There is no consensus on duration of the nasal splint after nasal septum surgeries. The pressure of nasal splint on the mucosa may cause tissue necrosis and nasal septum perforation.
ObjectivesTo investigate the histopathological changes of the nasal mucosa caused by nasal splints in a rabbit model.
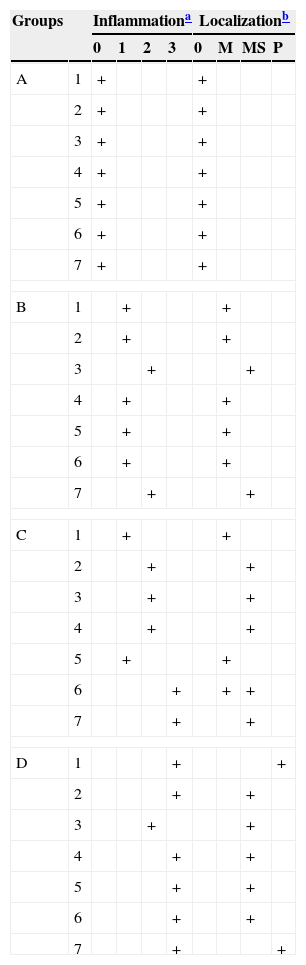
MethodsNo splint was used in group A. Bilateral silicone nasal splints were placed for five, ten, and 15 days in groups B, C, and D, respectively. Biopsy of the nasal mucosa was performed after removal of splint. Histopathologic evaluations were performed. The severity and depth of the inflammation were scored.
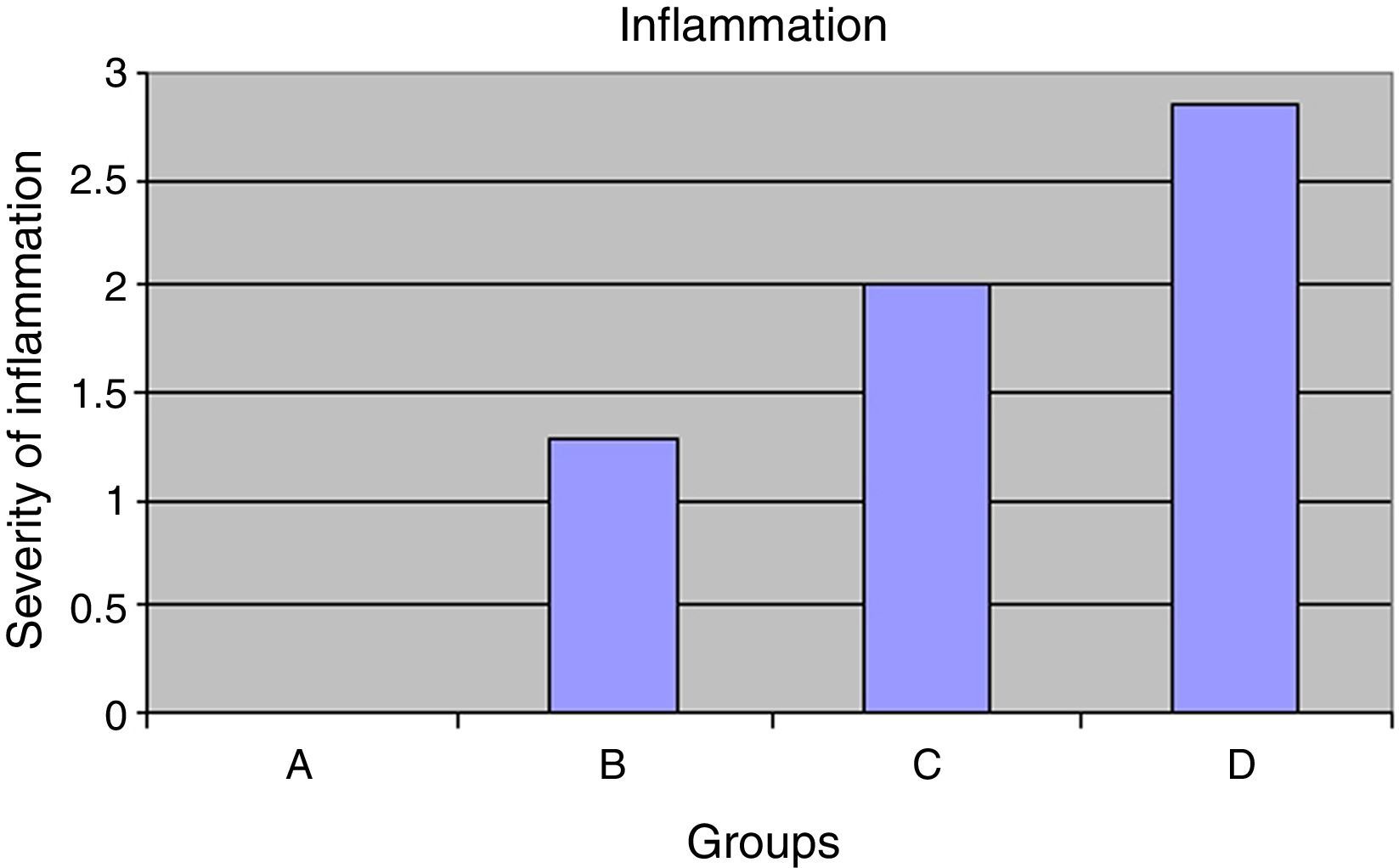
ResultsGroup A had a normal histological appearance. Comparison of the results of groups B, C, and D with group A demonstrated statistically significant differences with regards to the severity of histopathological findings. There was no statistically significant difference between groups B and C. There were statistically significant differences between the groups B and D, and also between groups C and D.
ConclusionsLonger duration of nasal splint had a higher risk for septal perforation. Therefore, removal of the splint as soon as possible may be helpful for preventing potential perforations.
Não existe consenso acerca do tempo de permanência de splints nasais no pós-operatório de cirurgias no septo. A pressão causada pelos mesmos na mucosa nasal pode causar necrose e perfurações septais.
ObjetivosInvestigar mudanças histopatológicas da mucosa nasal causadas por splints nasais em coelhos.
MétodoNenhum splints foi utilizado no grupo A. Splints de silicone foram utilizados por 5, 10 e 15 dias nos grupos B, C e D, respectivamente. Biópsia da mucosa nasal foi realizada após a remoção dos mesmos. Avaliações histopatológicas foram realizadas, e a gravidade e a profundidade do processo inflamatório foram medidas.
