The complexity of the nasal tip structures and the impact of surgical maneuvers make the prediction of the final outcome very difficult. Therefore, no single technique is enough to correct the several anatomical presentations, and adequate preoperative planning represents the basis of rhinoplasty.
ObjectiveTo present results of rhinoplasty, through the gradual surgical approach to nasal tip definition based on anatomical features, and to evaluate the degree of patient satisfaction after the surgical procedure.
MethodsLongitudinal retrospective cohort study of the medical charts of 533 patients of both genders who underwent rhinoplasty from January of 2005 to January of 2012 was performed. Cases were allocated into seven groups: (1) no surgery on nasal tip; (2) interdomal breakup; (3) cephalic trim; (4) domal suture; (5) shield-shaped graft; (6) vertical dome division; (7) replacement of lower lateral cartilages.
ResultsGroup 4 was the most prevalent. The satisfaction rate was 96% and revision surgery occurred in 4% of cases.
ConclusionThe protocol used allowed the implementation of a gradual surgical approach to nasal tip definition with the nasal anatomical characteristics, high rate of patient satisfaction with the surgical outcome, and low rate of revision.
A complexidade das estruturas da ponta nasal e o impacto de manobras cirúrgicas sobre o seu suporte dificultam a previsão da forma final da mesma. Devido a isso, nenhuma técnica isolada é suficiente para corrigir adequadamente as numerosas apresentações anatômicas, sendo o planejamento pré-operatório, a base da rinoplastia.
ObjetivosApresentar resultados de rinoplastias, por meio da abordagem cirúrgica gradativa para definição da ponta nasal baseada nas características anatômicas, e avaliar o grau de satisfação dos pacientes após a realização do procedimento cirúrgico.
MétodoEstudo em coorte histórica longitudinal no qual foram avaliados os prontuários de 533 pacientes de ambos os gêneros submetidos à rinoplastia no período de Janeiro de 2005 a Janeiro de 2012. Os pacientes foram divididos em sete grupos: (1) Nenhuma cirurgia na ponta nasal; (2) Divulsão interdomal; (3) Ressecção cefálica; (4) Sutura domal; (5) Enxerto em escudo; (6) Divisão vertical dos domus; (7) Reconstrução das cartilagens alares maiores.
ResultadosO grupo 4 foi o de maior prevalência. A taxa de satisfação foi de 96% e a revisão cirúrgica ocorreu em 4% dos casos.
ConclusãoO protocolo utilizado permitiu a associação da abordagem cirúrgica gradativa para definição da ponta nasal com as características anatômicas nasais, alta taxa de satisfação com o resultado cirúrgico e baixa taxa de revisão.
The nasal tip is the most challenging part of rhinoplasty. The complexity of its structures, such as the cartilage elements arranged in a variable fashion and positioned against gravity, the relatively poor blood supply and variable skin thickness, as well as the impact of surgical maneuvers on the support of the tip makes it difficult to predict its final shape.1
The evaluation of nasal tip can be studies its definition, projection, and rotation, in addition to its length. Several mathematical formulas and rules have been described, in attempts to define the ideal characteristics of the nasal tip.2,3 Moreover, the thickness and texture of the skin and subcutaneous tissue envelope have a significant impact on the degree of definition reflected in the nasal tip.4
The description of a systematic and planned approach to achieve more predictable results in nasal tip surgery is recent.5 Since then, algorithms have been proposed for the treatment of boxy nasal tips and to increase the definition in amorphous tips through more appropriate suture techniques for each type of larger alar cartilage shape, and for the patient skin type, but with little emphasis on the use of grafts, especially in patients with thick skin.6,7 Due to this fact, another algorithm was proposed to control the projection associated with nasal tip refinement in order to improve the predictability of the nasal tip surgery by using non-destructive and non-palpable techniques, which only emphasized suture techniques and some grafts, while failing to address the simplest or the even more complex techniques.8
Due to the multiplicity and complexity of the nasal tip deformities encountered by surgeons, no single technique is adequate to correct the several anatomical presentations of the nasal tip. Therefore, preoperative planning is the basis of rhinoplasty.9 Thus, to date, only one study described the gradual and systematic approach to nasal tip definition, based on preoperative anatomical assessment emphasizing surgical techniques, from the simplest to the most complex and, thus, the present study was based on this previously described protocol.10
This study aims to disclose the results of rhinoplasty, through a gradual surgical approach to nasal tip definition based on anatomical characteristics and to evaluate the degree of satisfaction of patients after the surgical procedure.
MethodsAccording to the Regulations on Human Research, Resolution 196/96 of the Ministry of Health, the study was approved by the Research Ethics Committee of the institution, protocol number 241.098/2013.
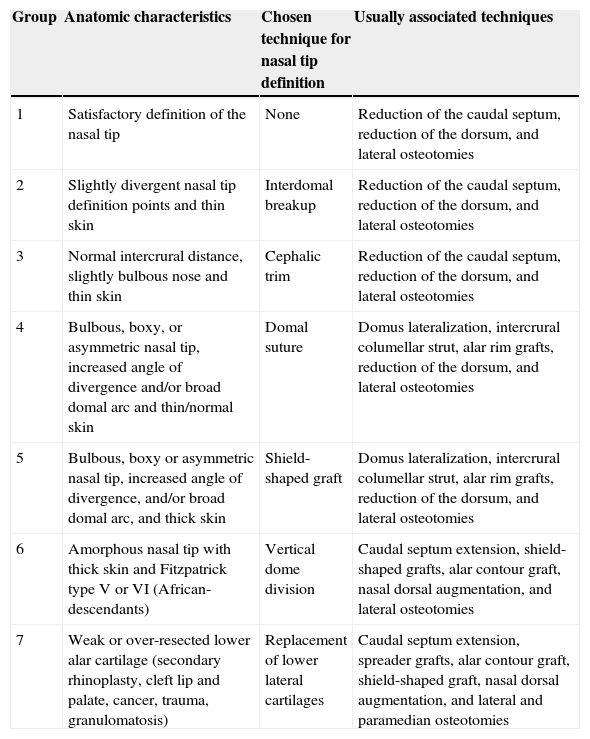
This was a longitudinal retrospective cohort study, which evaluated the medical records of 780 patients of both genders who underwent rhinoplasty in the period of January 2005 to January 2012, by the medical team of the Department of Otolaryngology and Head and Neck Surgery of the Hospital de Base de São José do Rio Preto - Faculdade de Medicina de São José do Rio Preto (FAMERP), São José do Rio Preto, SP, Brazil. A total of 533 patients who met the study criterion were selected. The following variables were analyzed: gender, age at surgery, nasal anatomical characteristics, type of surgical approach, and degree of patient satisfaction after the procedure (defined through the last note on the chart). The sole criterion for inclusion in the study was for the patient to have been submitted to rhinoplasty with or without nasal tip surgery. The exclusion criteria were less than one year of postoperative follow-up and missing data in the chart. According to the data obtained, the patients were divided into groups as shown in Table 1.10
Distribution by group of the proposed surgical techniques for nasal tip definition according to the anatomical characteristics.10
| Group | Anatomic characteristics | Chosen technique for nasal tip definition | Usually associated techniques |
|---|---|---|---|
| 1 | Satisfactory definition of the nasal tip | None | Reduction of the caudal septum, reduction of the dorsum, and lateral osteotomies |
| 2 | Slightly divergent nasal tip definition points and thin skin | Interdomal breakup | Reduction of the caudal septum, reduction of the dorsum, and lateral osteotomies |
| 3 | Normal intercrural distance, slightly bulbous nose and thin skin | Cephalic trim | Reduction of the caudal septum, reduction of the dorsum, and lateral osteotomies |
| 4 | Bulbous, boxy, or asymmetric nasal tip, increased angle of divergence and/or broad domal arc and thin/normal skin | Domal suture | Domus lateralization, intercrural columellar strut, alar rim grafts, reduction of the dorsum, and lateral osteotomies |
| 5 | Bulbous, boxy or asymmetric nasal tip, increased angle of divergence, and/or broad domal arc, and thick skin | Shield-shaped graft | Domus lateralization, intercrural columellar strut, alar rim grafts, reduction of the dorsum, and lateral osteotomies |
| 6 | Amorphous nasal tip with thick skin and Fitzpatrick type V or VI (African-descendants) | Vertical dome division | Caudal septum extension, shield-shaped grafts, alar contour graft, nasal dorsal augmentation, and lateral osteotomies |
| 7 | Weak or over-resected lower alar cartilage (secondary rhinoplasty, cleft lip and palate, cancer, trauma, granulomatosis) | Replacement of lower lateral cartilages | Caudal septum extension, spreader grafts, alar contour graft, shield-shaped graft, nasal dorsal augmentation, and lateral and paramedian osteotomies |
The results were previously submitted to descriptive statistics to determine the normal range. The two-tailed Student's t-test was used for independent samples with normal distribution and the Mann–Whitney test for non-normally distributed samples. When applicable, the chi-squared test was used for comparison between variables. The level of significance was set at 5%.
