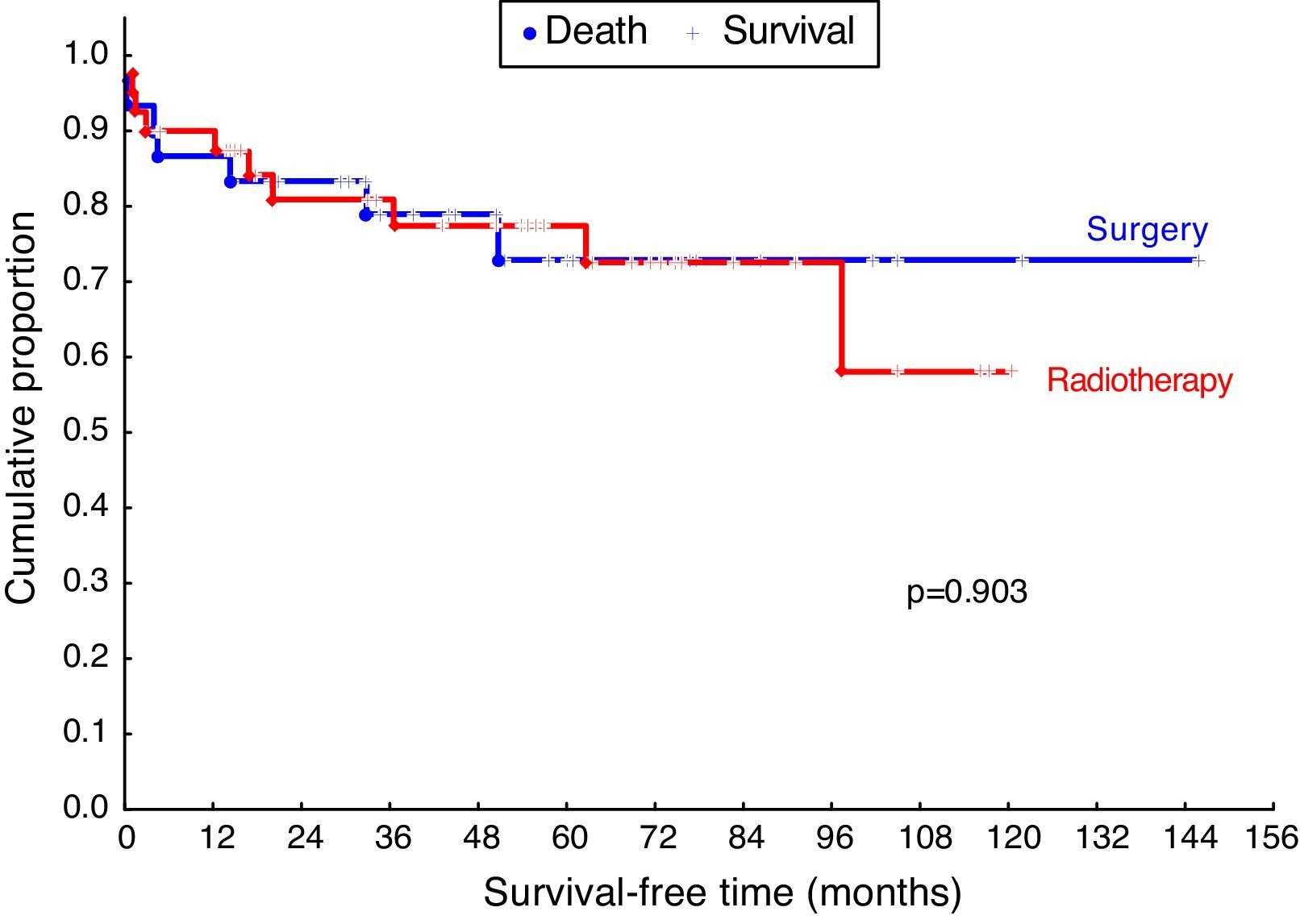
StatisticsThe results of quantitative variables were described as mean, median, minimum and maximum values, and standard deviations. Qualitative variables were expressed as frequencies and percentages. To compare the groups defined by the initial treatment (radiation therapy or surgery) compared to mean age, Student's t-test was used for independent samples. Regarding qualitative variables, either Fisher's exact test or the chi-squared test was employed for this comparison. The comparison between groups with respect to disease-free time, laryngeal rescue-free time, and survival time was carried out using the Log-rank test. Kaplan–Meier curves were presented in order to describe the evolution of the cases in both groups compared to the times of interest. p-Values < 0.05 were considered as statistically significant.
ResultsDuring ten years, 199 patients with laryngeal carcinoma aged between 30 and 84 years, 92.5% male, were evaluated. The most common site of laryngeal cancer was the glottis in 99 patients (49.25%), followed by the supraglottic area in 52 cases (26.13%), while another 49 patients (24.62%) had large lesions classified as transglottic tumors.
