Patients with dentofacial deformities may benefit from orthognathic surgery in the maxilla. Maxillary osteotomy may include procedures in the bone, cartilaginous, and soft tissues of the nose, leading to shape alterations.
ObjectiveTo evaluate the anatomic alterations of the nasal region in patients undergoing a Le Fort I osteotomy for advancement or superior impaction.
MethodsThis is a clinical prospective study. Twenty-one patients were evaluated during the pre- and postoperative periods. The positioning of the nasal tip and the modification of the nasal base were evaluated.
ResultsThe results showed that the nasal tip was superiorly positioned in 85% of the cases, advanced in 80%, rotated in 80%, and there was a wide nasal base in 95%, resulting in esthetic improvement.
ConclusionsSurgeries of maxillary advancement and superior reposition tend to cause elevation and advancement of the nasal tip, as well as enlargement of the nasal base.
Pacientes com deformidades dento-faciais podem ser beneficiados pela cirurgia ortognática na maxila. A técnica cirúrgica da osteotomia da maxila inclui também procedimentos realizados na parte óssea e cartilaginosa e tecidos moles do nariz o que pode provocar mudanças na forma.
ObjetivoEste trabalho teve como proposta avaliar as mudanças anatômicas da região nasal, decorrentes de cirurgias maxilares pela osteotomia Le Fort I para avanço e/ou impacção.
MétodoTrata-se de um estudo clínico prospectivo. Foram incluídos 21 pacientes, submetidos à cirurgia e avaliados antes e 6 meses após o ato cirúrgico em relação aos movimentos da ponta nasal e modificações da base do nariz.
ResultadosOs resultados mostraram mudanças da ponta nasal para cima em 85% dos casos, para anterior em 80%, rotação em 80% e alargamento da base nasal em 95%, promovendo melhorias estéticas.
ConclusãoCirurgias de avanço e reposicionamento superior da maxila tendem a causar elevação e avanço da ponta do nariz, assim como, um alargamento da base nasal.
Dentofacial deformity can be defined as any condition where the facial skeleton differs from the accepted normal, with malocclusion and altered facial appearance. Orthognathic surgery is indicated for the correction of these deformities, aiming to achieve functional and esthetic recovery. The surgery, when associated with orthodontic procedures, improves masticatory function and facial appearance, with a stable result from the occlusal point of view, and is the best form of treatment for patients with dental and skeletal problems.1
Patients with dentofacial deformities represent approximately 20% of the population and may exhibit varying degrees of functional or esthetic impairment.2 These malformations can occur in only one maxilla, extend to multiple craniofacial structures, or appear unilaterally or bilaterally, as well as occurring at different degrees in the vertical, horizontal, or transverse head planes.
According to the extent of the problem, surgery varies from small mobilization of groups of teeth to full mobilization of the mandible and maxilla. Orthognathic surgery is indicated when all growth factors are finished and orthodontic treatment is no longer sufficient to maintain a balance between teeth and bone.2 The goal of these treatments, surgical and orthodontic, is the correction of dentofacial deformities and the balance of teeth, bone structure, and soft tissue for improved function and better facial appearance.
Le Fort I-type osteotomy of the maxilla includes procedures performed in bone, cartilage, and soft tissues of the nose that can cause changes in nasal shape and function, which sometimes are unpredictable.3
Therefore, the aim of this study was to evaluate the nasal shape by cephalometric study in patients undergoing orthognathic surgery for maxillary advancement and/or impaction through Le Fort I osteotomy.
MethodsAll patients underwent maxilla advancement and/or impaction surgery through Le Fort I technique under general anesthesia, without segmentation, for correction of horizontal and vertical deformities. Before surgery the patients underwent a pre-operative planning phase and pre-surgical orthodontic treatment, which continued after the surgery. They were assessed pre- and postoperatively (six months). Patients with syndromes or cleft palate were excluded. All participants who agreed to participate signed an informed consent.
The surgical technique consisted of a standard maxillary vestibular incision, from the midline to the 2nd molar, performed bilaterally, followed by tissue dissection and subperiosteal detachment to expose the lower orbital ridges and malar prominence with infraorbital nerve preservation. The osteotomy was initiated with a surgical reciprocating saw in the greatest concavity of the piriform recess, horizontally, past the zygomatic pillar. Thin chisels were used to complete the osteotomies of the lateral nasal wall and nasal septum, and a strong curved chisel was used to perform the palatal-pterygoid disjunction.
Mobilization of the maxilla was then performed caudally with manual manipulation to verify its mobility. Rowe forceps were employed to complete maxillary repositioning. The maxilla was positioned according to the surgical guide or, in Class I occlusion of patients, with maxillo-mandibular fixation using steel wire. The osteosynthesis of the maxilla was performed using four 1.5-mm “L” plates with five orifices, pre-shaped to the desired advancement and positioned on the canine and zygomatic pillars.4,5 The measurement of the maxillary impaction extent was performed from the incisal border of incisor teeth to a fixed point on the glabella.
Measurements of the nasal width and displacement of the nasal tip were used to evaluate nasal shape in the pre and postoperative periods (six months). The width was obtained by measuring the most lateral point of the nostrils, using a caliper.
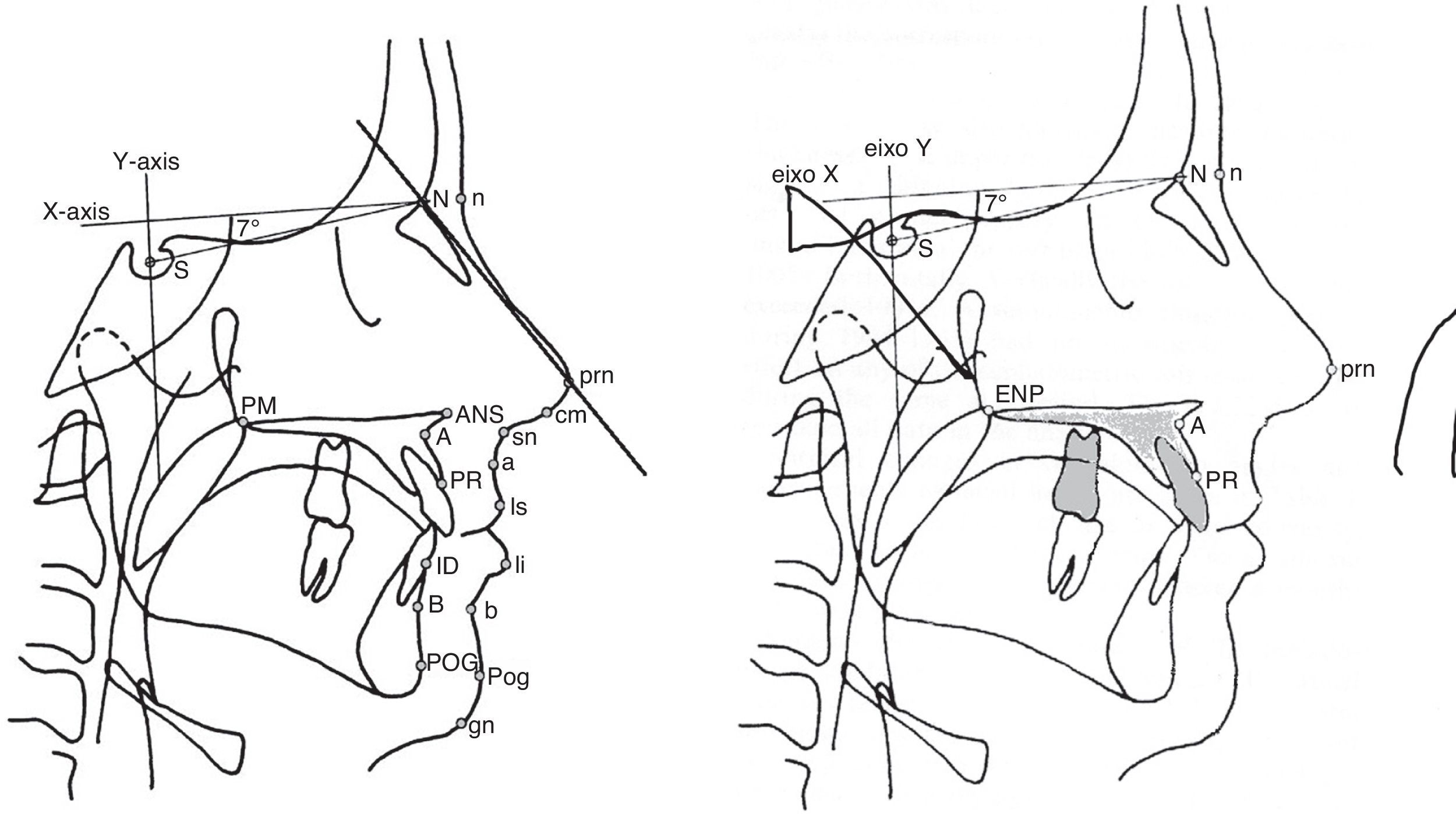
Bone mobilization and the modification of the nasal tip after surgery were measured using cephalometric radiography in pre- and postoperative profile, which was performed by the same professional and analyzed three times, with a period of one month between each; there was agreement in 90% of cases. Subsequently, tracings were performed on the radiographs, based on Heliovaara et al.6 (Fig. 1), which were then compared to observe the changes in soft tissues. For that purpose, the lateral cephalometric radiographs were performed using standardized method, obtained with the patient positioned in the Frankfurt plane, with occluded molars and lips at rest, preoperatively and six months after surgery.
Schematic demonstration of the cephalometric points employed, based on Heliövaara et al.6
After obtaining the radiographs, a cephalogram was created, adapting an 18cm×24cm sheet of ultraphan paper and then, with a 0.5 pencil, anatomical structures and landmarks were traced on the light box. The S point (center of sella), N point (nasion), the SN lines; the X axis (horizontal line starting at point N, ascending 7° of the SN line); Y axis (vertical line perpendicular to the horizontal line passing through the S point) were traced in this cephalogram, corresponding to structures that are not altered by surgery, which serve as reference for movement analysis of the structures altered by surgery.
Then maxillary landmarks were identified: PNS (posterior nasal spine), A (deepest point in the anterior contour of the maxillary alveolar arch), and the PR point (prosthion – the most anterior–inferior point of the upper dentoalveolar margin). Postoperative maxillary position was obtained by the distances between X, Y, and the PNS axes; X, Y, and A axes; and X, Y, and PR axes. Changes in soft tissues were evaluated using the PRN point (most anterior point of the nasal tip), measuring the distance between this point and the reference lines X and Y and the SnPrn angle (Fig. 1). Statistical analysis consisted of box-plot and paired Student's t-test, with significance set at 5%.
The study was approved by the University Ethics Committee (178/02).
ResultsIn the present study, the sample consisted of 20 patients (12 women and men). The mean age was 21.4 years (minimum 14 and maximum 37). Twenty patients had class III skeletal deformities.
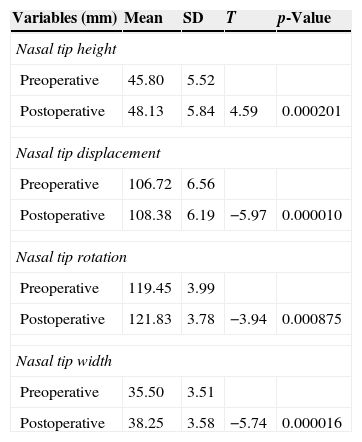
There was an elevation of the nasal tip in 85% of patients, an advancement of the nasal tip in 80%, an increase in the rotation angle of the nasal tip in 80%, and increased nasal width in 95% (Table 1).
Student's t-test for nasal height, displacement, and rotation; and nasal base width.
| Variables (mm) | Mean | SD | T | p-Value |
|---|---|---|---|---|
| Nasal tip height | ||||
| Preoperative | 45.80 | 5.52 | ||
| Postoperative | 48.13 | 5.84 | 4.59 | 0.000201 |
| Nasal tip displacement | ||||
| Preoperative | 106.72 | 6.56 | ||
| Postoperative | 108.38 | 6.19 | −5.97 | 0.000010 |
| Nasal tip rotation | ||||
| Preoperative | 119.45 | 3.99 | ||
| Postoperative | 121.83 | 3.78 | −3.94 | 0.000875 |
| Nasal tip width | ||||
| Preoperative | 35.50 | 3.51 | ||
| Postoperative | 38.25 | 3.58 | −5.74 | 0.000016 |
SD, standard deviation.