ResultsOf the total of 533 patients who underwent rhinoplasty, 158 (30%) were males and 375 (70%) were females. The age range for males at the time of surgery ranged from 12 to 62 years (mean 26.7±8.9 years) and for females the age ranged from 11 to 66 years (mean 27.2±8.2 years), which is a non-significant difference (p=0.3279).
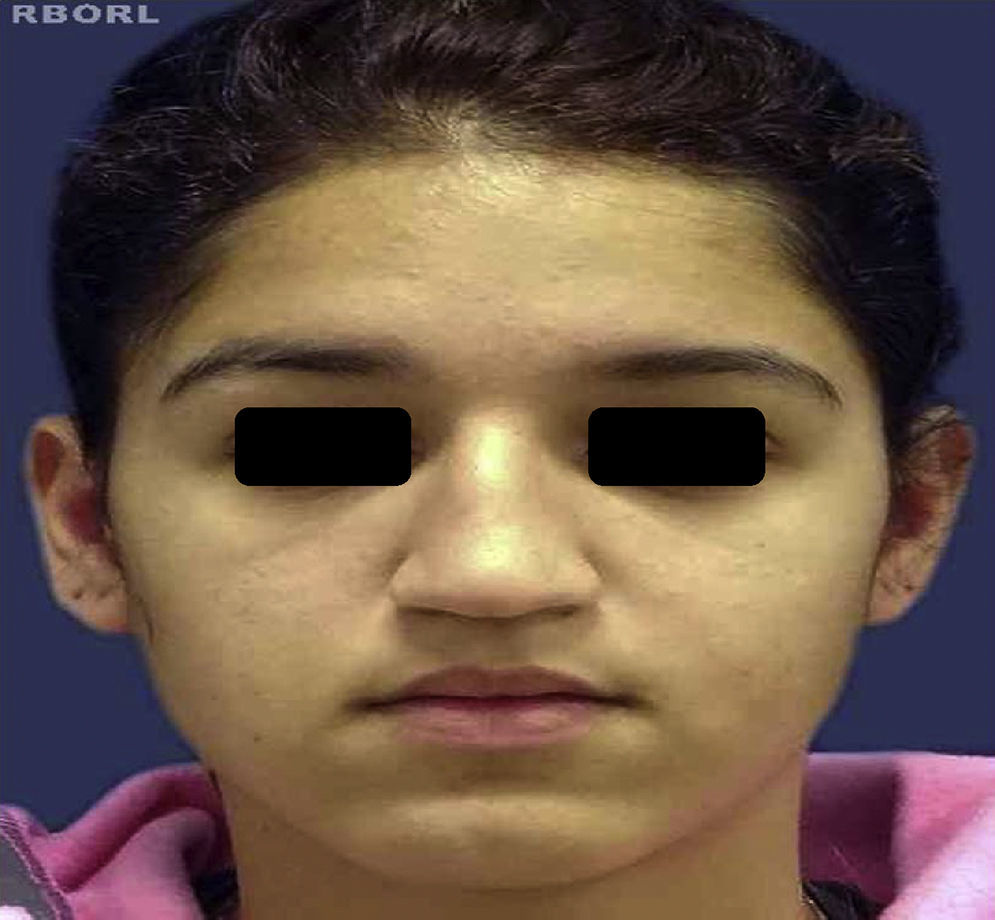
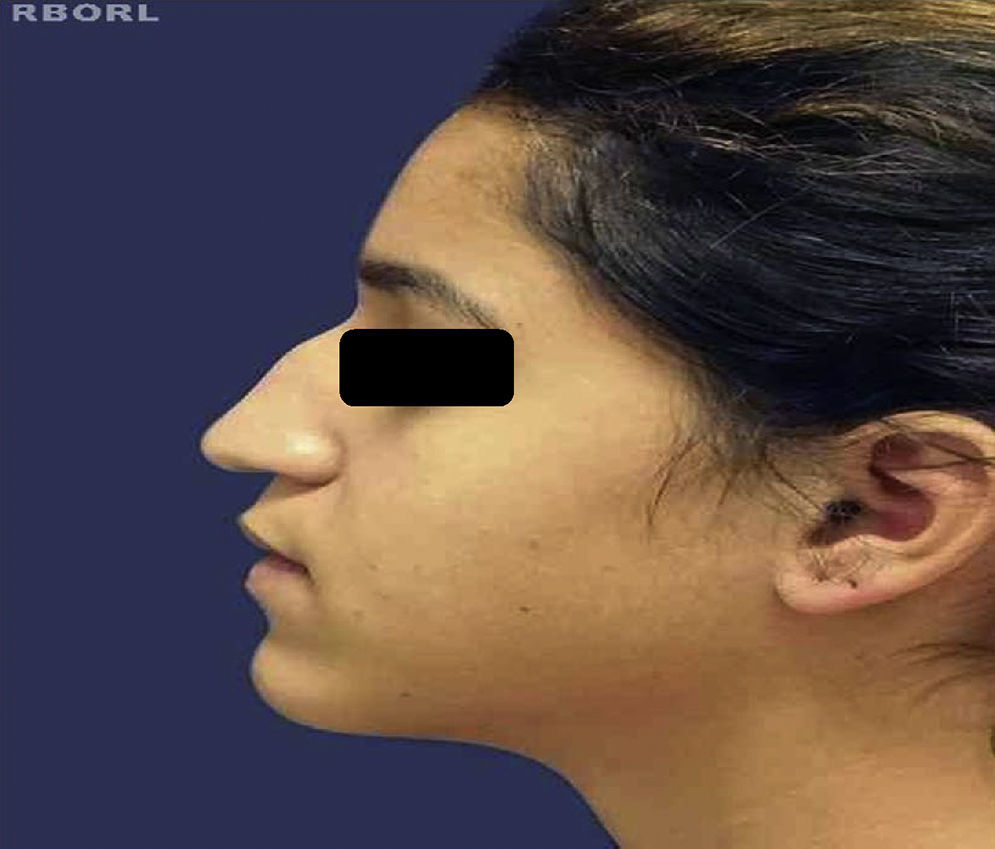
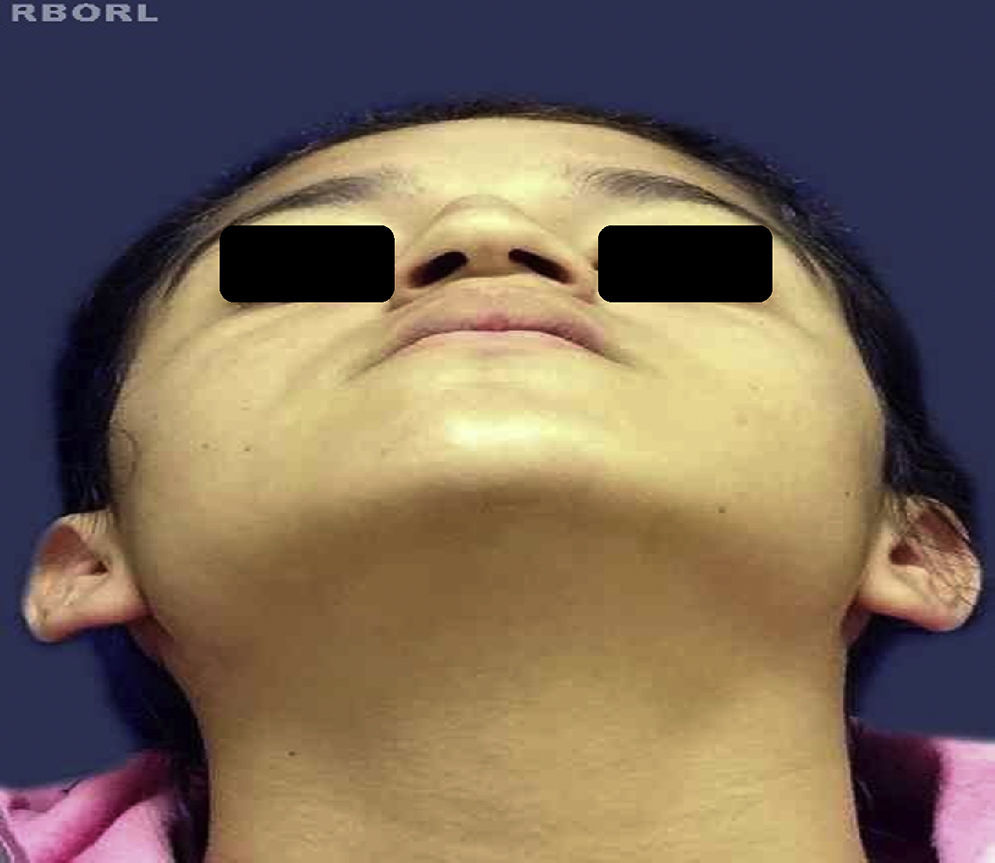
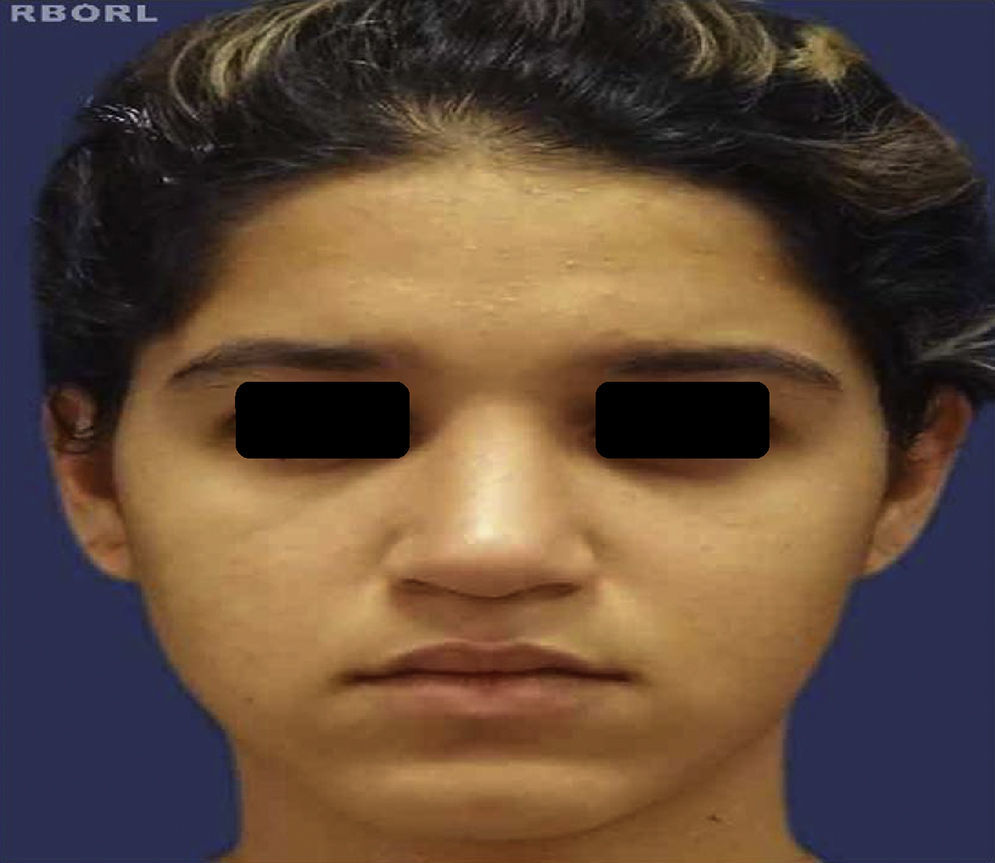
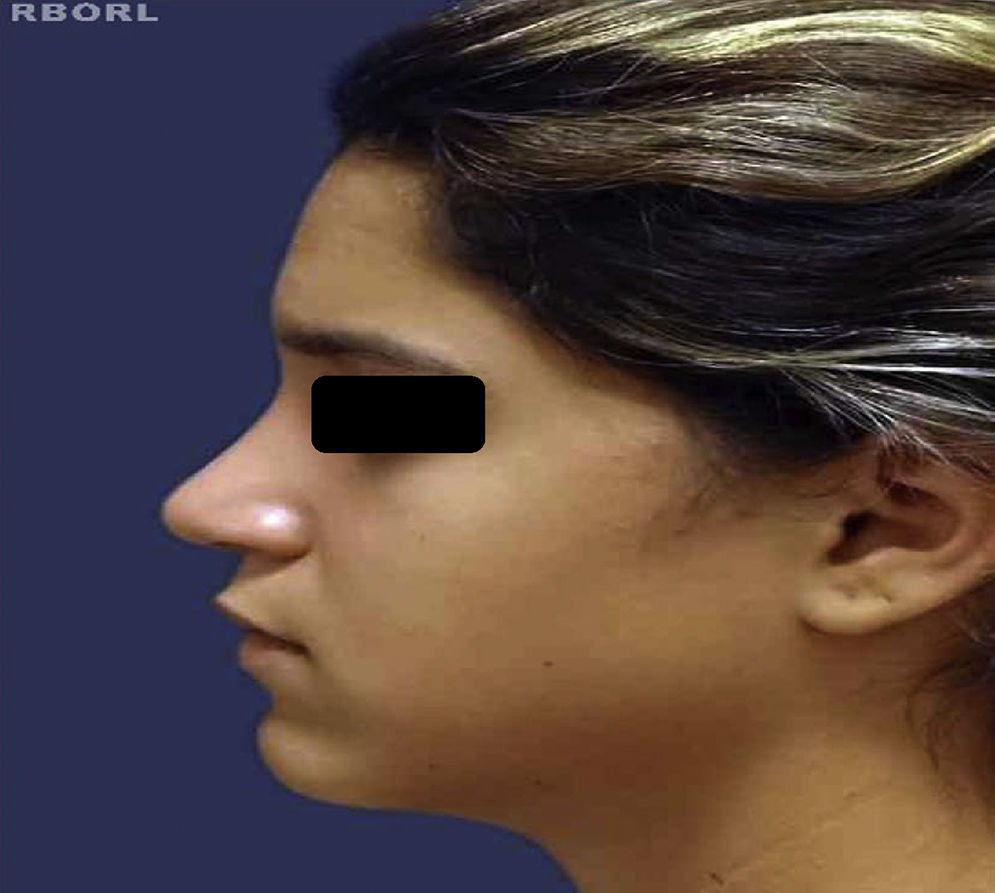
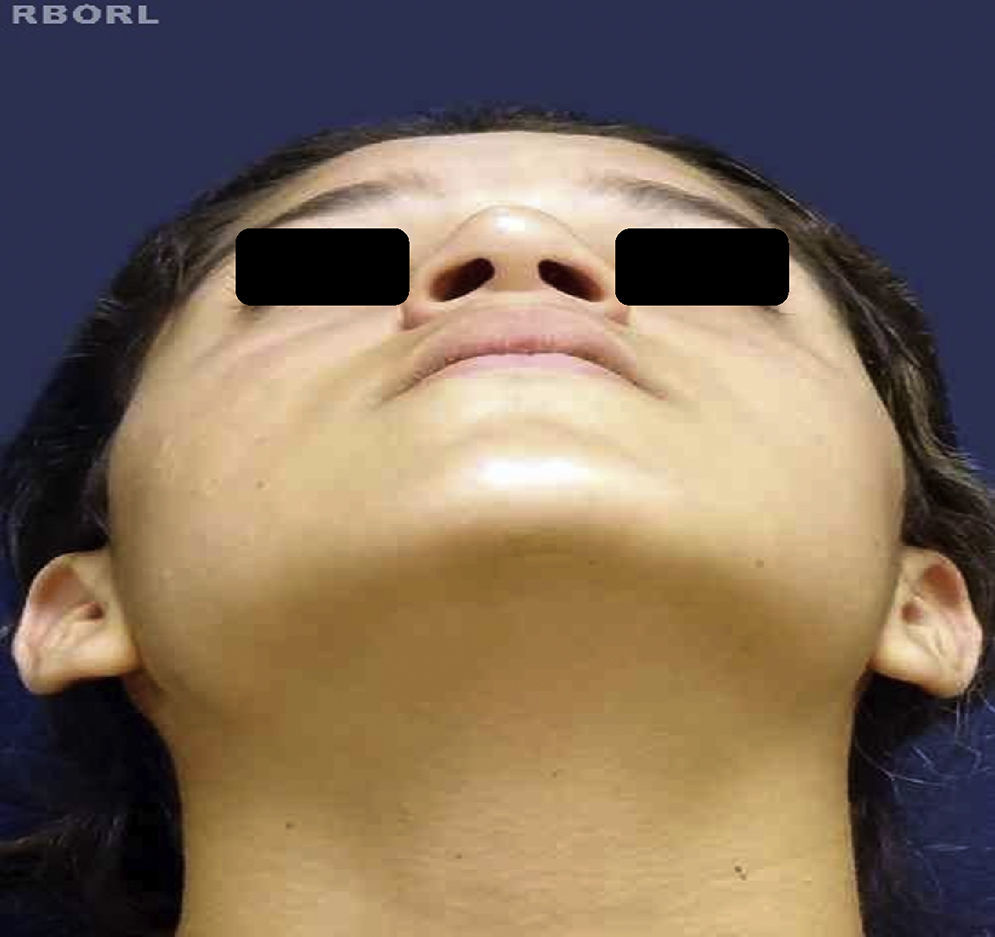
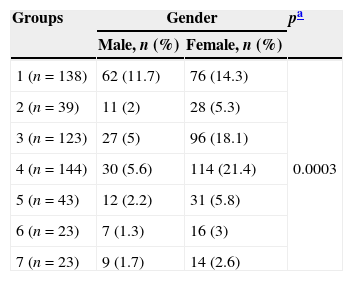