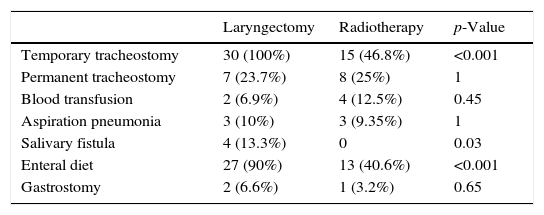
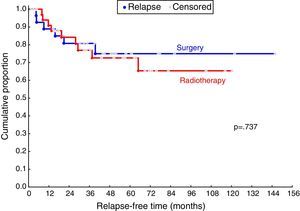
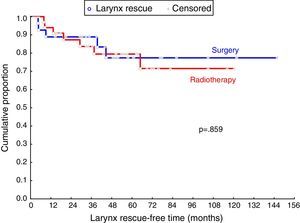
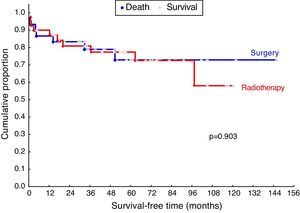
Among the 199 patients with laryngeal carcinoma, 62 patients with glottic carcinoma were included and divided into two groups according to the initial proposed treatment: Group A underwent partial laryngectomy (n=30) and Group B underwent radiotherapy, with or without chemotherapy (n=32). Supracricoid laryngectomy was performed on 18 patients (two T1b, six T2, ten T3), while frontolateral laryngectomy was used in 12 patients (11 T1a and one T2). Both groups were homogeneous when comparing mean age (57.5 vs. 59.5 years for patients undergoing surgery or radiotherapy, respectively). The same was observed for distribution in different clinical staging for the two groups (Table 1). Evaluations of complications during treatment and functional results are presented in Table 2. With regard to oncological outcome, no differences were observed in distant metastasis occurrence rate or in second primary tumor between groups, as well as in disease-free time, laryngeal rescue-free time, and overall five-year survival, as shown in Figs. 1–3.
Complications and functional results.
| Laryngectomy | Radiotherapy | p-Value | |
|---|---|---|---|
| Temporary tracheostomy | 30 (100%) | 15 (46.8%) | <0.001 |
| Permanent tracheostomy | 7 (23.7%) | 8 (25%) | 1 |
| Blood transfusion | 2 (6.9%) | 4 (12.5%) | 0.45 |
| Aspiration pneumonia | 3 (10%) | 3 (9.35%) | 1 |
| Salivary fistula | 4 (13.3%) | 0 | 0.03 |
| Enteral diet | 27 (90%) | 13 (40.6%) | <0.001 |
| Gastrostomy | 2 (6.6%) | 1 (3.2%) | 0.65 |
It is currently accepted that radiotherapy, transoral laser microsurgery, and open partial laryngectomy can provide high local control rates for patients with early glottic carcinoma of larynx coupled with functional conservation of the organ. However, there appears to be no high-level evidence regarding the best treatment option for these patients, because of the lack of randomized studies comparing these different treatment options.11 Conservative surgery has been one of the mainstays of treatment of laryngeal cancer since the first successful resection via laryngofissure credited to Sands in 1863,12 and later followed by the description of a hemilaryngectomy performed by Billroth in 1875.13 In parallel to the development of new techniques for partial laryngectomy, the evolution of radiation therapy resulted in an effective option for conservative treatment for laryngeal carcinomas.14 Since then, some studies have tried to assess the oncological outcomes of radiotherapy and conservative surgery for glottic carcinomas, but conflicting results are often described, as those observed by Bron et al.15 and Zohar et al.,16 who found higher local control rates compared to those of open surgery, while Rucci et al.17 suggested that the local-regional control with radiotherapy would be more efficient, particularly for patients with T1a and T1b glottic carcinomas.
However, Pontes et al.18 followed 43 patients with T1a and T1b laryngeal carcinoma submitted to an initial treatment with radiotherapy and observed a high recurrence rate in 30.2% of patients after a mean follow-up time of 29.5 months. In the present series, it was observed that the overall three-year disease-free rates were similar both for patients undergoing partial laryngectomy (80.8%) and for those undergoing radiotherapy (76.9%). Although there are few studies that directly compared the oncological results of partial laryngectomy vs. radiotherapy for selected early and T3 glottic carcinomas in the same institution, in 1984 Kaplan et al.19 indicated that patients with early glottic carcinomas had similar oncological outcomes when treated with radiotherapy or surgery. However, it was observed that surgery was superior to radiotherapy in patients with reduced or fixed vocal fold mobility (patients selected: T2 and T3); thus, it was suggested that open laryngectomy should be the first line of treatment for these patients. These results were corroborated in a recent evidence-based review by Hartl et al.20; these authors concluded that patients with T2 glottic carcinoma can achieve initial local control rates between 84% and 95%, which are comparable to rates after radiotherapy, open partial surgery, or transoral laser resection. However, they emphasized that patients with T2 glottic carcinoma presenting reduced mobility or deep extension to paraglottic space or ventricle represented a subgroup with lower local control rates, when subjected to radiation or laser transoral surgery. Succo et al.21 also suggested that open partial surgery results in higher local control and long-term laryngeal preservation rates in patients with glottic carcinoma, showing decreased or fixed vocal cord mobility compared to those treated with transoral laser surgery, and considered that this was due to the fact that 16.8% of patients clinically staged as cT2 were classified as pT3 with pathological staging, and that this group would be particularly favored by partial laryngectomy.
