First branchial cleft anomalies account for 8–10%1,2 of all branchial cleft defects, representing approximately 17% of all pediatric cervical masses. The low incidence and the various clinical presentations of these congenital malformations of the branchial apparatus make the diagnosis difficult even for the experimented otolaryngologist. Depending on the type of the anomaly (fistula, sinus or cyst), the fistulous tract can be located medial or lateral to the facial nerve. CT scans provide useful information on the location of the fistulous tract.
We report a rare case of type II first branchial cleft fistula presenting as a tract with 2 openings – a cervical opening in the left submandibular region and a small fistulous opening at the floor of the cartilaginous portion of the left external auditory canal (EAC). Treatment consisted in complete excision of the fistulous tract and superficial parotidectomy with preservation of the facial nerve.
Case reportA 4 year-old girl presented in the ENT clinic with a left upper neck mass that was first noticed 6 months ago. The parents’ interrogatory revealed that during acute rhinopharyngitis episodes the mass became red and swollen, and a whitish, recurrent discharge leaked both from a small opening in the left laterocervical region and from the left EAC. Clinical examination showed that the mass was ovoidal, measuring 2.5–1cm, fluctuant and relatively mobile on deep cervical structures. A small cutaneous opening was noticed in the left submandibular region.
Otoscopy revealed a small depression on the floor of the left EAC with an intact tympanic membrane.
CT scans showed a fistulous tract connecting the cartilaginous portion of the left EAC to the upper laterocervical region that crossed the deep parotid lobe. The diagnosis of first branchial cleft fistula was made.
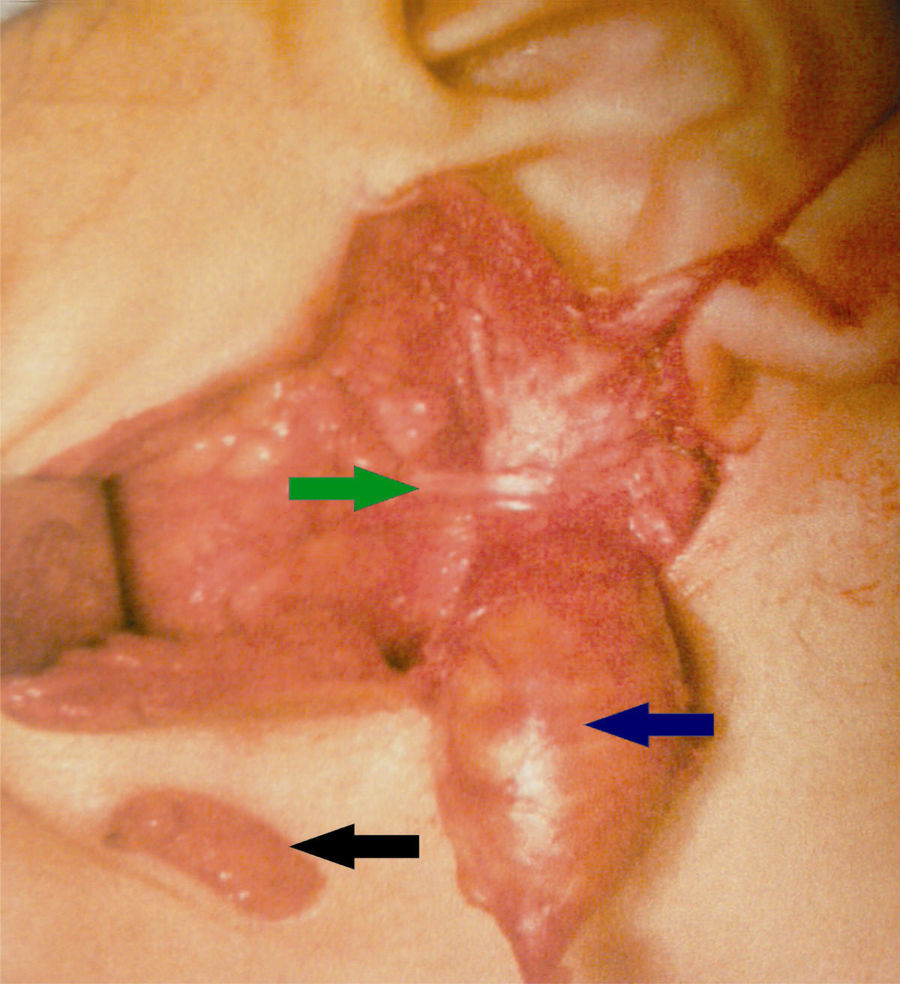
Under general anesthesia, the fistulous tract was excised using a classic parotidectomy incision described by Adson and Ot in 1923 and modified by Redon in 1955. Because of the distance between the incision and the inferior cutaneous opening of the fistula, an elliptical excision of the opening was also performed (Fig. 1).
