Vertebral artery dissection (VAD) is an important differential diagnosis in patients with vertigo, and can be confused with vestibular migraine. VAD can cause stroke in young patients, and its estimated incidence is 1–1.5/100,000/year.1
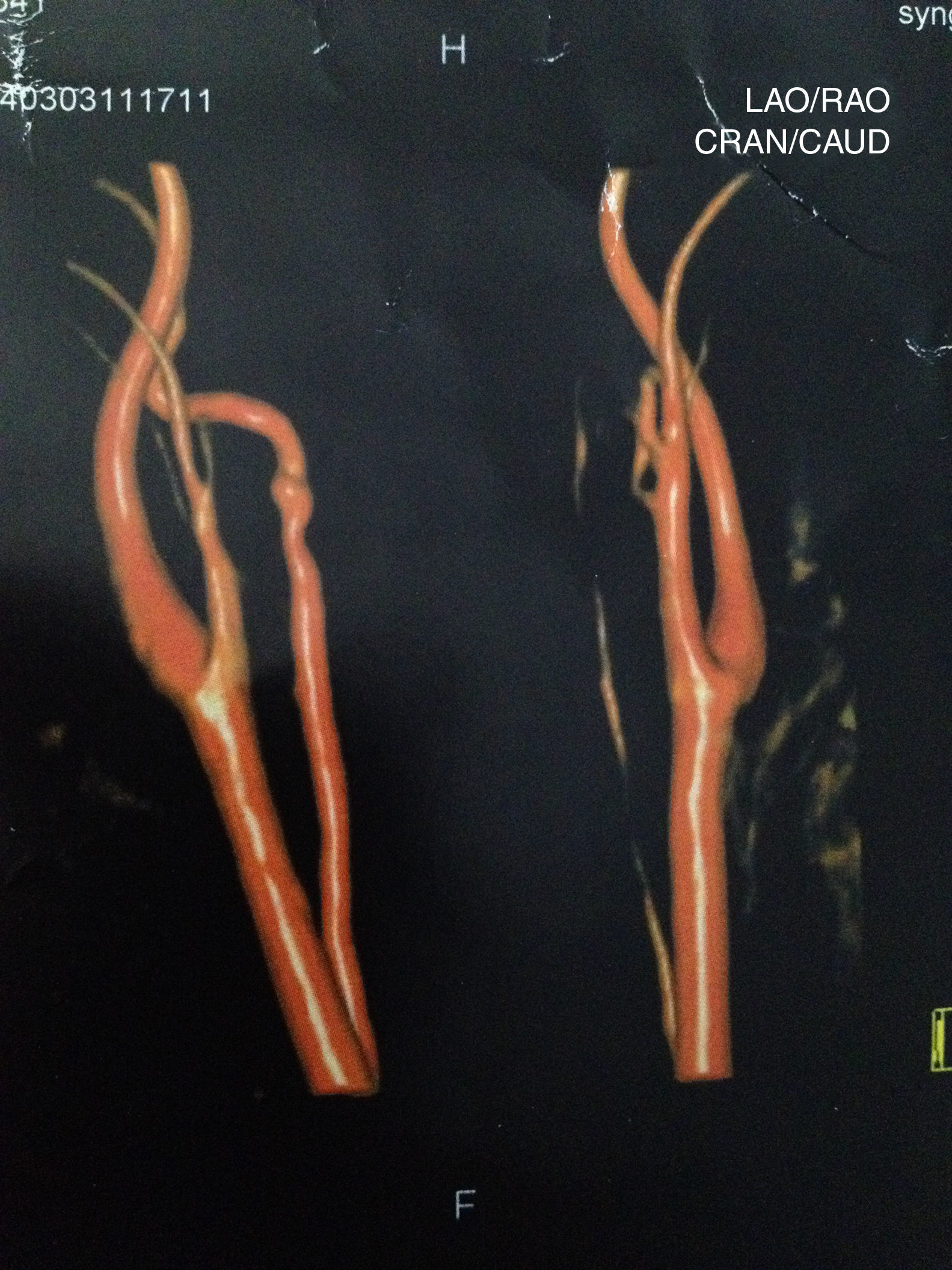
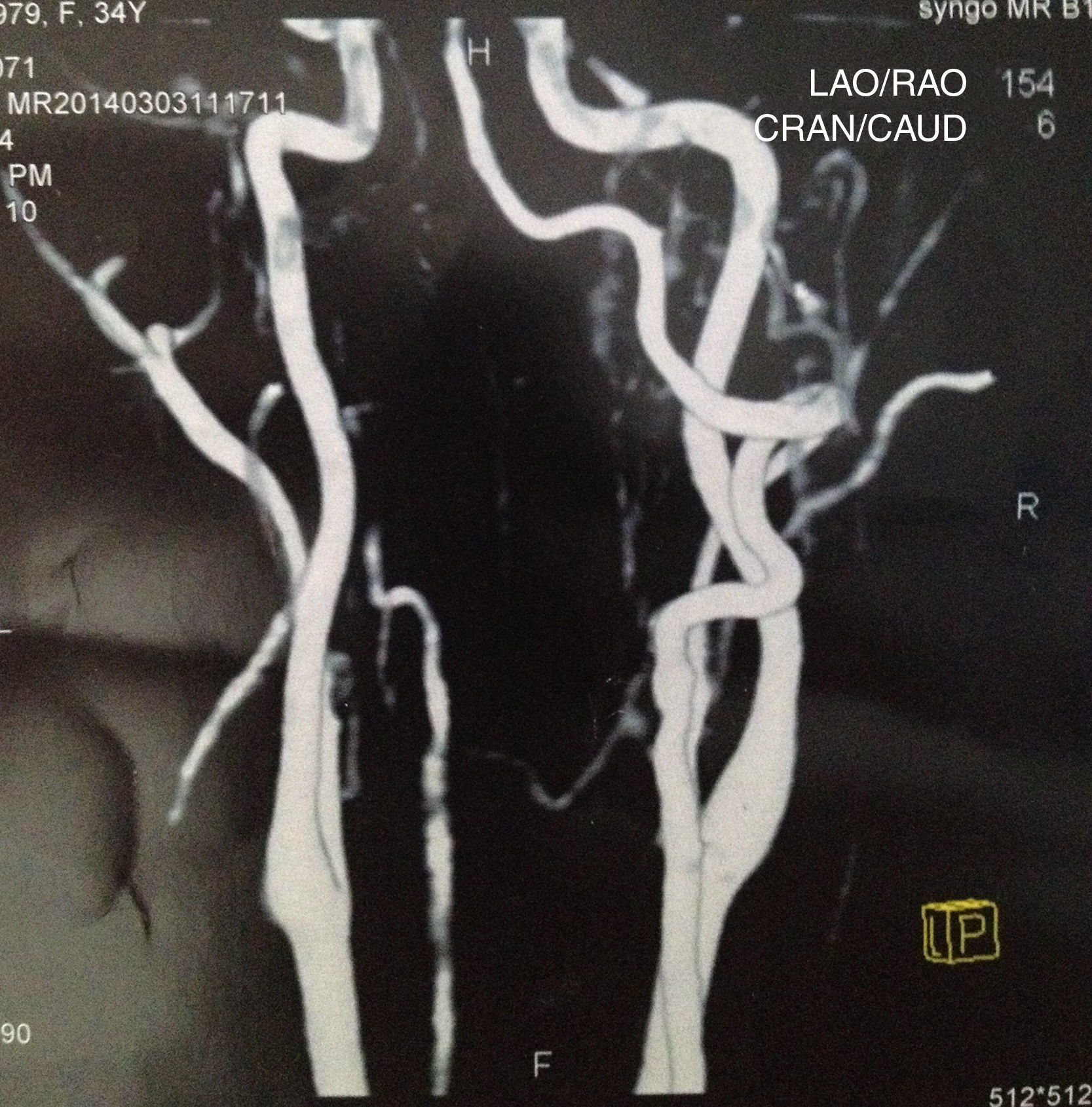
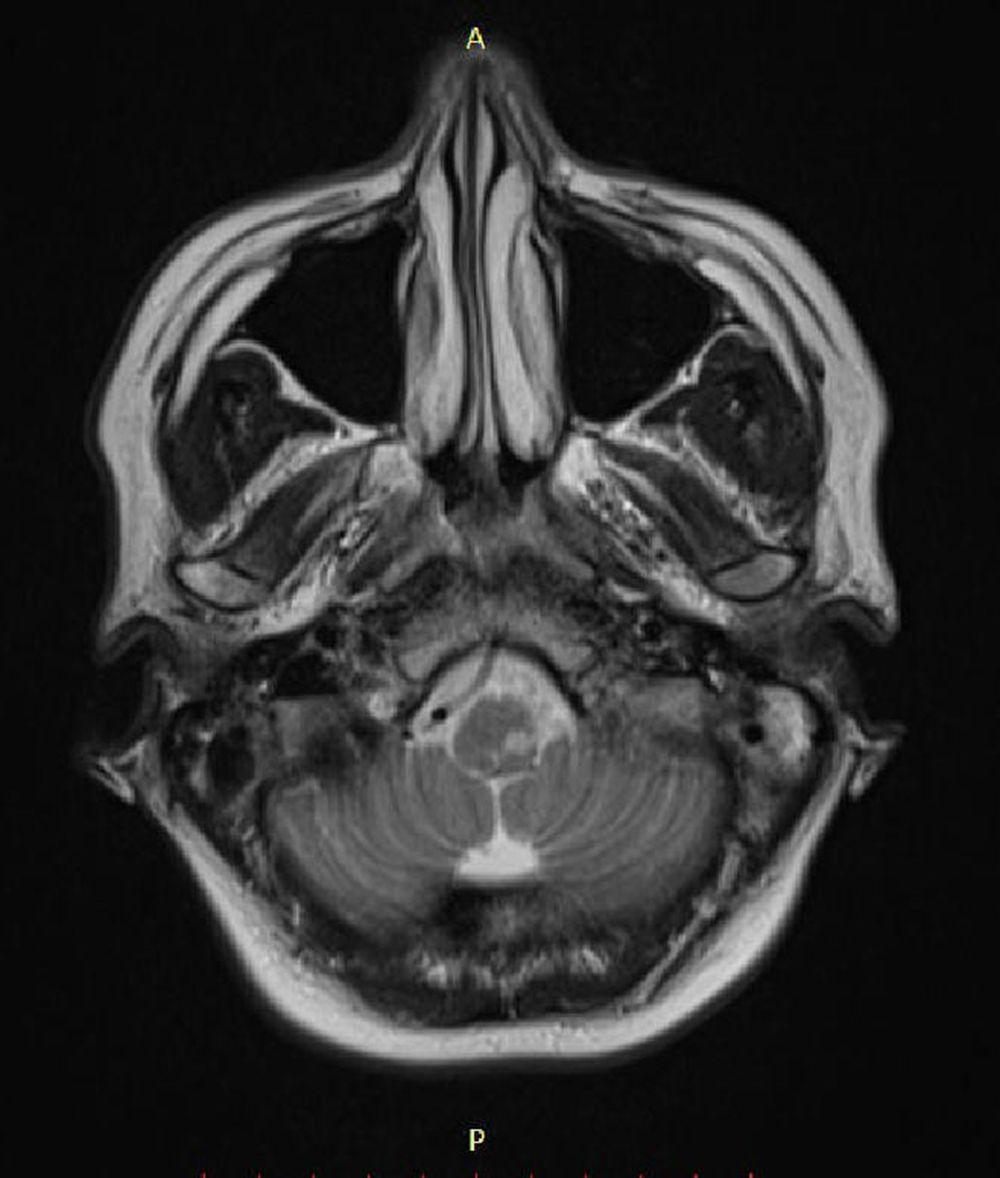
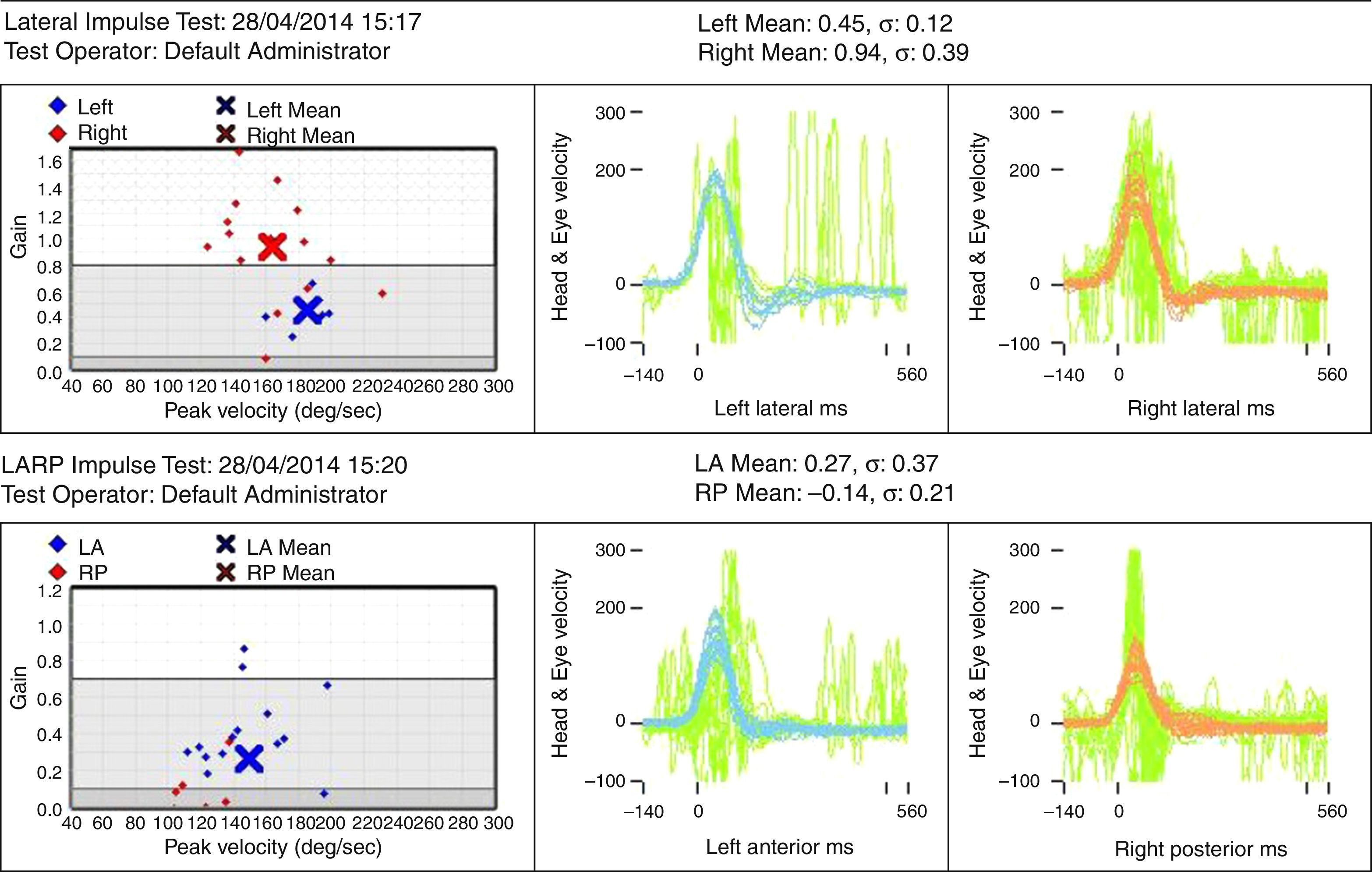
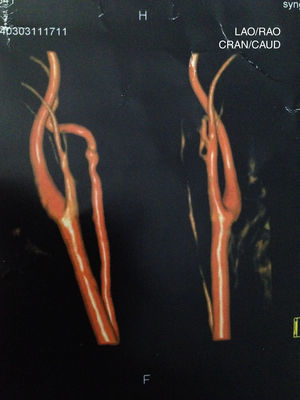
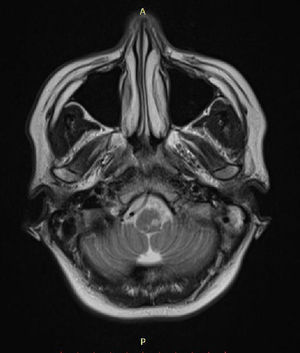
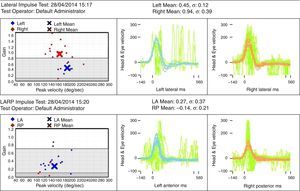
Case reportSV, female, 34, reported high-intensity, stabbing left temporal headache with continuous occipital and posterior cervical radiation, which had started two days before. In the preceding day, the patient experienced disabling vertigo and vomiting that worsened with head movement. The patient went to the hospital where her condition partially improved with the use of anti-vertigo and painkiller medications. A computed tomography of her head was obtained and was interpreted as normal and the patient was released with a presumptive diagnosis of vestibular migraine. Hours later, her problem evolved with diplopia, dysphagia, dysphonia, difficulty