ResultadosGrupo A apresentou uma aparência histológica normal. Comparações de resultados entre os grupos B, C e D com o grupo A demonstraram diferenças estatísticas relevantes na gravidade histopatológica. Não houve diferenças estatísticas relevantes entre os grupos B e D, assim como entre os grupos C e D.
ConclusãoDe acordo com os resultados, quanto maior aduração no uso de splints nasais maioro risco de perfuração septal. Portanto, a remoção de splints nasais deve ser realizada assim que possível, prevenindo potenciais perfurações.
Various types of packing are placed into the nasal passages after nasal septum surgeries in order to ensure that the bilateral mucoperichondrial flaps are secured in place. Securing the mucoperichondrial flaps is important to prevent complications such as bleeding or hematoma.1 Placement of packing into the nasal passages between the nasal lateral wall and the septum also prevents potential synechiae. There is no consensus on how long the nasal splint can be kept in place without causing injury to the nasal structures.2
Nasal septum perforation as a post-surgical complication is observed in approximately 0.7–1.4% of patients after septoplasty.3 Nasal septum perforation occurs due to respective mucosal damage, particularly. Such a perforation may be caused by disrupted blood flow originating from the nasal splint pressure on the mucosa and tissue necrosis.
The present study assessed the histopathological changes of the nasal mucosa caused by nasal splint and evaluated the relationship between the duration of nasal packing and septal perforation in a rabbit model.