After the identification and dissection of the facial nerve trunk, we performed a superficial parotidectomy and discovered the fistulous tract lying under the facial nerve branches. The fistulous tract was excised along with the inferior cutaneous opening, taking care to preserve the branches of the facial nerve. Finally, the superior opening of the fistula was excised together with a small portion of the cartilaginous floor of the left EAC.
The postoperative care was uneventful. Histological examination of the specimen revealed that the fistulous tract was lined by squamous epithelium with adnexal structures and cartilage disposed in hyaline lamellae, thus confirming the diagnosis of type II first branchial cleft fistula.
DiscussionAnomalies of first branchial cleft are rare entities resulting from incomplete closure of the ectodermal portion of this cleft. The first description of these anomalies dates back from 1865 (Virchow). In 1929, Hyndman and Light gathered 108 cases from the medical literature.
In 1971, Arnot classified the anomalies of the first arch and first branchial cleft in: type 1 anomalies (encountered mostly in adults), consisting in a pretragal cyst draining in the parotid area, and type 2 anomalies (usually developing during childhood), appearing in the anterior cervical triangle.
The histological classification was made by Work: type I – ectodermal origin of the anomaly (squamous epithelium), and type II – ectodermal and mezodermal origin (squamous epithelium, adnexial structures and cartilage). Type I anomaly presents as an epidermoid cyst or fistula located in the periaural region, with a fistulous tract parallel to the EAC that ends in a cul-de-sac at the level of the mesotympanum. Type II lesions present as a cyst, sinus (tract with an external opening), a fistulous tract with a superior opening at the level of the bony–cartilaginous junction of the EAC or a combination of these elements. The inferior opening of type II lesions (as in our case report) is situated in a triangular area described by E. Poncet that is bounded by the EAC above, the mental region anteriorly and the hyoid bone inferiorly.3 It is also important to know that type II anomalies are situated above the vascular structures of the neck and the digastric muscle, but their position regarding the facial nerve is variable, with the nerve situated above, below or even crossed by the lesion.
Finally, in a third classification Olsen divided the defects as cysts, sinuses or fistulas.
The analysis of clinical manifestations (cervical – usually a little depression near the mandibular angle; parotid – small masses located in the parotid area, and auricular – otorrhea and sometimes a membranous attachment between the floor of the EAC and the tympanic membrane – 10% of the cases in the series of Triglia), cervical and parotid area CT scans or MRI and the fact that these lesions are rarely associated with other facial malformations can lead to the diagnosis of first branchial cleft anomalies. In children, differential diagnosis includes congenital ear cysts, preauricular tags and second branchial cleft anomalies.
Concerning our case, the location of the cervical mass, its characteristics, the otoscopic findings along with CT scans provided solid elements in favor of the diagnosis.
It is generally admitted that fistulas are often located medial to the nerve, whereas sinus tracts tend to run lateral to it.4,5 Based on these observations, we performed a complete surgical excision of the fistulous tract together with the superficial parotid lobe, because of the position of the mass (below the facial nerve). This particular situation of the anomaly explains the difficulty of this kind of surgery, in which facial nerve damage can occur (40% in the series of Ford2 and 15% in the series of Triglia).
We must insist on the fact that there is a second problem concerning the complete excision of these lesions without damaging the nerve, and that is in relationship with the child's age: the younger the patient, the mastoid tip is not completely developed and the facial nerve tends to have a more superficial position as it arises from the stylomastoid foramen. In this case, facial nerve monitoring becomes a must in finding the nerve's trunk and in performing a safe dissection of its branches.6
Also, the risk of iatrogenic facial palsy during the surgical removal of the tumor is higher if there is a history of recurrent infections and inadequate treatment (incision, drainage or incomplete excision) that may lead to intensive scarring. Fortunately, in our case, the diagnosis was early because the general practitioner promptly referred the patient to the ENT clinic and there were no previous attempts to remove the lesion, thus minimizing the risk of scarring.
Concerning the upper portion of the fistulous tract, it is essential to remove a small cartilage portion of the EAC along with the fistulous opening to prevent its recurrence. In our case, we could approach the margins of the superior opening after the excision without causing a secondary stenosis of the EAC.
ConclusionCongenital malformations of the first branchial cleft region represent entities that an otolaryngologist might encounter during practice. We highlight a case of this rare pediatric pathology and its management, recommending general practitioners and clinicians to be aware of the consequences of misdiagnosing it or delaying the surgical treatment. A thorough knowledge of the embryology of the cervicofacial region ensures an early diagnosis and a complete surgical excision of these lesions, minimizing the risk of serious complications such as permanent facial nerve palsy.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Codreanu CM, Codreanu C, Codreanu M. First branchial cleft fistula: a difficult challenge. Braz J Otorhinolaryngol. 2017;83:364–6.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.