coughing, and oscillopsia; the patient returned and was admitted to the hospital. She had a history of hypothyroidism and migraine (eight years before, the patient suffered a pulsatile-type frontal headache in her premenstrual period, which stopped with the use of common painkiller drugs), and was taking oral contraceptives. She had no history of cervical trauma. At admission, her physical examination revealed a broad-based slow gait and left-side ptosis, enophthalmos, and miosis, with an arrhythmic pattern, and horizontal spontaneous nystagmus to the right. Cerebellar tests indicated severe dysmetria and eudiadocokynesis. Tactile hypoesthesia in the left facial hemisphere and right hemibody were observed; this latter finding was associated with thermal hypoesthesia. No change in muscle strength was noted. Magnetic resonance angiography of the carotid and vertebral arteries was obtained, showing left vertebral artery dissection (VAD) with posterior inferior bulb infarction (Figs. 1–3). The search for autoimmune disease through autoantibody survey and for infectious diseases (human immunodeficiency virus, syphilis, and cultures) was negative. The video head impulse test suggested hypofunction with lesser lateral- and left anterior-channel gain (Fig. 4). Anticoagulation with full-dose enoxaparin was initiated during hospitalization, later replaced by warfarin, and resulted in a slow and gradual clinical improvement. The patient was discharged after 18 days of hospitalization. Three months after her hospital discharge, the patient was receiving vestibular rehabilitation and daily physical therapy, with progressive improvement in motor skills. She is currently walking unassisted, but with slight imbalance.
Connective tissue diseases and trauma are risk factors for VAD, but such occurrences are absent in most patients, requiring strong clinical suspicion for their diagnosis.1
The association with migraine is well documented; migraine can act as a predisposing factor for nontraumatic VAD. It is postulated that repeated episodes of migraine could cause the involved arteries to become vulnerable to dissection.2
In a systematic review, vertigo was the most common symptom, present in 58% of cases of VAD, followed by headache and neck pain, which were the initial symptoms in 67% of cases.1 The vertebral artery can nourish the cervical anterior spinal artery; an association between VAD and cervical cord ischemia has been described.3
The present case is characteristic of Wallenberg syndrome, caused by the occlusion of the posterior inferior cerebellar artery, usually as a result of VAD, in which the patient presents with dysphagia, dysphonia through involvement of the nucleus ambiguous of the vagus, vertigo, sensory changes in the face, ipsilateral Horner and cerebellar syndromes, and thermal and algic hemianesthesia of contralateral body.4
The treatment for VAD consists of anticoagulation, except in patients with intracranial involvement, due to the risk of subarachnoid hemorrhage. Instituted early, anticoagulation improves the prognosis, which emphasizes the importance of early diagnosis.1,2 Due to possible adverse effects of anticoagulants, in many cases, preference is given to the use of antiplatelet agents.2 The CADISS study was the first randomized clinical trial to compare antiplatelet versus anticoagulant treatment for extracranial cases of carotid and vertebral artery dissection. After three months of treatment, no differences were detected between groups regarding death or stroke.5
Stroke was diagnosed in 63% of cases, with the highest prevalence in patients with extracranial dissection; subarachnoid hemorrhage was observed in 10% of cases, all of them with intracranial VAD, probably due to the long course of the artery through the subarachnoid space.1 Studying bulbar infarction, Kim et al. stated that VAD was responsible for 9.2% of the cases, and that 34.5% of these cases had been caused by large-vessel atherosclerosis, that has been blamed as the primary etiology.6 Most cases of VAD have a good progression, with a poor prognosis in only 10% of patients.1
ConclusionAs this is a potentially treatable cause of stroke, VAD should be considered in patients with vertigo and craniocervical pain, even in those without risk factors. Early diagnosis is critical for the early institution of anticoagulation to provide the best opportunity for an improved prognosis.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Rocha M, Nakao BH, Manoel EM, Moussalem GF, Ganança FF. Vertebral artery dissection: an important differential diagnosis of vertigo. Braz J Otorhinolaryngol. 2017;83:367–9.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.