Cartilage graft tympanoplasty has a better success rate in the treatment of chronic otitis media if regularly prepared and placed.
ObjectiveTo prepare cartilage island material and evaluate its effect on the success rate of tympanoplasty.
MethodsThe medical records of 87 patients (48 males and 39 females; mean age, 27.3±11.2 years; range, 14–43 years) with chronic otitis media without cholesteatoma who underwent intact canal-wall-up tympanoplasty and revision surgery between December of 2007 and October of 2011 were retrospectively evaluated. Surgery was performed under general anesthesia via a retroauricular approach.
ResultsThe overall success rate of this technique was 93% in terms of perforation closure. No graft lateralization or displacement into the middle ear occurred. The overall average preoperative air bone gap was 37.27±12.35dB, and the postoperative air bone gap was 27.58±9.84dB. The mean postoperative follow-up period was 15.3 months (range: 7–21 months).
ConclusionIf cartilage graft is properly prepared and placed, cartilage graft tympanoplasty appears to provide better success rates and hearing results.
A timpanoplastia de enxerto de cartilagem tem uma melhor taxa de sucesso no tratamento de otite média crónica se for preparada e colocada de forma sistemática.
ObjetivoPreparar o material de enxerto de cartilagem “em ilha” e avaliar o seu impacto na taxa de sucesso da timpanoplastia.
MétodoOs registos médicos de 87 pacientes (48 do sexo masculino e 39 do sexo feminino; idade média 27.3±11.2 anos; intervalo 14-43 anos) com otite média crónica sem colesteatoma que foram submetidos a timpanoplastia de levantamento de parede do canal intacto e cirurgia de revisão entre Dezembro 2007 e Outubro 2011 foram avaliados em retrospetiva. A cirurgia foi realizada sob anestesia geral através de uma abordagem retro auricular.
ResultadosA taxa de sucesso global da nossa técnica foi de 93% em termos de sutura da perfuração. Não ocorreu lateralização do enxerto nem deslocação para o ouvido médio. O intervalo aéreo-ósseo pré-operatório médio global (ABG) era de 37.27±12.35dB e o ABG pós-operatório era de 27.58±9.84dB. O período médio de seguimento pós-operatório era de 15.3 meses (intervalo 7-21 meses).
ConclusãoSe o enxerto de cartilagem for devidamente preparado e colocado, a Timpanoplastia de enxerto de cartilagem apresenta melhores taxas de sucesso e resultados ao nível da audição.
The aim of tympanoplasty is to close tympanic membrane perforations, restore hearing, and reconstruct a healthy middle ear cavity. Although tympanoplasty is a highly successful procedure in 70–90% of normally ventilated middle ears, the prognosis is poorer in cases with total dysfunction, adhesive processes, infection, tympanic fibrosis, and defect of the entire tympanic membrane.1,2 Many autogenous, several allogenous (homogeneous), and a few xenogenous graft materials have been used for ear drum perforation closure and reconstruction of the middle ear and ear canal.3
The major advantage of cartilage is its stiffness and bradytrophic metabolism, which make it particularly suitable for difficult conditions, such as subtotal perforations, adhesive otitis, and reoperation.4
The aim of the present study was to prepare the cartilage island graft material and to evaluate its effect on the success rate of tympanoplasty.
MethodsA retrospective study was performed on 87 patients undergoing tympanic membrane repair for tympanic membrane perforations between December of 2007 and October of 2011. All the patients had chronic otitis media without cholesteatoma.
Age, gender, size of perforations, primer or revision surgery, time between both tympanoplasties for revision cases, preoperative and postoperative pure-tone average air bone gap (PTA-ABG), and average time of follow-up were obtained for all patients.
Surgical techniqueThe cartilage island method for tympanoplasty was performed under general anesthesia using a postauricular approach. Graft materials were harvested from conchal perichondrium, and the preferred cartilage was conchal cartilage due to its concave shape and its ease of acquisition using the postauricular approach. The cartilage is stripped 0.2mm from the edge circumferentially using a blade (No. 15). Wedge resection of cartilage from the peripheral to the central region of the graft for placement of the malleus handle by leaving the perichondrium was performed (Fig. 1). The perichondrium is placed medial to the remnant tympanic membrane or tympanic annulus. The long handle of the malleus was placed into the wedge resected area of the graft using a lock-and-key approach to stabilize the graft.
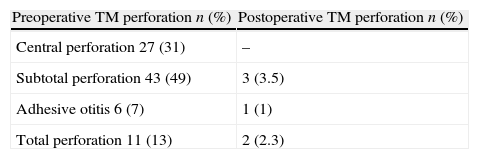
ResultsThe mean age of the 87 patients (48 males and 39 females) was 27.3±11.2 years (range, 13–40 years). Twenty-seven patients had benign central perforations, 43 had subtotal perforations, six had adhesive tympanic membranes, and ten had total perforations (Table 1). Eleven ears were drained during surgery. Seventeen patients were revision cases. The previous tympanoplasties had been performed in another hospital. All of them were first revision cases. Temporalis fascias were used in their first operation. The overall average preoperative ABG was 37.27±12.35dB, and the postoperative ABG was 27.58±9.84dB. The mean postoperative follow-up period was 15.3 months (range, 7–21 months). The time between the failed tympanoplasty and revision tympanoplasty was 10–23 months.
