It has become common to use scales to measure the degree of involvement of facial paralysis in phonoaudiological clinics.
ObjectiveTo analyze the inter- and intra-rater agreement of the scales of degree of facial paralysis and to elicit point of view of the appraisers regarding their use.
MethodsCross-sectional observational clinical study of the Chevalier and House & Brackmann scales performed by five speech therapists with clinical experience, who analyzed the facial expression of 30 adult subjects with impaired facial movements two times, with a one week interval between evaluations. The kappa analysis was employed.
ResultsThere was excellent inter-rater agreement for both scales (kappa>0.80), and on the Chevalier scale a substantial intra-rater agreement in the first assessment (kappa=0.792) and an excellent agreement in the second assessment (kappa=0.928). The House & Brackmann scale showed excellent agreement at both assessments (kappa=0.850 and 0.857). As for the appraisers’ point of view, one appraiser thought prior training is necessary for the Chevalier scale and, four appraisers felt that training is important for the House & Brackmann scale.
ConclusionBoth scales have good inter- and intra-rater agreement and most of the appraisers agree on the ease and relevance of the application of these scales.
A utilização das escalas para mensurar o grau de comprometimento da paralisia facial tem se tornado rotina cada vez mais comum na clínica fonoaudiológica.
ObjetivosAnalisar a concordância inter- e intra-avaliadores das escalas do grau de paralisia facial e a opinião dos avaliadores quanto à sua utilização.
MétodoEstudo clínico observacional transversal das escalas de Chevalier e de House & Brackmann, realizado com cinco fonoaudiólogos com experiência clínica que analisaram a expressão facial de 30 indivíduos adultos com variação de comprometimento da mímica facial, por duas vezes, com intervalo de uma semana entre sessões. A análise de kappa foi empregada.
ResultadosHouve excelente concordância inter-avaliadores para as duas escalas (kappa>0,80) e na escala de Chevalier foi observada concordância substancial intra-avaliadores na 1ª avaliação (kappa=0,792) e excelente na 2ª avaliação (kappa=0,928). A escala de House & Brackmann apresentou excelente concordância nos dois momentos da avaliação (kappa=0,850 e 0,857). Quanto à opinião dos avaliadores, na escala de Chevalier um dos profissionais acha necessário treinamento prévio; na escala de House & Brackmann, quatro profissionais acham importante haver o treinamento.
ConclusãoAmbas as escalas apresentam boa concordância inter- e intra-avaliadores e a maioria dos profissionais concorda quanto à facilidade e à relevância da aplicação destas escalas.
Facial palsy can arise from traumatic, iatrogenic, infectious, idiopathic, neoplastic, congenital, metabolic, or toxic origins. The degree of impairment is also quite variable.1 The incidence of Bell's palsy (idiopathic) is estimated to be 20–30 cases per 100,000 people, with a slightly higher prevalence among women.2 The degree of facial paralysis impairment reflects the number of affected axons; the greater the insult to the nerve, the greater the possibility of degeneration of the axonal fibers and of subsequent denervation of muscle fibers of the hemiface.3
The role of phonoaudiology for patients with facial paralysis has grown in recent years; this increase is also evident in scientific studies. Intervention for facial paralysis advocates the optimization of facial expressions and of the functions of chewing, swallowing, and communication.
People with facial paralysis commonly experience functional and psychosocial impairment. The face remains asymmetrical at rest and during motion.4 The mobility of the muscles of the mouth, essential for speech, expression, and also for nourishment, is altered, and because of this there is demand for speech therapy.5 Incomplete and synkinesic movements in the forehead, eyes, nose, and lips also may occur, as well as excessive tearing during activities such as chewing.6,7
From the psychosocial aspect, nonverbal communication becomes compromised8; during speech, several processes are involved, and facial expression enhances and amplifies emotion, i.e., the expressiveness of the context to be transmitted.4 Patients with sequelae of facial paralysis of long duration generally relate communication problems, since they cannot convey their emotions through facial expression, and are prone to having their emotional state misinterpreted.1 One study points to a variety of psychosocial problems occurring as a result of facial paralysis, including depression, anxiety, rejection, and paranoia in patients.9
The needs to determine the prognosis for facial palsy and to plan treatment have led to the development of methods to quantify this problem clinically. Several subjective and objective methods have been proposed for this evaluation; the subjective methods are based on the presence or absence of certain pre-established facial movements,10,11 and include the House & Brackmann,12 Yanagihara,13 and Chevalier14 scales, among others.
