The success of pharyngeal surgery in the treatment of obstructive sleep apnea syndrome depends on the appropriate selection of patients.
ObjectiveTo propose a new staging for indication of pharyngeal surgery in obstructive sleep apnea syndrome.
MethodsA total of 54 patients undergoing extended tonsillectomy were retrospectively included, divided into six stages. Stage I: patients with palatine tonsils grade 3/4 and modified Mallampati index 1/2; stage II: palatine tonsils 3/4 and modified Mallampati index 3/4; stage III: palatine tonsils 1/2 and modified Mallampati index 1/2; stage IV: palatine tonsils 1/2 and modified Mallampati index 3/4; stage V: body mass index ≥40kg/m2 with palatine tonsils 3/4 and modified Mallampati index 1, 2, 3, or 4. Stage VI: body mass index ≥40 with palatine tonsils 1/2 and modified Mallampati index 1, 2, 3, or 4.
ResultsThe surgical success rates were 88.9%, 75.0%, 35.7%, 38.5%, and 100.0% in stages I–V.
ConclusionThe presence of hypertrophic palatine tonsils was the anatomical factor in common in the most successful stages (I, II, and V), regardless of body mass index. Although the modified Mallampati index classes 3 and 4 reduced the success rate of surgery in patients with hypertrophic tonsils (stage II), the presence of modified Mallampati index classes 1 and 2 did not favor surgical success in patients with normal tonsils (stage III).
O sucesso da cirurgia faríngea no tratamento da síndrome da apnéia obstrutiva do sono (SAOS) depende da adequada seleção de pacientes.
ObjetivoPropor um novo estadiamento para indicação de cirurgia faríngea na SAOS.
MétodoEstudo retrospectivo, onde foram inclusos, 54 pacientes submetidos a amigdalectomia ampliada, divididos em 6 estádios. Estádio I: pacientes com tonsilas palatinas graus 3/4 e índice de Mallampati modificado (IMM) 1/2; Estádio II: tonsilas palatinas 3/4 e IMM 3/4; Estádio III: tonsilas palatinas 1/2 e IMM 1/2; Estádio IV: tonsilas palatinas 1/2 e IMM 3/4; Estádio V: IMC (índice de massa corpórea) ≥ com tonsilas palatinas 3/4 e IMM 1,2,3 ou 4. Estádio VI: IMC ≥ kg/m2 com tonsilas palatinas 1ou2 e IMM 1, 2, 3, ou 4.
ResultadosAs taxas de sucesso cirúrgico foram de 88,9%; 75,0%; 35,7%; 38,5% e 100,0% nos estádios I a V.
ConclusãoA presença de tonsilas palatinas hipertróficas foi o fator anatômico em comum nos estádios de maior sucesso (I, II e V), independente do IMC. Apesar do IMM classe III e IV diminuir a taxa de sucesso da cirurgia em pacientes com tonsilas hipertróficas (estádio II), a presença de IMM classe I e II não favoreceu o sucesso cirúrgico em pacientes com tonsilas normotróficas (estádio III).
Obstructive sleep apnea syndrome (OSAS) is a highly prevalent disease that affects 32.9% of the adult population of the city of São Paulo, Brazil1 and compromises the quality of life of patients as a result of excessive daytime sleepiness, cognitive function impairment and increased risk for cardiovascular disease.2,3 Ventilation with positive airway pressure, especially continuous positive airway pressure (CPAP) is the treatment of choice for patients with moderate to severe OSAS4; however, many patients have difficulty adapting to this long-term treatment.3,5–7
Uvulopalatopharyngoplasty was the most often performed pharyngeal surgical procedure to treat OSAS; however, the success rate, when the surgery is indiscriminately indicated, was approximately 40%.6 Several factors were considered unfavorable, such as disease severity, age, the presence of multiple sites of obstruction, obesity, and anatomical abnormalities of the maxilla and mandible.8
Several pharyngeal surgery techniques are described in the literature, and according to a meta-analysis,9 the isolated uvulopalatopharyngoplasty procedure, with or without tonsillectomy, interferes with the apnea–hypopnea index (AHI), but maintains residual OSAS,9,10 mainly in patients with moderate to severe OSAS.