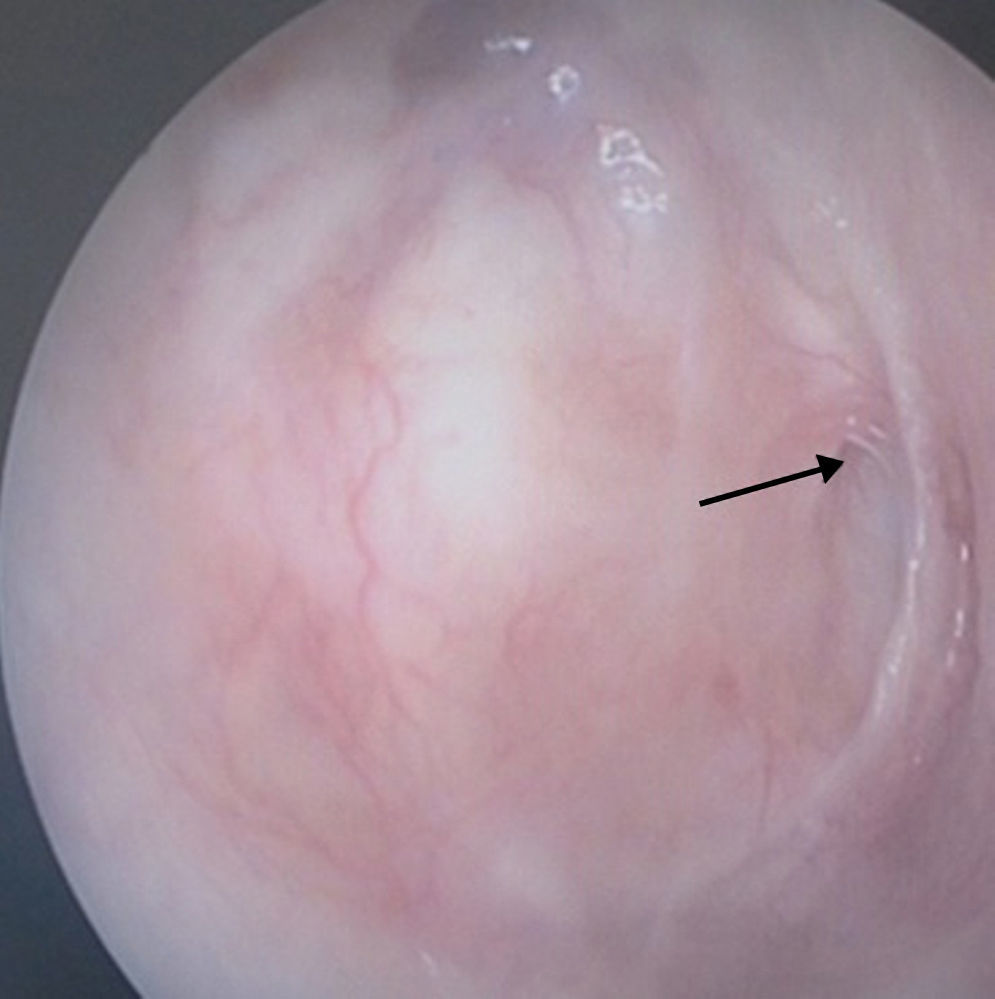
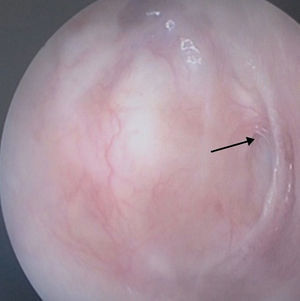
The conchal cartilage underlay graft resulted in a 93% take rate with an intact repair. No graft had lateralized or displaced into the middle ear. No retraction pocket occurred during the follow-up period. Fig. 2 presents the anatomical result of a graft 12 months after the operation. Postoperative results included six patients with postoperative perforations between the remnant tympanic membrane and cartilage part of the graft. Fig. 3 shows a representative image of a perforated graft seven months postoperatively.
Recurrent perforations were all smaller than the initial perforations and occurred in three patients with subtotal perforations, in one patient with an adhesive membrane, and in two patients with total perforations (one revision; Table 1).