The pursuit of evidence-based practice has become essential in the therapeutic process. Thus, the use of scales to measure the degree of facial paralysis involvement has become increasingly common in the clinical phonoaudiological routine.
The agreement in judgments regarding the degree of facial paralysis based on these scales has been widely investigated. The scales depend on the interpretation of a professional; factors such as clinical experience with the disease and with the instrument influence the evaluation. The degree of reliability of a scale can be estimated by measuring the concordance between inter- and intra-rater results achieved in its application to the same patient.15 Thus, the aim of this study was to determine and compare the inter- and intra-rater agreement in the interpretation of the degree of peripheral facial paralysis impairment based on two functional scales, and to relate the appraisers’ point of view on the use of these instruments.
MethodsThis was a cross-sectional observational study approved by the Research Ethics Committee of the Federal University of Minas Gerais, under Opinion No. 406/08. For the conduction of this study, photos of facial expressions of 30 adults with a range of facial mimicry appropriate for complete peripheral unilateral facial paralysis were selected, consisting of three without and 27 with facial paralysis. With this goal in mind, the cases were selected through stratified sampling from the database of clinical procedures for facial paralysis from the Outpatient Speech Clinic of the Federal University of Minas Gerais. A speech therapist with over ten years of experience with the scales, who did not participate in inter- and intra-rater analyses, made the choice of cases, so that an equilibrium was established among the levels of classification of the scales used in the study. The chosen cases included photos of facial expressions according to the instructions that the participants received: frightened face (occipitofrontal muscle), furious face (corrugator supercilii muscle), sad face (depressor muscle of the lower lip), and bad smell face (pyramidal of the nose/transverse of the nose), eyes slightly closed (orbicularis oculi muscle – palpebral portion), eyes tightly occluded (orbicularis oculi muscle – orbital portion), and overhanging lower lip (chin muscle), totaling ten images per participant. Individuals with facial paralysis associated with craniofacial deformity or impairment of bilateral facial movements were excluded.
The photos of each case were presented to and analyzed by five female speech therapists with mean age 27.2 years, who had worked with facial paralysis for at least two years, but with no experience in the use of rating scales for the degree of involvement of facial mimicry. The professionals who agreed to participate in the study signed an informed consent. Regarding the time of training and experience in the area, two professionals (40%) had up to three years, one (20%) had between 3.1 and five years, and two (40%) had more than five years of training.
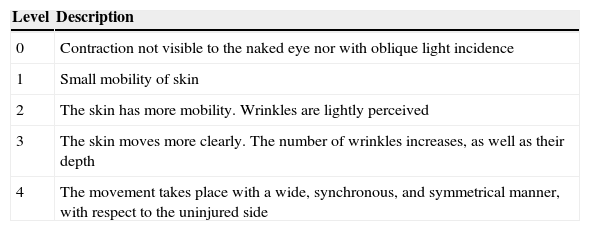
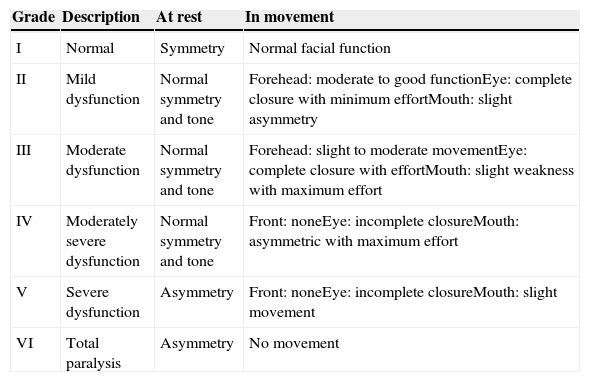
The speech therapists in this study underwent prior training to classify the severity of facial paralysis using the House & Brackmann12 and Chevalier et al.14 scales; the three cases selected for the training were not included in the 30 cases presented for analysis. On the Chevalier scale (Table 1), the facial movements are evaluated globally, and there is no separate analysis for regions of the face, while in the House & Brackmann scale (Table 2) the evaluation is performed separately, where different thirds, namely, forehead, eye, and mouth, are considered. In addition, the House & Brackmann scale allows analysis with the face at rest and in movement.