In general, there is evidence suggesting that patients with glottic cancer show similar five-year survival rates after radiotherapy or open partial laryngectomy, ranging from 70% to 88% for patients with T1 carcinoma and between 64% and 78% for T2 tumors.4 The same can be observed in the present study, with overall five-year survival rates of 77.4% and 72.9% after radiotherapy and surgery, respectively.
Considering the possibility of similar oncological results, some authors suggest that partial laryngectomy should be considered as the first therapeutic choice for glottic tumors, allowing a precise pathological staging of the disease; radiotherapy would be reserved for adjuvant therapy, or for a second primary carcinoma.22 However, radiotherapy is the primary form of initial treatment for glottic carcinoma in most centers and reaches rates of 84.4% of cases in Canada and 63.2% of patients in the United States.23 One advantage of radiotherapy is the possibility of avoiding a temporary or permanent tracheostomy usually associated with conservative laryngectomy. However, the authors noted that, despite the fact that temporary tracheostomies have been more frequent in patients undergoing partial laryngectomy, definitive tracheostomy rates (patients who could not be decannulated after initial treatment) were 28.1% and 23.3% after radiotherapy and open partial laryngectomy, respectively. Therefore, considering permanent tracheostomy as the main negative functional consequence in the treatment of patients with laryngeal carcinoma,24,25 the present study did not observe a significant difference between these therapeutic modalities regarding this issue.
Another important aspect of the functional preservation of the larynx is the protection fostered by lower airways, allowing continuation of a non-restricted oral diet. While the need for temporary enteral nutrition was significantly higher in patients undergoing surgery, it should be noted that 40.6% of patients undergoing radiotherapy also required enteral nutrition during treatment, and similar rates of dietary need for temporary gastrostomy were observed, both in patients undergoing radiation therapy (3.2%) and open partial laryngectomy (6.7%). Dysphagia after partial laryngectomy is due to local changes, caused by resection of structures and also by changes in the mechanism of laryngeal elevation, while radiation causes damage to the mucosa and pharyngolaryngeal muscle tissues that is directly related to the therapeutic dose used.
Debelleix et al.26 reviewed the literature and concluded that, to reduce the laryngeal edema, it would be appropriate to limit the radiation dose incident to non-tumor areas of the larynx to about 40–45Gy; but today most patients receive 70Gy in conventional radiotherapy. Francis et al. evaluated the relationship between the therapeutic modality and the potential of long-term dysphagia in patients with head and neck cancer, concluding that patients undergoing radiotherapy and chemotherapy are 2.5 times more prone to undergo dysphagia compared to patients undergoing surgical treatment alone.27 Other drawbacks in the quality of life for patients with laryngeal cancer are also reported, for instance, worsening in voice quality and a predisposition to respiratory infections (aspiration pneumonia) due to weakness in swallowing. Traditionally, it has been considered that surgery, either open or endoscopic, is responsible for the higher incidence of these undesirable effects when compared to radiation therapy. This study demonstrated that the incidence of aspiration pneumonia was comparable after radiotherapy (9.35%) and open partial laryngectomy (10%). Some studies have also shown that partial laryngectomy promotes better results concerning dental problems, dry mouth, and swallowing in general.4,8
Although the literature suggests that oncological and functional results can be similar when comparing open partial laryngectomy vs. radiotherapy for patients with glottic cancer, the authors have noted a decline in the use of open surgery in recent decades in favor of less invasive treatment modalities, such as radiation or transoral laser resection. However, it is important to emphasize that partial laryngectomy remains an oncologically and functionally effective option, especially for patients with glottic carcinomas with a decrease or fixation of vocal fold mobility, or in situations such as unavailability of laser technology or even in radiotherapy services with a long waiting time for treatment.
ConclusionOpen partial laryngectomy presented disease-free time and overall survival outcomes similar to those obtained with radiotherapy for selected patients with early glottic and T3 carcinomas, also demonstrating similar rates of severe laryngeal dysfunction with need of permanent tracheostomy. Therefore, this procedure must be maintained among the main therapeutic modalities available for such cases, and the treatment selection should consider the availability of local resources, waiting time for each treatment modality, and personal preferences.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Graciano AJ, Sonagli M, da Silva AGC, Fischer CA, Chone CT. Partial laryngectomy in glottic cancer: complications and oncological results. Braz J Otorhinolaryngol. 2016;82:275–80.