DiscussionRecently, temporal muscle fascia has been the most commonly used graft material for tympanoplasty surgery, and the success rate is nearly 90% for closure of the tympanic membrane.5,6 Causes of tympanoplasty failure using a temporal muscle fascia graft included severe ear pathologies, pathology of the malleus handle and stapes arch revision surgery, atelectasis, cholesteatoma, tympanosclerosis, large (>50% of total tympanic membrane diameter) and anterior perforations, tobacco smoke exposure, perforation drainage during surgery, and bilateral disease.7,8 Since the temporal muscle fascia is composed of irregularly arranged elastic fibers and fibrous connective tissue, the postoperative dimensions of the graft are usually unpredictable.9 A more rigid, and more resorption- and retraction-resistant graft material, may provide better success rates. Therefore, cartilage graft materials are preferred for large perforations, and they presented better graft take results than temporalis muscle fascia tympanoplasty.
After the description of cartilage grafts in 1962 by Heerman, many authors have described the palisade and perichondrium island technique for patients with atelectasis, perforations, and cholesteatoma.10–13 The main advantage of cartilage tympanoplasty is that epithelization may continue over the cartilage surface even if the graft detaches anteriorly. The other advantage is that this technique avoids synechia formation between the graft and promontorium, because there is no need to use a sponge in the middle ear to support the graft. A cartilage graft has been thought have a very low metabolic rate. It receives its nutrients by diffusion, is easy to work with because it is pliable, and resists deformation from pressure variations. In the present study, the conchal cartilage was harvested with its posterior perichondrium and the cartilage that is stripped 0.2mm from all around the graft by leaving the perichondrium. The perichondrium is then placed medial to the tympanic membrane or tympanic annulus. In this technique, wedge resection of cartilage from the peripheral to medial region of the graft (for malleus handle) was performed by leaving the perichondrium, and the malleus handle was placed into this area using a lock-and-key approach to stabilize the graft.
Neumann et al.4 reported a graft take rate of 100% in their palisade cartilage tympanoplasty study, and they did not observe resorption or recurrent defects of the rebuilt tympanic membrane. Khan et al.14 used a shield-sliced tragal cartilage-perichondrium composite graft, and their success rate was 97.67%. Sismanis et al.15 reported their revision tympanoplasty cases, and their success rate was 93.5%. In the present study, the success rate of the technique was 93%. Neither graft lateralization nor collapse into the middle ear space occurred in the present patients. Although the thickness of the graft decreased the middle ear space, no significant adverse effect in hearing was observed.
Although the graft-take success rate is high in cartilage tympanoplasty, hearing gain might not be satisfactory due to its effect on tympanic membrane elasticity. However, despite the belief of many surgeons, recent studies have shown that no statistically significant difference exists in temporalis fascia and cartilage tympanoplasties in terms of postoperative hearing results.5,6,16–21 Dornhoffer6 reported an ABG value of 6.8dB for cartilage tympanoplasty. Gerber et al.5 found the average improvement in the air condition threshold to be 10dB. Additionally, Bozdemir et al.22 reported better hearing results in temporalis fascia grafting than conchal cartilage grafting. In the present study, satisfactory hearing results were observed. This result may be due to increased stabilization by thinning of the cartilage part of the graft.
In the early postoperative period, six graft perforations were observed. These perforations were between the remnant tympanic membrane and cartilage part of the graft. Sismanis et al.15 reported that two of three of their graft failures were secondary to residual middle ear cholesteatomas, and these occurred in the attic. Tek et al.23 reported three graft failures in cartilage tympanoplasty, and they were anterior perforations.
Many authors have suggested that cartilage tympanoplasty provides sufficient structural stability during times of negative middle ear pressure and readily resists continued Eustachian tube dysfunction.24 Altuna et al.24 reported that their cartilage tympanoplasty is very effective in revision cases and demonstrated acceptable success rates for grafting and hearing results in high-risk perforations. Their graft success rate was 87%. Additionally, the perforations of their cases were small and due to malposition of the cartilage. In the present study, only one revision case showed graft failure, occurring in the anterior part of the graft and between the remnant membrane and cartilage part of the graft. Kaziktas et al.1 found the graft success rate to be 95.7% in palisade cartilage tympanoplasty and 75% in temporal muscle fascia tympanoplasty. In the present study, the graft was taken in 40 (93%) of 43 patients with subtotal perforations.
The present experience with conchal cartilage tympanoplasty demonstrates that the procedure is very effective, particularly in total perforations, atelectasis, isolated tympanic membrane perforations, and wet perforation drainage during surgery.
ConclusionCartilage island tympanoplasty is an effective procedure for all types of tympanoplasty patients. It provides better graft take and hearing results if it is properly prepared and placed.
Conflicts of interestThe authors declare no conflicts of interest.
The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/fMdJps.
Please cite this article as: Yurttas V, Yakut F, Kutluhan A, Bozdemir K. Preparation and placement of cartilage island graft in tympanoplasty. Braz J Otorhinolaryngol. 2014;80:522–6.