MethodsThe experimental study was approved by the Experimental Animal Ethics Committee (2011/A39). A total of 28 healthy rabbits with normal anterior rhinoscopic examination were included. Animals were randomly assigned to four equal groups. In the control group (group A), no nasal splint was placed. Nasal packing was placed using bilateral silicone nasal splints sutured with 4-0 silk suture and were held in place for five, ten, and 15 days in groups B, C, and D, respectively, after anesthesia using ketamine hydrochloride 80mg/kg IM (Ketalar 10mL flask, E. Warner Lambert) and xylazine hydrochloride 2mg/kg IM (Rompun 50mL 2% flask, Bayer) combination. After the procedure, metamizole 10mg/kg was administered intramuscularly to relieve pain. The size of nasal splint was approximately 1.5cm×0.7cm diameter.
According to the clinical observations, septal perforation due to the nasal splint was seen on the end portion (proximal) of the splint. Based on this observation, biopsies were obtained 1cm behind the columella, measuring approximately 0.5cm×0.5cm diameter, under anesthesia in the group A at the beginning of the study and in the other groups, after the nasal splint was removed. The biopsy specimen was fixed in a 10% neutral formalin solution and a routine tissue follow-up was performed. It was then embedded in paraffin and cut into 5μm thickness. Hematoxylin–eosin (H–E) stained sections were evaluated under light microscopy by two single-blinded pathologists; all evaluations between the two pathologists were in agreement.
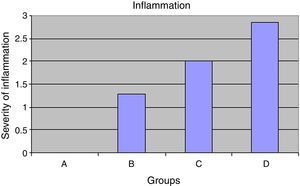
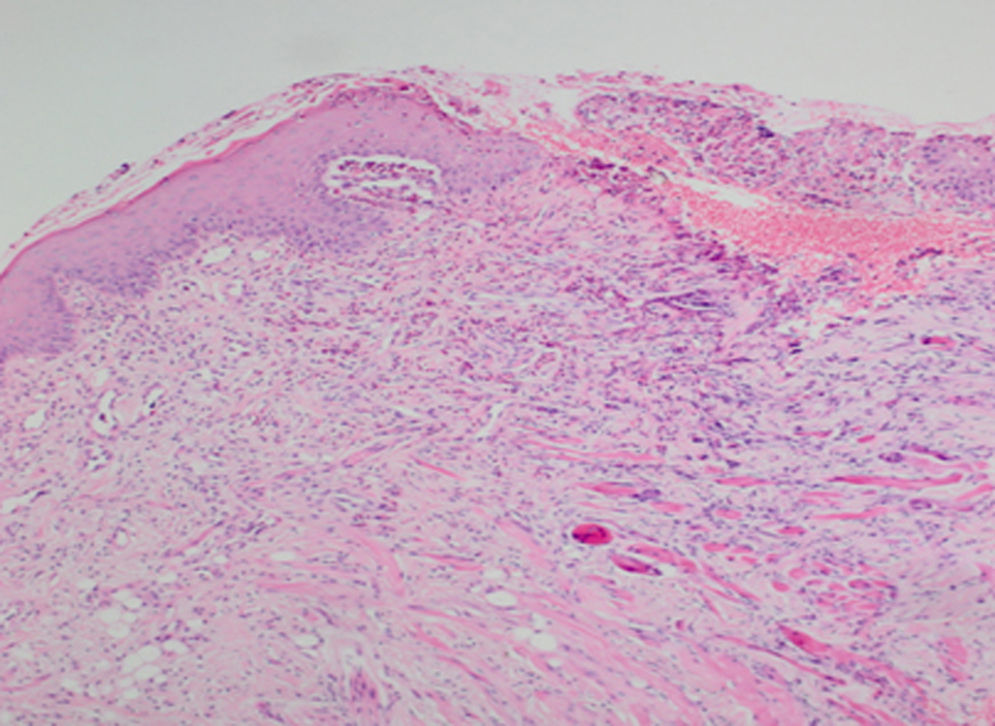
The surface of normal septal mucosa was lined by respiratory epithelium, with hyaline cartilage, which consists of vessels and connective tissue under the submucosa. The findings were compared with normal mucosal pattern and scored from 0 to 3, based on the presence and character of inflammation (acute or chronic inflammation), mucosal erosion, ulceration, and perforation. The acute inflammation was shown by neutrophil prepotency with rare eosinophils. Also, the severity of the inflammation was scored by the number of inflammatory cells in a 400× magnification area (no inflammatory cells [0]; less than 10 inflammatory cells, mild1; 10–30 inflammatory cells, moderate2; and over 30 inflammatory cells, severe3). Histomorphological changes were scored as: normal histology, limited only to the mucosa, involving the submucosa, and mucosal ulcerations and/or perforations.