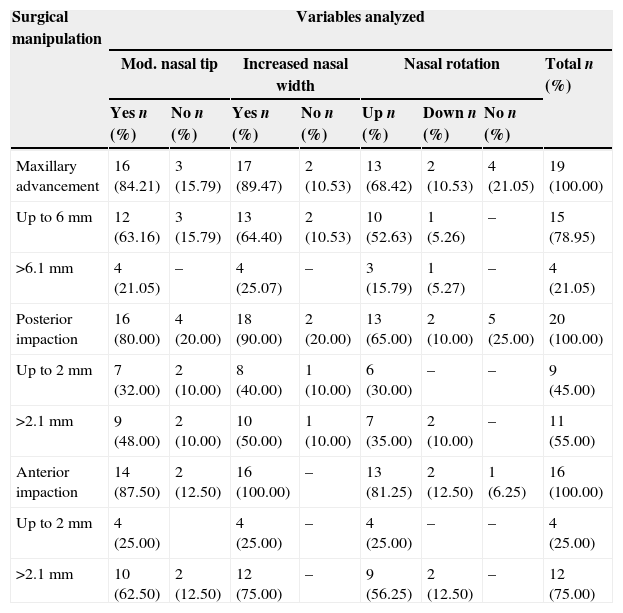
In most cases, there were modifications in the nasal tip, increased nasal width, and upward nasal rotation, according to the amount of maxillary advancement, and anterior or posterior impaction (Table 2).
Modification of the nasal tip, increased nasal width, and nasal rotation according to surgical manipulation.
| Surgical manipulation | Variables analyzed | |||||||
|---|---|---|---|---|---|---|---|---|
| Mod. nasal tip | Increased nasal width | Nasal rotation | Total n (%) | |||||
| Yes n (%) | No n (%) | Yes n (%) | No n (%) | Up n (%) | Down n (%) | No n (%) | ||
| Maxillary advancement | 16 (84.21) | 3 (15.79) | 17 (89.47) | 2 (10.53) | 13 (68.42) | 2 (10.53) | 4 (21.05) | 19 (100.00) |
| Up to 6mm | 12 (63.16) | 3 (15.79) | 13 (64.40) | 2 (10.53) | 10 (52.63) | 1 (5.26) | – | 15 (78.95) |
| >6.1mm | 4 (21.05) | – | 4 (25.07) | – | 3 (15.79) | 1 (5.27) | – | 4 (21.05) |
| Posterior impaction | 16 (80.00) | 4 (20.00) | 18 (90.00) | 2 (20.00) | 13 (65.00) | 2 (10.00) | 5 (25.00) | 20 (100.00) |
| Up to 2mm | 7 (32.00) | 2 (10.00) | 8 (40.00) | 1 (10.00) | 6 (30.00) | – | – | 9 (45.00) |
| >2.1mm | 9 (48.00) | 2 (10.00) | 10 (50.00) | 1 (10.00) | 7 (35.00) | 2 (10.00) | – | 11 (55.00) |
| Anterior impaction | 14 (87.50) | 2 (12.50) | 16 (100.00) | – | 13 (81.25) | 2 (12.50) | 1 (6.25) | 16 (100.00) |
| Up to 2mm | 4 (25.00) | 4 (25.00) | – | 4 (25.00) | – | – | 4 (25.00) | |
| >2.1mm | 10 (62.50) | 2 (12.50) | 12 (75.00) | – | 9 (56.25) | 2 (12.50) | – | 12 (75.00) |
Regarding the soft tissues of the nasal region, a decrease in the X-Prn axis distance measurement was observed from the pre- to the postoperative period, indicating an elevation of nasal tip in 85% of cases. After comparing the pre- and postoperative measurements of the Y-Prn axis, an increase of this distance was observed between the two evaluations, indicating that advancement of the nasal tip was observed in 80% of cases.
After comparing the measurements of the SnPrn angle pre- and postoperatively, there was an increase in the measurement of the angle, indicating an upward rotation of the nasal tip in 80% of cases, downward rotation in 10%, and no rotation of the nasal tip in 10% of patients. The measurement of postoperative nasal width increased in 95% of cases.