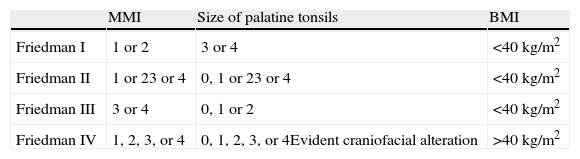
In an attempt to improve the selection criteria for uvulopalatopharyngoplasty, Friedman et al.11 proposed a clinical staging based on anthropometric and otorhinolaryngological physical examination for patients with OSAS, that is used till date. This staging is based on three clinical criteria: modified Mallampati index (MMI), palatine tonsil size, and body mass index (BMI). MMI classes 3 and 4 show an unfavorable relationship among the soft palate, the tongue, and the oropharynx; palatine tonsils grade 3 and 4 are considered hypertrophic.
Thus, he divided patients into four groups. Group I: patients with MMI 1 or 2 associated with palatine tonsil grade 3 or 4 and BMI<40kg/m2; group II: patients with MMI 3 or 4 associated with palatine tonsil grade 3 or 4 or MMI 1 or 2 with palatine tonsils grade 1 or 2 and BMI<40kg/m2; group III: patients with MMI 3 or 4 associated with palatine tonsil 1 or 2 with BMI<40kg/m2; and group IV: patients with BMI>40kg/m2 or significant skull-facial alteration, regardless of the MMI and tonsil size.
Utilizing his staging, Friedman et al.12 published a series of 134 patients who underwent pharyngeal surgery; the surgical success for groups I, II, and III was 80.6%, 37.9%, and 8.1%, respectively. The authors felt that the procedure was contraindicated in group IV, stating that the presence of MMI classes 3 and 4 could prevent a favorable surgical outcome, even in patients with hypertrophic palatine tonsils, and that the presence of evident skull-facial alterations and obesity class III would be factors to render the procedure contraindicated.
However, Martinho et al.,13 in a series of cases with seven obese patients with OSAS, MMI classes 3 and 4, and hypertrophy of the palatine tonsils grades 3 and 4, observed a significant reduction in the AHI (preoperative: 81±26/h; postoperative: 23±18/h; p<0.05) and minimum oxyhemoglobin saturation improvement (preoperative: 69±14%; postoperative: 83±3%; p<0.05), after extended tonsillectomy. Despite the small number of patients, this study suggested that tonsillar hypertrophy may be the main factor associated with pharyngeal surgery success, regardless of the MMI or the presence of obesity.
Therefore, it is evident that the clinical and anatomical assessment of patients with OSAS is crucial in choosing the best treatment modality. However, to date, there is no ideal staging model for the indication of pharyngeal surgery in the treatment of OSAS, especially for patients with BMI>40kg/m2 or with significant skull-facial alteration, regardless of the MMI and size of palatine tonsils.
Therefore, this study aimed to develop a new staging model for the indication of pharyngeal surgery in adult patients with OSAS, as well as to describe the use of the extended tonsillectomy technique to treat these patients.
MethodsThe research project was approved by the ethics committee (CEP: 0268/11).
A retrospective study was conducted by reviewing the medical charts of patients treated from January of 2003 to December of 2007 in a Respiratory Sleep Disorder Outpatient Clinic of the Department of Otorhinolaryngology and Head and Neck Surgery.
Inclusion criteria were patients aged between 18 and 65 years, of both genders, with moderate to severe OSAS, submitted to extended tonsillectomy with pre- and postoperative polysomnography assessment.
Patients referred for other clinical or surgical treatments of OSAS other than extended tonsillectomy; those with other types of sleep disorder than OSAS; those who used sedatives, consumed alcohol, or had a clinically decompensated disease were excluded from the study.
Assessment protocolIn this outpatient clinic, patients are routinely submitted to the assessment protocol, that consists of otorhinolaryngological evaluation, visual analog scale (VAS), Epworth sleepiness scale,14 and baseline polysomnography, which is repeated three months after the surgical procedure.
On the VAS, patients were asked about the presence of snoring and witnessed pauses, which were considered “usual” when they occurred every night or almost every night. The Epworth sleepiness scale14 suggests excessive daytime sleepiness when the scores are >9. These criteria were used in combination with the polysomnography findings for the diagnosis of OSAS, according to the II International Classification of Sleep Disorders (ICSD-2)15 and the American Academy of Sleep Medicine (AASM) 2005 criteria.16
Otorhinolaryngological assessmentThe otorhinolaryngological assessment consisted of the facial skeleton inspection through oroscopy and anterior rhinoscopy. For the purpose of the study, we describe only the criteria to be used in the proposed staging method. They are the palatine tonsil classification (PTC), the MMI, and the BMI, calculated using the formula: weight (kg)/height2 (m2).