Assessment of facial movement according to Chevalier (1987).
| Level | Description |
|---|---|
| 0 | Contraction not visible to the naked eye nor with oblique light incidence |
| 1 | Small mobility of skin |
| 2 | The skin has more mobility. Wrinkles are lightly perceived |
| 3 | The skin moves more clearly. The number of wrinkles increases, as well as their depth |
| 4 | The movement takes place with a wide, synchronous, and symmetrical manner, with respect to the uninjured side |
Assessment of facial movement according to House & Brackmann (1985).
| Grade | Description | At rest | In movement |
|---|---|---|---|
| I | Normal | Symmetry | Normal facial function |
| II | Mild dysfunction | Normal symmetry and tone | Forehead: moderate to good functionEye: complete closure with minimum effortMouth: slight asymmetry |
| III | Moderate dysfunction | Normal symmetry and tone | Forehead: slight to moderate movementEye: complete closure with effortMouth: slight weakness with maximum effort |
| IV | Moderately severe dysfunction | Normal symmetry and tone | Front: noneEye: incomplete closureMouth: asymmetric with maximum effort |
| V | Severe dysfunction | Asymmetry | Front: noneEye: incomplete closureMouth: slight movement |
| VI | Total paralysis | Asymmetry | No movement |
After completion of the training, the photos of the facial muscles of 30 subjects were examined individually by the professionals, with no possibility of discussion and for as long as they felt necessary. The analyses were conducted at two different times, with a one-week interval between the two sessions, in order to verify the intra-rater agreement. However, the order of presentation of the cases for the second analysis was changed. For the classification of the degree of facial paralysis change, descriptions of the scales were offered to the speech therapists, for consultation.
After the second evaluation of the cases, the speech therapists were asked to answer a questionnaire with four multiple choice questions, where they expressed their views on the use of the scales, and an open question about what they thought necessary to add in the scales.
The responses of the speech therapists were tabulated and the results were subjected to a statistical analysis using R software, version 2.15.0. To perform analyses of inter- and intra-rater agreement, the weighted coefficient kappa (k) was used. This allowed measurement of the agreement between two or more raters,16 and percentile bootstrap confidence intervals of 95% were used. To check the intra-rater agreement, the researchers took into account the first and second assessments. kappa values=0 were considered as poor agreement, 0–0.20 as slight, 0.21–0.40 as significant, 0.41–0.60 as moderate, 61–0.80 as substantial, and >0.80 as excellent.17
For those questions related to the appraisers’ point of view, a descriptive analysis was conducted.
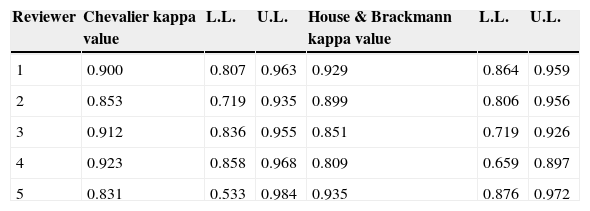
ResultsThe results of the assessment of inter-rater agreement in the interpretation of the degree of facial paralysis impairment (Table 3) showed excellent agreement of all speech therapists for both scales, with kappa>0.80.
Assessment of inter-rater agreement in the interpretation of the degree of facial paralysis impairment.
| Reviewer | Chevalier kappa value | L.L. | U.L. | House & Brackmann kappa value | L.L. | U.L. |
|---|---|---|---|---|---|---|
| 1 | 0.900 | 0.807 | 0.963 | 0.929 | 0.864 | 0.959 |
| 2 | 0.853 | 0.719 | 0.935 | 0.899 | 0.806 | 0.956 |
| 3 | 0.912 | 0.836 | 0.955 | 0.851 | 0.719 | 0.926 |
| 4 | 0.923 | 0.858 | 0.968 | 0.809 | 0.659 | 0.897 |
| 5 | 0.831 | 0.533 | 0.984 | 0.935 | 0.876 | 0.972 |
L.L., lower limit of the 95% confidence interval; U.L., upper limit of the 95% confidence interval.
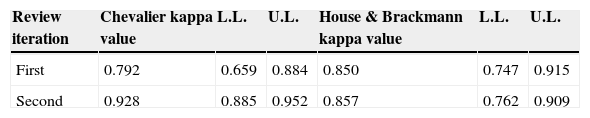
As to the intra-rater investigation (Table 4), in the first assessment and, after a week, in the second assessment, the use of the Chevalier scale resulted in an agreement that was considered substantial for the first (kappa=0.792) and excellent for the second (kappa=0.928) assessment. However, the House & Brackmann scale obtained an excellent agreement at both times of assessment (kappa=0.850 and 0.857, respectively).