DiscussionThe correction of dentofacial deformities through orthognathic surgery aims to provide a more functional maxilla-mandibular relationship and, consequently, improve the patient's facial harmony.
Le Fort I osteotomy is indicated for the mobilization of the maxilla in the three spatial planes, allowing the correction of several deformities. In the present study, this treatment was used for maxillary advancement and impaction in patients with class II and III deformities.7–11 All patients had postoperative alterations in the nasal region, which is in agreement with the literature.3
Maxillary superior repositioning and advancement can cause nasal tip elevation and augmentation of the alar base.6 Regardless of the amount of maxillary advancement, and anterior or posterior impaction, in most cases there was modification of the nasal tip, increased nasal width, and upward nasal rotation. A probable explanation for this fact is that there was a new positioning of the anterior nasal spine and, with the dissection of soft tissues, the standard preoperative measures were partially lost, generating slight distortions.
Bimaxillary surgery5 may be a good option when the anteroposterior discrepancy is greater than 8mm, which was not the case in the present study. Aydil et al.5 reported that a Le Fort I surgery together with mandibular sagittal osteotomy, when indicated for mandibular advancement, significantly affected the vertical and anteroposterior position of the maxilla and mandible, respectively. When performed in combination, these surgical techniques can efficiently change the position of the upper incisors and nasal position in both the vertical and anteroposterior directions. Bimaxillary orthognathic surgery seems to be an efficient method to obtain satisfactory results in the appearance of soft, dental, and skeletal tissues, associated with facial profile in patients with high angle Class II skeletal deformity.
Araújo1 compared cephalometric points in pre- and postoperative lateral radiographs, observing that in maxillary advancement surgeries, the most anterior point of the nose is changed horizontally by 30%, and if the alar base suture is performed, it may reach 35%. Regarding the findings of this experiment, a mean ratio of 40% was observed among patients who underwent surgery, although some patients demonstrated a very different result, either higher or lower (0–90%), as all patients also underwent repositioning of the upper maxilla and alar base suture, with 3-0 prolene suture, fixing the inner region of the right and left alar bases, while the lip was sutured using conventional sutures or V-Y, according to the patient's facial type; this aspect is very important in order for the patient to have a nose that is proportional to the rest of the face, resulting in a more harmonious appearance.
The maxilla can be impacted in most cases without compromising airflow.12,13 The enlargement of the anterior nasal area, reducing air resistance even after the nasal skeleton is reduced, may explain the significant improvement in nasal breathing after maxillary impaction.14,15 Even if there is gain in the anterior nasal area due to anterior mobilization of the maxilla after surgery, the authors agree with Bottini et al.4 regarding the non-performance of rhinoplasty at the time of orthognathic surgery to correct pre-existing defects, such as a dorsal hump, a very broad or very narrow nasal base, a deviation of the nasal pyramid, or other cosmetic defects resulting from the orthognathic surgery.
The establishment of the developmental stage and bone growth is of utmost importance for the correct diagnosis, planning, and treatment of individuals, particularly those who are at the pubertal growth stage.16 A carpal radiography can be used for this type of diagnosis. The patient in this study, a 14-year-old female, underwent surgery after being assessed by an endocrinologist, when her wrist radiographs were reviewed, upon which it was observed that she was already in the final stage of growth.
Some aspects of the surgical technique may interfere with nasal breathing and shape, such as removal of the bony and cartilaginous septum to prevent interference and deviations in the maxilla, removal of hypertrophied turbinates, expansion of the piriform aperture in patients with a long face in order to increase the nasal cavity, and suture of the nasal base.2
Considering these aspects, it is mandatory to interview the patient pre- and postoperatively to discover what their actual esthetic and functional expectations are, as well as to explain the possible appearance outcomes of orthognathic surgery.
ConclusionSurgeries of advancement and superior repositioning of the maxilla tend to cause elevation and advancement of the nasal tip, as well as enlargement of the nasal base.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Dantas WR, da Silveira MM, Vasconcelos BC, Porto GG. Evaluation of the nasal shape after orthognathic surgery. Braz J Otorhinolaryngol. 2015;81:19–23.
Institution: Universidade de Pernambuco (UPE), Recife, PE, Brazil.