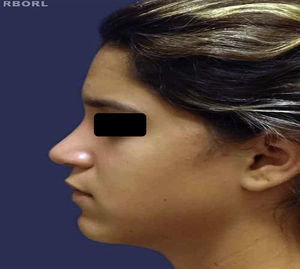
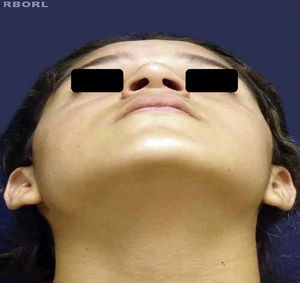
Table 2 shows the number of patients in each assigned group and according to gender. Group 4, in relation to the number of patients, showed higher prevalence (27%), followed by group 1 (26%), group 3 (23.1%), group 5 (8%), group 2 (7.3%), and groups 6 and 7, which had the same prevalence (4.3%). All groups had a higher prevalence of females, which was statistically significant (p=0.0003). Figs. 1–6 show the preoperative and postoperative appearance of a patient belonging to group 4 (highest prevalence), aged 17 year old, female, normal skin thickness, nasal tip angle with intercrural divergence and increased domal arch, symmetrical nostrils, sub-rotation, and convexity of the nasal bridge. Rhinoseptoplasty was performed through marginal and intercartilaginous incisions, followed by cephalic resection of lateral branches; transdomal, interdomal and septo-columellar sutures with interposition of columellar strut; dorsum reduction; and lateral osteotomies. After 12 months, there was improvement in tip definition.
Patient distribution n (%) in each group in relation to gender.
| Groups | Gender | pa | |
|---|---|---|---|
| Male, n (%) | Female, n (%) | ||
| 1 (n=138) | 62 (11.7) | 76 (14.3) | 0.0003 |
| 2 (n=39) | 11 (2) | 28 (5.3) | |
| 3 (n=123) | 27 (5) | 96 (18.1) | |
| 4 (n=144) | 30 (5.6) | 114 (21.4) | |
| 5 (n=43) | 12 (2.2) | 31 (5.8) | |
| 6 (n=23) | 7 (1.3) | 16 (3) | |
| 7 (n=23) | 9 (1.7) | 14 (2.6) | |
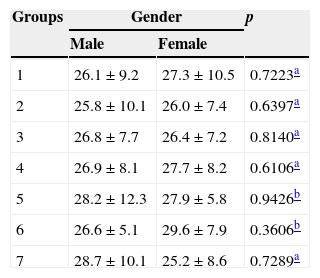
The analysis of mean age between the genders of the patients from each analyzed group allowed for identification of approximately similar mean values revealing no statistical difference (Table 3).
Distribution, in mean values±standard deviation, of the age range in each group analyzed in relation to gender.
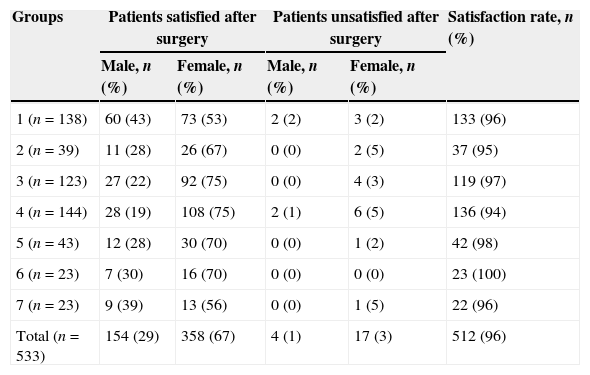
The number of patients was assessed according to gender in each surgical group in relation to satisfaction with the rhinoplasty result 12–30 months after the procedure, showing an overall rate of 96% of satisfied patients, with a predominance of females (67%). Twenty-one patients (4%), also with a prevalence of females (3%) expressed dissatisfaction with the outcome of the procedure. Regarding the groups, Group 6 showed 100% satisfaction, followed by Groups 5 (98%), group 3 (97%), groups 1 and 7 (both 96%), and group 2 (95%). Group 4 had the lowest rate of satisfaction (94%; Table 4).
Distribution of patients according to gender, in each group, in relation to the satisfaction with the surgical procedure outcome.
| Groups | Patients satisfied after surgery | Patients unsatisfied after surgery | Satisfaction rate, n (%) | ||
|---|---|---|---|---|---|
| Male, n (%) | Female, n (%) | Male, n (%) | Female, n (%) | ||
| 1 (n=138) | 60 (43) | 73 (53) | 2 (2) | 3 (2) | 133 (96) |
| 2 (n=39) | 11 (28) | 26 (67) | 0 (0) | 2 (5) | 37 (95) |
| 3 (n=123) | 27 (22) | 92 (75) | 0 (0) | 4 (3) | 119 (97) |
| 4 (n=144) | 28 (19) | 108 (75) | 2 (1) | 6 (5) | 136 (94) |
| 5 (n=43) | 12 (28) | 30 (70) | 0 (0) | 1 (2) | 42 (98) |
| 6 (n=23) | 7 (30) | 16 (70) | 0 (0) | 0 (0) | 23 (100) |
| 7 (n=23) | 9 (39) | 13 (56) | 0 (0) | 1 (5) | 22 (96) |
| Total (n=533) | 154 (29) | 358 (67) | 4 (1) | 17 (3) | 512 (96) |
The nasal tip can be assessed by its definition, projection (distance from tip of nose to the most posterior point of the naso-facial junction), and rotation (cephalic or caudal movement of the nasal tip in relation to the head plane).2,3 To achieve a better definition of the nasal tip, every surgeon should work with the concepts of conservation of the skeleton, cartilage repositioning, and highly precise surgical technique. Due to anatomical variations, especially in the major alar cartilages and the envelope of skin and subcutaneous tissue, a protocol was created describing several techniques for nasal tip definition.10 With a systematic approach to preoperative planning,10 it is possible to achieve satisfactory postoperative results, thus making rhinoplasty less intimidating, despite its reputation as one of the most challenging procedures in facial plastic surgery.3,5,9
Thus, the present study used a protocol published in the literature,10 for the gradual approach to nasal tip definition, based on anatomical features, which allow the surgeon to correct simpler deformities in thin-skinned patients, using conservative techniques, reserving the more complex techniques for larger tip deformities in patients with thick skin.
Of the patients in the study (533), there was a higher prevalence of females (70%), which was similar to that described in the literature (67.8%), although it analyzed a larger sample (641 patients).10 When patients were distributed in the seven study groups, there was a predominance of females in all groups. The reference study10 showed no gender distribution data between the groups for comparison with the present study.
Regarding the number of patients in each group, there was a difference in prevalence when compared to the baseline study,10 probably due to different regional and ethnic characteristics between both locations where the studies were performed. In the present study and in the reference study,10 Group 4 showed a larger number of patients.
When the rate of patient satisfaction was assessed in relation to surgical outcome in each protocol group, differences were observed in prevalence between this study and the reference.10 These differences may be due, as mentioned above, to regional and ethnic characteristics.
Despite the difficulties inherent to surgical procedures in groups 5, 6, and 7, the present study found a higher rate of satisfaction in them, when compared to the reference study.10
In spite of differences in the sample and the physical characteristics of patients, the assessment of overall satisfaction rate of this study (96%) was similar to that of the reference study (95.6%).10 However, the rate of revision of the present study was lower (4%) than that of the reference study (5.6%),10 although both are considered low for rhinoplasty.
Therefore, in general, the rates of patient satisfaction and revision obtained in the present study were considered adequate for nasal tip definition, according to the approach protocol used.10 This gradual approach can be considered the initial step in the preoperative planning of rhinoplasty. After defining to which group each patient belongs, other maneuvers should be selected to correct other deformities, progressing from simple repairs to the complex, based on the anatomical diagnosis.
ConclusionsThe protocol allowed the use of a progressive step-by-step surgical approach for nasal tip definition depending on the anatomical nasal characteristics, produced a high rate of satisfaction with the surgical outcome, and a low rate of revision.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: de Carvalho TB, Thomazi E, Leutz RP, Souza RP, Molina FD, Piatto VB, et al. Gradual approach to refinement of the nasal tip: surgical results. Braz J Otorhinolaryngol. 2015;81:31–6.