The MMI was performed as suggested by Friedman et al.,17 with the patient in the sitting position, with maximum mouth opening and relaxed tongue positioned within the oral cavity. Patients were classified into four grades: grade 1 (the entire oropharynx is well visualized, including the soft palate, the tonsillar pillars, the palatine tonsils, and the uvula); grade 2 (the upper pole of the palatine tonsils and the uvula are visualized); grade 3 (part of the soft palate and the uvula insertion is visualized); and grade 4 (only the hard palate is visualized).
As proposed by Friedman et al.17 and Zonato et al.,18 the palatine tonsils were classified as grade 1 (occupying up to 25% of the oropharynx), grade 2 (50% of the oropharynx), grade 3 (75% of the oropharynx), and grade 4 (> 75% of oropharynx). Grades 3 and 4 were considered as cases of obstructive hypertrophy of the palatine tonsils.
Basal polysomnographyPolysomnography was performed in an EMBLA computerized system (EMBLA® S7000; EMBLA Systems, Inc. – Broomfield, CO, United States). An overnight recording was performed in a dark, quiet room, specially designed for this procedure, while monitoring was performed through electroencephalogram, electrooculogram, submental and tibial electromyogram, electrocardiogram, airflow by nasal cannula connected to a pressure transducer and an oral thermistor, respiratory movements by inductance plethysmography with thoracoabdominal belts, oxyhemoglobin saturation (SpO2) by pulse oximetry, and snoring sounds were recorded by a microphone and body position sensor.
The staging of sleep followed the criteria proposed by Rechtschaffen and Kales,19 and awakenings followed the 1992 criteria of the American Sleep Disorders Association (ASDA).20 The staging of respiratory events followed the 1999 criteria of the AASM.16
The diagnosis of OSAS followed the 2005 clinical and polysomnographic criteria of the ICSD-2.15 A mild increase in AHI was considered when patients had index values between 5 and 15 events per hour of sleep; moderate increase, between 15 and 30; and marked increase, >30.
The baseline polysomnography was repeated three months after pharyngeal surgery. The surgery was considered a partial success when there was a 50% reduction in AHI and an AHI<20/h, according to the criteria used by Friedman et al.21
Surgical technique–extended tonsillectomyThe surgical technique used in patients with hypertrophic tonsils is conservative, as the main objective is the lateral amplification of the pharynx, while preserving and repositioning the pillars, addressing mainly the lateral oropharyngeal wall, sparing the soft palate and the uvula region (midline). Therefore, this technique is called extended tonsillectomy.
Initially, a bilateral tonsillectomy is performed, with an elliptical peritonsillar incision in the mucosa overlying the palatopharyngeal and palatoglossus muscles after medial traction of the mucosa, aiming at its maximum preservation in this region. This is followed by tonsil removal through dissection along the tonsil capsule, while preserving the underlying musculature and subsequent hemostasis using bipolar cautery and simple stitches with vicryl rapid 3.0® suture thread. The muscle layer of the tonsillar region is closed with single stitches in the craniocaudal direction, using vicryl rapid 3.0® suture thread. After closing the muscle layer, the palate “web” (membrane formed by the low insertion of the posterior pillar of the uvula) is removed, when present, using electric scalpel or scissors, and this is the upper limit of the midline resection. Then, the mucosa is closed with vicryl rapid 3.0® suture thread, using simple stitches, in the craniocaudal direction. If the uvula is considered long, a partial uvulectomy is performed, corresponding to the distal third of the uvula. The aim of this technique is the lateral enlargement of the pharynx and anteriorization of the soft palate.
The procedure is performed under general anesthesia without pre-anesthetic sedative medication, as recommended in patients with OSAS. Patients remain in the hospital for 24hours and receive antibiotics (amoxicillin at a dose of 50mg/kg/day for seven days) and non-opioid analgesics (paracetamol and dipyrone) at discharge. The follow-up consultations are performed after one, three, 12, 18, and 24 weeks.
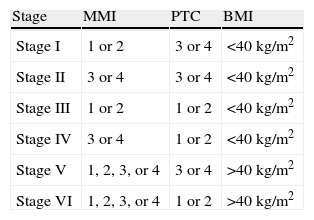
New proposed stagingIn our proposed staging (Table 1), we decided to divide stage II of Friedman et al.17 (Table 2) into two separate sub-groups and to add a group for patients with class III obesity (BMI>40kg/m2) with palatine tonsils grade 3 and 4 associated with any class of MMI, as a new stage V. We did not perform surgery for patients with obesity class III and tonsils grade 1 and 2, regardless of MMI.