Evaluation of intra-rater interpretation of the degree of facial paralysis impairment in both moments of evaluation.
| Review iteration | Chevalier kappa value | L.L. | U.L. | House & Brackmann kappa value | L.L. | U.L. |
|---|---|---|---|---|---|---|
| First | 0.792 | 0.659 | 0.884 | 0.850 | 0.747 | 0.915 |
| Second | 0.928 | 0.885 | 0.952 | 0.857 | 0.762 | 0.909 |
L.L., lower limit of the 95% confidence interval; U.L., upper limit of the 95% confidence interval.
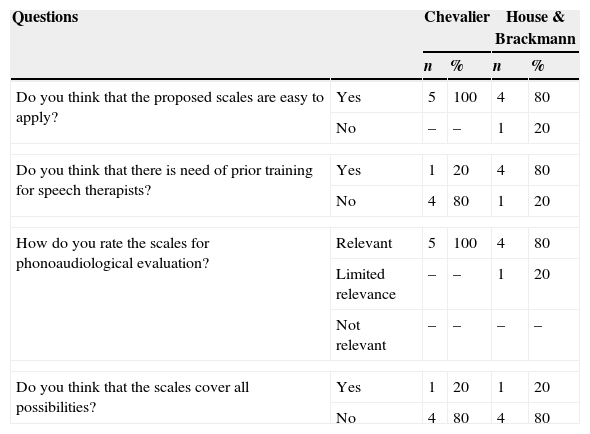
The opinion of the involved professionals, regarding the use of the scales, revealed that the majority considered the scales as easy to use and relevant. For the House & Brackmann scale, they considered it necessary to have some prior training (Table 5). In the open question, when asked about what could be added to the scales to enhance their use, the speech therapists suggested improving the subdivision of the scores for the “in movement” section, and a better detailing of the facial thirds.
Description of the appraisers’ point of view regarding the scales of facial paralysis.
| Questions | Chevalier | House & Brackmann | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Do you think that the proposed scales are easy to apply? | Yes | 5 | 100 | 4 | 80 |
| No | – | – | 1 | 20 | |
| Do you think that there is need of prior training for speech therapists? | Yes | 1 | 20 | 4 | 80 |
| No | 4 | 80 | 1 | 20 | |
| How do you rate the scales for phonoaudiological evaluation? | Relevant | 5 | 100 | 4 | 80 |
| Limited relevance | – | – | 1 | 20 | |
| Not relevant | – | – | – | – | |
| Do you think that the scales cover all possibilities? | Yes | 1 | 20 | 1 | 20 |
| No | 4 | 80 | 4 | 80 | |
n, number of appraisers.
For cases of facial paralysis, it is crucial to determine the topographic diagnosis, the prognosis, and an etiology so that treatment for the best possible rehabilitation can be delivered.18 The combination of various techniques such as surgery, drugs for clinical treatment, and therapeutic support is essential to achieve success in the recovery of facial motor functioning,3 and the speech therapist is an integral part of the multidisciplinary team. The scales for facial paralysis severity aid in diagnosis and contribute to the definition of medical conduct, including in the area of speech therapy.
The House & Brackmann scale is often advocated by the American Academy of Otolaryngology, and the Chevalier scale is mentioned in the phonoaudiological literature7,19 for evaluation of facial paralysis. For these reasons, they were chosen in this study.
The results of this study indicated that there is a high index of inter-rater agreement for both scales, since the value of kappa>0.80 is classified as an excellent agreement.17 Instruments of this nature are fundamental to quickly and clearly evaluate the effectiveness of rehabilitation therapies. It has been reported that the House & Brackmann scale identified the positive results of a protocol of orofacial neuromuscular rehabilitation for peripheral facial paralysis.20
As for the intra-rater analysis, these results revealed that there is agreement in the interpretation of the degree of facial paralysis impairment for both scales, but there is evidence of differences between the first and second assessments with the Chevalier scale. Considering the kappa value, the first evaluation can be classified as having substantial agreement (kappa=0.792), although its value is almost an excellent agreement, while the second evaluation by this scale and both evaluations by the House & Brackmann scale can be classified as excellent, representing total agreement during their evaluation. The occurrence of a greater agreement during the second assessment (kappa=0.928) using the Chevalier scale may indicate that the frequent use of this tool makes it more reliable and effective. The Chevalier scale is intended to classify patients in a simple and practical way, and at first, the non-detailing of the facial function of the facial thirds can lead to generalized and less oriented interpretations.