SPSS 17.0 was used for statistical evaluation. The Kruskal–Wallis test was used to compare all groups, and the Mann–Whitney U test was used for comparing two groups.
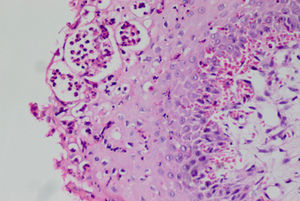
ResultsInflammatory and histopathologic changes observed in the groups are shown in Table 1. The control group (group A) had a normal histological appearance (Fig. 1). There was no inflammation in the group A. In the group B, there was mild inflammation involving the mucosa in five animals, and moderate inflammation that extended to the submucosa in two animals (Fig. 2). The average severity of the inflammation was 1.28 for the group B (Fig. 3).
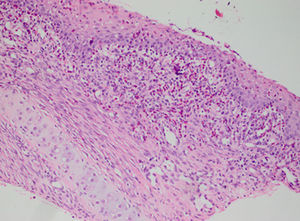
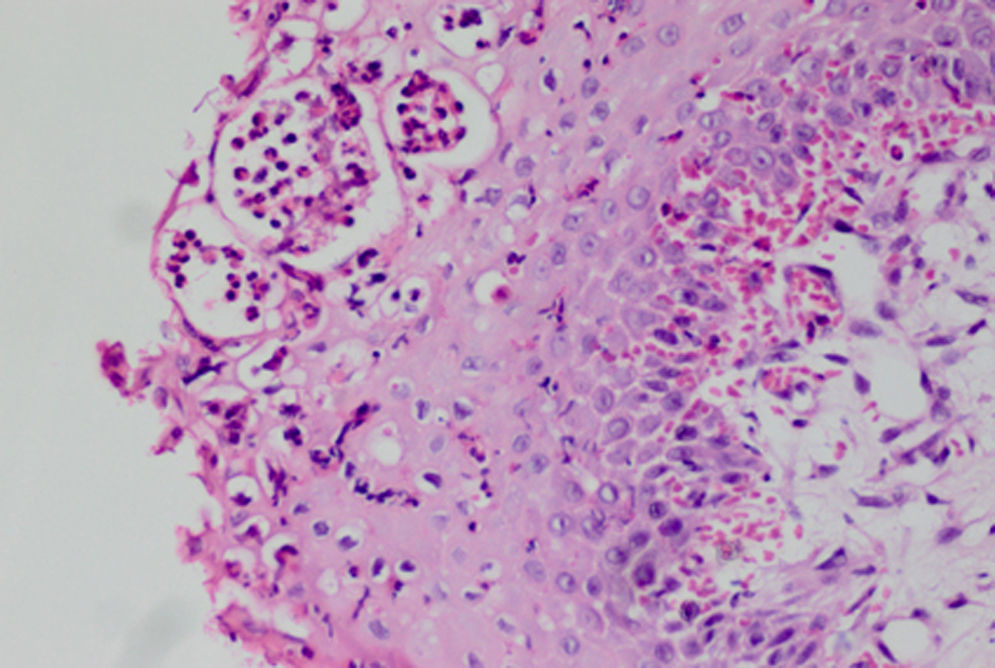
In group C, mild inflammation involving the mucosa was found in two animals, moderate inflammation extending to the submucosa in three animals, and severe inflammation extending the submucosa in two animals (Fig. 4). Increased inflammation was seen in the group C compared to group B.
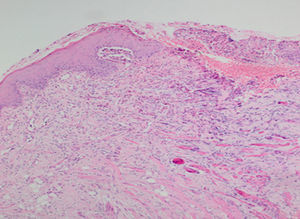
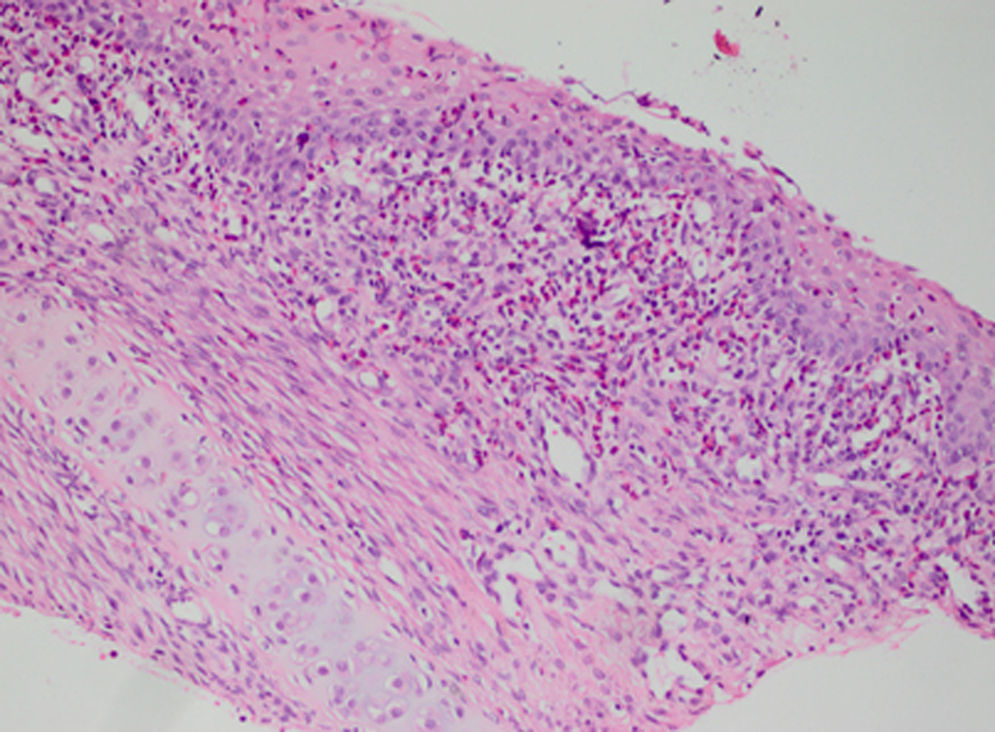
In group D, there was severe inflammation extending to the submucosa in four animals (Fig. 5). One animal was found to have moderate inflammation extending to the submucosa. In two animals, severe inflammation presented with perforations and ulcerations. The average severity of the inflammation was 2.85 (Fig. 3). There was increased inflammation compared with group C.
The results showed that there was a statistically significant difference in the severity of histomorphological findings between the group A and the other groups (groups B, C, and D).
There was no statistically significant difference on the severity of histomorphological findings between group B and C (p>0.05). However, statistically significant differences in the severity of histomorphological findings between groups B and D, and groups C and D (p splint) held for the longest time and macroscopic perforations were seen in two animals in this group.
DiscussionSeptoplasty, septorhinoplasty, and endoscopic sinus surgery are commonly performed surgical methods by ear, nose, and throat, and plastic surgeons. Various types of nasal packing are used both to prevent nasal bleedings and/or septal hematomas, and also to support fenestrated parts until they are healed with fibrin, especially in septoplasty and septorhinoplasty.1 Nasal packing used in these surgeries affects function of the nose and comfort of the patient. However, there has been no consensus achieved on the duration, indications, and type of nasal packing.2,4
Nasal packing may cause various problems such as nasal septal perforations,5 pyogenic granulomas,6 life-threatening toxic shock syndromes,7 obstructive sleep apneas,8 reduced oxygen saturation and increased pulse rates,9 pains,10,11 and necrosis of the inferior turbinate.5 Changes in the ear pressure associated with nasal packing were also found.12 It has been accepted that the duration of nasal packing potentially influences the development of these complications. The use of nasal packing after septal surgery is still under discussion. In order to avoid the complications of nasal packing, trans-septal suturing techniques have been adopted instead of packing, and various comparative studies have been conducted in this respect. In one such study, Ardehali et al.11 compared patients who received nasal packing with patients who received trans-septal suturing after surgery and found no significant differences for the rate of hematoma, perforations, and synechiae. Camirand et al.13 reported that they did not use any type of nasal packing after the surgery and documented no complications, such as epistaxis, synechiae, hematoma, or septal perforations, similar to the findings of Lemmens et al.14
Genc et al. investigated the effects of nasal packing moistened with vaseline-nitrofurazone against trans-nasal suturing techniques on the septum of rabbits by evaluating the histopathological changes of packing on nasal mucosa.15 The packing was held in the nose for 48h. Increased mucosal inflammation was observed in both techniques, and no statistical significance was found when compared to the control group. McIntosh et al.16 caused wounds on the nasal mucosa on an animal model, then applied Merocel® as packing material to the one side and left the other side without packing. The packing was removed on the fifth day, and no histopathological difference in the re-epithelization and ciliary functions of the nasal mucosa was found between the two groups. This study suggested that holding the packing in place for extended periods followed by endoscopic sinus surgeries has no effects on the recovery of the mucosa. Against these studies, the present study found significant increased inflammation scores even if the nasal packing was kept in the nose for five days. It is suggested that this finding could be due to necrosis as a result of mucosal pressure. Necrosis on the cartilage was observed in group D, where the packing was held for the longest time in our study. In addition, perforation was observed in two animals in this group. Nasal septal perforation may be related with the hypoxemic–ischemic necrosis of the cartilage as a result of pressure.
Maccabee et al. investigated the histopathological effects of nasal packing on paranasal sinus mucosa.17 They placed Merocel® into the maxillary sinuses of rabbits and collected biopsies after their removal two weeks later. They observed that the epithelial and mucociliary activity fully disappeared in the mucosa, with an advanced stage of fibrosis at the basal lamina and lamina propria. They found that the Merocel® fibers were incorporated into the regenerated epithelium, observing lymphocyte infiltration. The finding of their study showed that holding the nasal packing in place for extended periods would result in severe fibrosis resulting in loss of the entire epithelial layer is similar to the findings of the present study. However, it is impossible for the silicone nasal packing used in the present study to be introduced into the regenerated epithelium. The use of nasal packing is expected to disrupt ciliary activity, which is one of the most important elements of nasal epithelium. Shaw, in his study on the nasal mucosa of sheep, showed that the ciliary surface on the nose was reduced by 50–68% by intranasal packing.18 Another study compared the mucociliary activity by rhinoscintigraphy following septum suturing of nasal packing, and found no meaningful differences. Also, no pre- and post-operative differences were found.19 In the present study, epithelial inflammation was observed at the lowest level in the group in which the nasal packing was removed at an early stage. Likewise, it is anticipated that early removal of nasal packing contributes positively to the ciliary function.
The knowledge of how long a frequently used material can be held in a specific region and which problems may arise during this period has potential to contribute to the more efficient use of that material. There has been no consensus on how long nasal packing should be held in the nose. To address issue, most of the ear, nose, and throat surgeons and source books have recommended the removal of packing at 48h and beyond. In a controlled study by Jiannis et al., 75 patients were treated by septoplasty, and the packing was held in place for 24h in one group, and 48h in another group.20 They scored the patient comfort during this time using a visual analog scale. They found that the patient comfort was poorer in the group where the packing was held in place for 48h. The same study found no differences for postoperative complications of bleeding and pain, also reporting that the group where the packing was held for 48h had higher fever. They recommended the removal of the packing in the shortest time possible. However, they made no mention of its effects on nasal mucosa in their study. This finding is in support of the present finding that the packing should be removed quickly. In another study, no statistically significant differences were found for hemorrhagic complications between maintenance of the packing for 24h or 48h.4
There has been no consensus on how long the packing used after nasal surgery should be held in the nose, and the type of packing to be used. No studies, except for a study by Lubianca et al.4 regarding the duration of nasal packing in the nose, were found in the literature. This study also reported that there were no statistical differences for hemorrhagic complications between the placement of 24-h packing and 48-h packing. Ensuring that patients can quickly return to their work and resume their daily social activities after the surgery is an important criterion used to assess the success of operations. However, despite short hospitalization after nasal operations, extended duration of the nasal packing seriously disrupts the patient's comfort.
ConclusionAfter nasal splint, the inflammation of the nasal mucosa and the risk for septal perforation increased as the nasal splint was kept in place longer. Conceivably, there could be a correlation between septal perforation and the duration of nasal splint after septoplasty.
Conflicts of interestThe authors declare no conflicts of interest.
The research was supported by the Research Fund of the Inonu University, Malatya, Turkey.
The authors would like to thank Ms. Nazire Bulam, a biostatistics expert from the Turgut Ozal Medical Center Medical Center, who contributed to statistical evaluations of this study.
The authors would also like thank Seckin Ulualp, M.D., from the Department of Otolaryngology-Head and Neck Surgery University of Texas Southwestern Medical Center Dallas, Texas, USA, for his assistance with editing the manuscript.
Institution: Istanbul Medeniyet University, School of Medicine, Turkey.
Please cite this article as: Tan M, Kalcioglu MT, Sahin N, Bayindir T, Samdanci E, Filiz A. Assessment of mucosal changes associated with nasal splint in a rabbit model. Braz J Otorhinolaryngol. 2015;81:184–9.



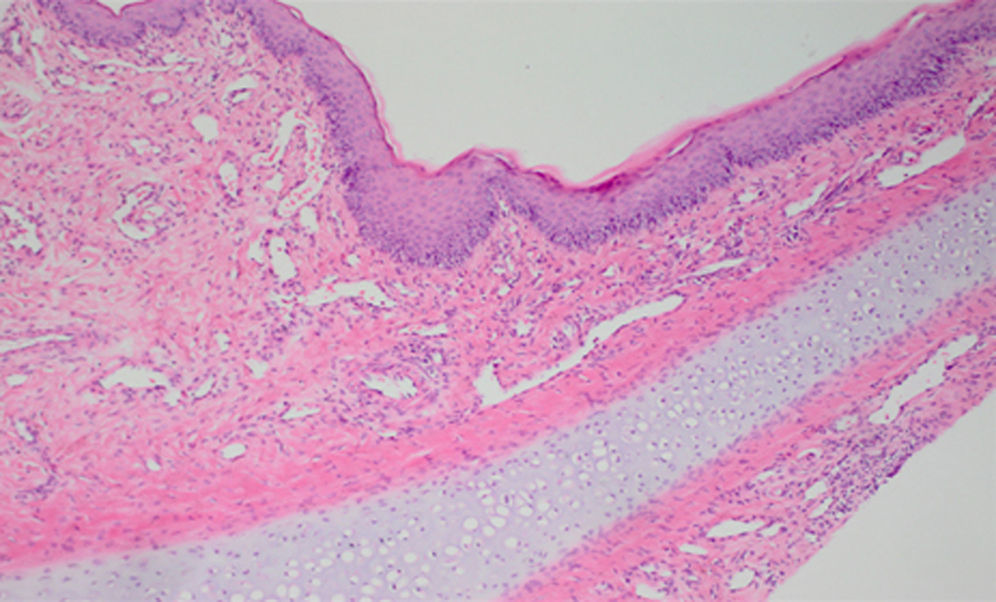
![Normal histological appearance (hematoxylin–eosin [H–E] 100×). Normal histological appearance (hematoxylin–eosin [H–E] 100×).](https://static.elsevier.es/multimedia/18088694/0000008100000002/v2_201503250422/S1808869414001025/v2_201503250422/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/7hLX2FbBoxC1192i158SI=)