New clinical staging for pharyngeal surgery indication in patients with obstructive sleep apnea.
| Stage | MMI | PTC | BMI |
| Stage I | 1 or 2 | 3 or 4 | <40kg/m2 |
| Stage II | 3 or 4 | 3 or 4 | <40kg/m2 |
| Stage III | 1 or 2 | 1 or 2 | <40kg/m2 |
| Stage IV | 3 or 4 | 1 or 2 | <40kg/m2 |
| Stage V | 1, 2, 3, or 4 | 3 or 4 | >40kg/m2 |
| Stage VI | 1, 2, 3, or 4 | 1 or 2 | >40kg/m2 |
MMI, modified Mallampati index; PTC, palatine tonsil classification; BMI, body mass index.
Friedman's staging for indication of uvulopalatopharyngoplasty in patients with obstructive sleep apnea syndrome.17
| MMI | Size of palatine tonsils | BMI | |
| Friedman I | 1 or 2 | 3 or 4 | <40kg/m2 |
| Friedman II | 1 or 23 or 4 | 0, 1 or 23 or 4 | <40kg/m2 |
| Friedman III | 3 or 4 | 0, 1 or 2 | <40kg/m2 |
| Friedman IV | 1, 2, 3, or 4 | 0, 1, 2, 3, or 4Evident craniofacial alteration | >40kg/m2 |
MMI, modified Mallampati index; BMI, body mass index.
Thus, the patients were divided into six groups: stage I, patients with grade 3 or 4 palatine tonsils and MMI class 1 or 2; stage II, patients with grade 3 or 4 palatine tonsils and MMI class 3 or 4; stage III, patients submitted to tonsillectomy (0) grade 1 or 2 palatine tonsils and MMI class 1 or 2; stage IV, patients submitted to tonsillectomy (0), grade 1 or 2 palatine tonsils, and MMI class 3 or 4; stage V, patients with BMI>40kg/m2 with grade 3 or 4 palatine tonsils and MMI class 1, 2, 3, or 4; and stage VI, patients with BMI>40kg/m2 with grade 1 or 2 palatine tonsils and MMI class 1, 2, 3, or 4. This latter group comprised the patients not referred for surgery due to high morbidity.
Within each stage, patients were also divided according to AHI, as follows: group I, patients with mild OSAS (between 5 and 15 events per hour of sleep and associated clinical complaints); group II, patients with moderate OSAS (between 15 and 30); and group III, patients with severe OSAS (>30).
ResultsOf the 622 reviewed medical records of patient treated during the study period, 129 patients received indication for extended tonsillectomy; 54 patients met the inclusion criteria and were thus included in the study.
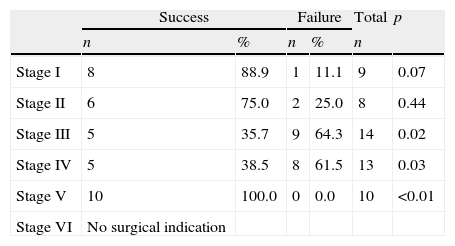
Of the 54 patients, 35 (64.8%) were males and 19 (35.1%) were females, aged 18–61 years, with a mean age of 38.9±7.5 years. After staging, the patients were divided as follows: stage I: nine patients (16.6%); stage II: eight patients (14.8%); stage III: 14 patients (25.9%); stage IV: 13 patients (24%); and stage V: 10 patients (18.5%). Surgical success rates were 88.9%, 75.0%, 35.7%, 38.5% and 100.0%, respectively.
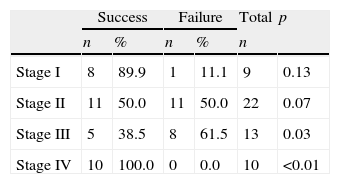
Data for each group and the success and failure rates are shown in Table 3. There was a statistically significant difference in stages III, IV, and V (p=0.02, p=0.03, and p<0.01, respectively). Stages III and IV presented the highest failure rates (p=0.02 and p=0.03, respectively), and the highest success rates were observed in stage V (p<0.01).