The scales of Chevalier and of House & Brackmann are considered subjective methods; thus, from the results of this study it can be inferred that, for the Chevalier scale, the higher the frequency of its use, the better the reliability in the classification of facial paralysis.
One study analyzed the use of two rating scales to determine which of the two assessment tools was more appropriate for clinical application. Thus, the House & Brackmann scale and the instrument proposed by Burres and Fisch were used in a normal subject and in 41 patients with abnormal facial movements. The study concluded that the House & Brackmann scale is easy to interpret, providing simple criteria for evaluation, since this instrument evaluates the degree of dysfunction separately, while the system used by Burres and Fisch is time consuming, labor intensive, and requires a complex calculation to determine the degree of facial paralysis impairment.21
Another study22 evaluated the concordance of clinical assessment and self-assessment by the patient after surgical removal of acoustic neurinoma and used the Yanagihara system and the House & Brackmann score. In general, the scores found by the clinicians significantly agreed with the self-assessment of patients. The authors concluded that these two assessment tools are suitable, not only for the clinician but also for the patient as a means of self-assessment.
In the literature, there is obvious interest in comparing assessment scales in patients with facial paralysis. At first, the researchers intended to check the practicality and applicability of these scales in clinical routines. Subsequently, an interest to examine whether the interpretation of clinical examination of facial palsy was similar to the patient's interpretation emerged, suggesting the importance of a psychosocial and clinical perspective. In the present study, the aim was to evaluate whether the instruments used for clinical evaluation are reliable and, comparing the two scales used, to define whether in either there is more agreement with respect to the clinical judgment of the appraisers.
Regarding the appraisers’ point of view with respect to the scales proposed for evaluation, it was found that in the Chevalier scale, only one appraiser thought that prior training for speech therapists was necessary. However, in the House & Brackmann scale, most appraisers found some training necessary. It is possible to analyze the discrepancy between the responses as a reflection of the many possibilities that the House & Brackmann scale proposes for the grading task, since for each movement of the facial movements the appraisers must consider the following options: normal, moderate, poor, or absent, and at the end they must assign the degree of overall impairment. Due to the greater complexity of the instrument, the speech therapists indicated the need for training. The training provided in this study can be considered sufficient, since the intra-rater results comparing the first and second assessments in the scale showed excellent agreement at both times. Another factor that must also be taken into consideration is the manner by which the House & Brackmann scale orients the analysis of facial movements among the facial thirds, and this may have favored the agreement.
All appraisers rated the application of the Chevalier scale as relevant. As to the House & Brackmann scale, most professionals found it relevant, classifying this instrument as applicable and important for the speech therapy practice. However, for these two analyzed scales, there was only one appraiser who thought that these instruments include all the possibilities for the classification of facial paralysis. All other speech therapists cited points that they considered important, and that the scales did not contemplate. This result is consistent with the assertion that the House & Brackmann scale can generate uncertainty on the conclusion of the degree of involvement, given that the assignment of a single score can be a difficult task, due to different degrees of changes in the upper and lower regions of the face.23
There is controversy about the applicability of both objective and subjective scales in defining the degree of facial paralysis, due to natural facial asymmetries of the evaluated patients, in addition to any differences in the degree of facial paralysis impairment among facial thirds. Thus, besides proposing an instrument to evaluate facial paralysis, new studies should focus on investigating the reliability of the scale proposed, for even with the use of objective scales, measurements are needed, depending on the skill and mastery of the appraiser with respect to the instrument. However, rating scales are valuable tools that help professionals in the diagnosis of clinical cases and that may assist in the clinical workup to be conducted after this evaluation.
Thus, in this study the Chevalier and House & Brackmann scales were found to be reliable assessment tools, and experience with their application makes them even more effective. Further research on the subject, with inclusion of other scales, is needed.
ConclusionThe Chevalier and of House & Brackmann scales are useful for clinical practice, since they exhibit high intra- and inter-rater agreement. The use of instruments of classification for functional impairment is important in scientific circles, and such scales proved to be good tools for the classification of facial paralysis.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Fonseca KM, Mourão AM, Motta AR, Vicente LC. Scales of degree of facial paralysis: analysis of agreement. Braz J Otorhinolaryngol. 2015;81:288–93.
Institution: Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, MG, Brazil.