Comparison of success and failure rates according to the new staging for patients undergoing extended tonsillectomy for the treatment of obstructive sleep apnea syndrome (OSAS).
| Success | Failure | Total | p | |||
| n | % | n | % | n | ||
| Stage I | 8 | 88.9 | 1 | 11.1 | 9 | 0.07 |
| Stage II | 6 | 75.0 | 2 | 25.0 | 8 | 0.44 |
| Stage III | 5 | 35.7 | 9 | 64.3 | 14 | 0.02 |
| Stage IV | 5 | 38.5 | 8 | 61.5 | 13 | 0.03 |
| Stage V | 10 | 100.0 | 0 | 0.0 | 10 | <0.01 |
| Stage VI | No surgical indication | |||||
Significance value: p<0.05, chi-square test.
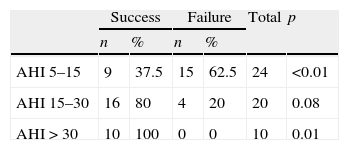
Regarding the AHI, 24 patients (44.4%) had mild increase in AHI; 20 patients (37.0%) had a moderate increase, and ten patients (18.6%) achieved a marked increase (Table 4). The failure rate was significantly higher in the group with mild increase in AHI (p<0.01), and the highest success rate was found in the group with a marked increase in AHI (p=0.01).
Comparison of success and failure rates according to the increase of apnea–hypopnea index.
| Success | Failure | Total | p | |||
| n | % | n | % | |||
| AHI 5–15 | 9 | 37.5 | 15 | 62.5 | 24 | <0.01 |
| AHI 15–30 | 16 | 80 | 4 | 20 | 20 | 0.08 |
| AHI>30 | 10 | 100 | 0 | 0 | 10 | 0.01 |
AHI, apnea–hypopnea index per hour of sleep.
Significance value: p<0.05, chi-squared test.
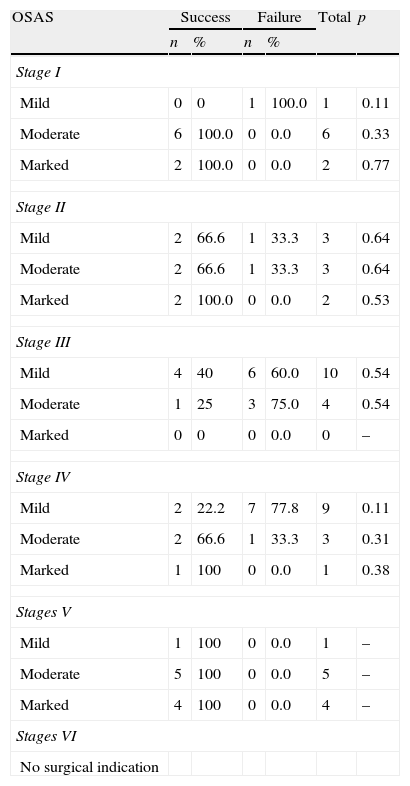
Within each proposed stage, the patients were divided according to AHI increase, and there were no statistically significant differences (Table 5).
Comparison of success and failure rates according to the new staging and apnea–hypopnea index for patients undergoing extended tonsillectomy for the treatment of obstructive sleep apnea syndrome (OSAS).
| OSAS | Success | Failure | Total | p | ||
| n | % | n | % | |||
| Stage I | ||||||
| Mild | 0 | 0 | 1 | 100.0 | 1 | 0.11 |
| Moderate | 6 | 100.0 | 0 | 0.0 | 6 | 0.33 |
| Marked | 2 | 100.0 | 0 | 0.0 | 2 | 0.77 |
| Stage II | ||||||
| Mild | 2 | 66.6 | 1 | 33.3 | 3 | 0.64 |
| Moderate | 2 | 66.6 | 1 | 33.3 | 3 | 0.64 |
| Marked | 2 | 100.0 | 0 | 0.0 | 2 | 0.53 |
| Stage III | ||||||
| Mild | 4 | 40 | 6 | 60.0 | 10 | 0.54 |
| Moderate | 1 | 25 | 3 | 75.0 | 4 | 0.54 |
| Marked | 0 | 0 | 0 | 0.0 | 0 | – |
| Stage IV | ||||||
| Mild | 2 | 22.2 | 7 | 77.8 | 9 | 0.11 |
| Moderate | 2 | 66.6 | 1 | 33.3 | 3 | 0.31 |
| Marked | 1 | 100 | 0 | 0.0 | 1 | 0.38 |
| Stages V | ||||||
| Mild | 1 | 100 | 0 | 0.0 | 1 | – |
| Moderate | 5 | 100 | 0 | 0.0 | 5 | – |
| Marked | 4 | 100 | 0 | 0.0 | 4 | – |
| Stages VI | ||||||
| No surgical indication | ||||||
When we staged the patients according to the criteria by Friedman et al.,21 the following results were obtained: in Friedman group I, nine patients were included with a surgical success rate of 89%; in Friedman group II, 22 patients were included with 50% surgical success; in Friedman in group III, 13 patients were included with surgical success rate of 38%; lastly, Friedman group IV included ten patients with surgical success rate of 100% (Table 6). Statistically significant differences were observed in Friedman stages III and IV, with the highest failure rate in Friedman group III (p=0.03) and the highest success in Friedman group IV (p<0.01).
DiscussionOur proposed staging demonstrated that the extended tonsillectomy surgery for the treatment of OSAS has the highest success rates in patients with hypertrophic tonsils (stages I, II, and V) and that MMI classes 3 and 4 (stage II) decreased the success rate in these patients. Nonetheless, the success rate was higher than in those patients with normal-sized tonsils (stages III and IV), even in patients with favorable MMI (stage III) and those with class III obesity (stage V). Thus, our division of Friedman et al.’s17 stage II and the inclusion of patients who have class III obesity associated with hypertrophic tonsils can improve the indication criteria for pharyngeal surgery in the treatment of OSAS.
CPAP is considered the gold standard for treating moderate to severe OSAS, but has the disadvantage that many patients have difficulties in adapting to it, especially in the long term, making surgical treatment a therapeutic option.22
When performed in a systematic way, the success rate of uvulopalatopharyngoplasty is 40.7%,6 but if patients are selected according to the presence of anatomical changes in the oropharynx, such as tonsillar hypertrophy, medianized pillars, redundant palate, and elongated uvula, the success rate is higher.11,12,21
Some studies in the literature have demonstrated higher success rates when the surgery was performed on patients with mild to moderate OSAS.23,24 In the present study, patients with marked increase in AHI were those who benefited the most from the surgical treatment, probably due to the criterion selected for success. In patients with mild increase in AHI, a reduction <50% was considered as failure, when it is known that, for these patients, the control of clinical symptoms is a more important outcome than AHI, since presence of OSAS is only considered in patients with AHI<15 per hour when associated with a clinical complaint.
Another fact that leads to believe that OSAS severity is not a determinant factor for the indication of pharyngeal surgeries for the treatment of OSAS is that, when the degree of AHI increase is compared among the stages, no significant differences were found in relation to success. Similar findings were described by Friedman et al.,12 who also found no association between OSAS severity and pharyngeal surgery success.
In 2002, Friedman et al.11 proposed a staging system based on upper airway alterations (size of palatine tonsils and MMI) and BMI, and reported a surgical success rate of 80.6% in patients with BMI<40kg/m2, with hypertrophic tonsils (grades 3 and 4) and favorable MMI (1 and 2), regardless of OSAS severity; the success rate decreased significantly as these parameters varied in the other stages.
Since Martin et al.13 found significant improvement in polysomnographic respiratory parameters in a case series of obese patients with MMI classes 3 and 4 and hypertrophic palatine tonsils (patients with Friedman's stages II and IV), we considered that a refinement of Friedman's17 staging system might improve the indication of pharyngeal surgeries, as this staging mixed patients with normal-sized and hypertrophic tonsils in stage II and contraindicated surgery in patients with class III obesity, even in the presence of hypertrophic tonsils (stage IV).
Confirming the findings of Martin et al.13 and Friedman et al.,21 our study demonstrated that patients who had hypertrophic palatine tonsils achieved higher success rates with the procedure, independent of AHI13,21 or class III obesity,13 and that the presence of MMI 3 and 4 decreased the success rate in such patients. However, the presence of MMI 1 and 2 in patients with normotrophic tonsils did not correlate with surgical success. Thus, we conclude that an unfavorable MMI decreases the chances of success, but a favorable MMI does not improve the chances of surgical success unless the patients also had hypertrophic tonsils.
ConclusionsDespite the limitations of this study, mainly its retrospective nature and a small sample size, we conclude that our proposed new staging method can improve the surgical indications and results of extended tonsillectomy in the treatment of patients with OSAS.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Vidigal TA, Haddad FL, Cabral RF, Oliveira MC, Cavalcante RR, Bittencourt LR, et al. New clinical staging for pharyngeal surgery in obstructive sleep apnea patients. Braz J Otorhinolaryngol. 2014;80:490–6.
Institution: Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil.