Psychogenic dysphonia is a functional disorder with variable clinical manifestations.
ObjectiveTo assess the clinical and vocal characteristics of patients with psychogenic dysphonia in a case series.
MethodsThe study included 28 adult patients with psychogenic dysphonia, evaluated at a University hospital in the last ten years. Assessed variables included gender, age, occupation, vocal symptoms, vocal characteristics, and videolaryngostroboscopic findings.
Results28 patients (26 women and 2 men) were assessed. Their occupations included: housekeeper (n=17), teacher (n=4), salesclerk (n=4), nurse (n=1), retired (n=1), and psychologist (n=1). Sudden symptom onset was reported by 16 patients and progressive symptom onset was reported by 12; intermittent evolution was reported by 15; symptom duration longer than three months was reported by 21 patients. Videolaryngostroboscopy showed only functional disorders; no patient had structural lesions or changes in vocal fold mobility. Conversion aphonia, skeletal muscle tension, and intermittent voicing were the most frequent vocal emission manifestation forms.
ConclusionsIn this case series of patients with psychogenic dysphonia, the most frequent form of clinical presentation was conversion aphonia, followed by musculoskeletal tension and intermittent voicing. The clinical and vocal aspects of 28 patients with psychogenic dysphonia, as well as the particularities of each case, are discussed.
Disfonia psicogênica é um distúrbio vocal funcional com diversas manifestações clínicas.
ObjetivoApresentar as características clínicas e vocais de uma série de pacientes com disfonia psicogênica. Tipo de estudo: estudo de série.
MétodoForam incluídos 28 pacientes adultos com disfonia psicogênica atendidos em um Hospital Universitário. Parâmetros analisados: sexo, idade, profissão, sintomas, características vocais, e achados videolaringoestroboscópicos.
Resultados28 pacientes (26 mulheres e dois homens). Profissão: domésticas (n=17), professor (n=4), vendedor (n=4), enfermeiro (n=1), aposentado (n=1) e psicóloga (n=1). Sintomas de inicio súbito reportados por 16 pacientes e progressivo por 12; curso intermitente dos sintomas foi reportado por 15 pacientes. A duração dos sintomas acima de 3 meses foi referido por 21 pacientes. A videolaringoestroboscopia identificou apenas alterações funcionais (nenhum paciente apresentou lesões estruturais ou de mobilidade das pregas vocais). Principais apresentações da disfonia psicogênica: afonia de conversão, tensão músculo esquelética e quebra de sonoridade.
ConclusõesNesta série de casos de pacientes com diagnóstico de disfonia psicogênica a forma de apresentação clínica mais frequente foi a afonia de conversão, seguida pela tensão músculo esquelética e sonoridade intermitente. Discutimos os aspectos clínicos e vocais de 28 pacientes com o diagnóstico de disfonia psicogênica e as particularidades de cada caso.
The somatization of emotional disorders through the voice, termed psychogenic functional dysphonia, has been known for years.1,2 This diagnosis is not always evident during the first contact with the patient; part of the difficulty lies in the different manifestations of this voice disorder. Additionally, patients tend to avoid discussing their emotional conflicts, even when repeatedly questioned, reflecting an initial resistance to the association of the physical symptoms with emotional issues. Another problem in confirming the diagnosis of psychogenic dysphonia is the need to exclude other diseases that may manifest similar vocal symptoms, such as acute infectious diseases, vocal cord paralysis, spasmodic dysphonia, and neuromuscular diseases.3–5
In psychogenic dysphonia, family or professional conflicts are often identified. The respiratory control, vocal intensity, vocal range, vocal resonance, fundamental frequency, articulation, and velocity and intonation of speech may be impaired.1,3 In most cases, more than one vocal parameter is altered, either permanently or not. The onset of vocal symptoms related to psychogenic dysphonia is usually sudden and can be accurately described by the patient.4 The intermittent nature of psychogenic dysphonia is the most prevalent form of evolution, in which periods of normal voice alternate with periods of aphonia or dysphonia.2–6 These fluctuations in vocal emissions are generally observed in the first minutes of the medical consultation, leading the physician to the diagnosis.
Considering the diversity of clinical manifestations displayed by patients with psychogenic dysphonia, the exchange of information among health professionals in order to facilitate diagnosis is valuable. This study aimed to analyze the diversity of clinical and vocal presentations in a case series of patients diagnosed with psychogenic dysphonia.
MethodsThis prospective study included adult patients of both genders, aged >20 years, with a diagnosis of psychogenic dysphonia treated in the Outpatient Clinics of Voice Disorders in a university hospital, from 2002 to 2014. The child and adolescent populations were excluded. Patients were continuously enrolled in the study, and after diagnosis confirmation was obtained through a multidisciplinary assessment by an otorhinolaryngologist, psychologist, and speech therapist. All patients completed the standardized assessment protocol for voice disorders in the clinic and underwent a videolaryngostroboscopy, as well as speech therapy and psychological evaluations.
The videolaryngostroboscopy was always performed by the same otorhinolaryngologist and author of the research, using a rigid telescope (70°, 8mm; Asap – Germany) or flexible nasofibroscope (3.3mm; Olympus – Japan) in those patients who did not allow the examination with the telescope. Images were captured using a conjugated system (multifunctional videosystem type XE – 50, Eco V 50W X – TFT/USB; Carl-Zeiss – Germany).
These examinations assessed the presence of laryngeal lesions, secretions, mucosal color and vocal fold mobility, presence of glottic cleft, presence of abnormal movements, and behavior of the vestibular folds during phonation and inspiration (tension, hyperconstriction). These tests were complemented by laryngostroboscopy (stroboscopic light source – Endo-Stroboscopel Model; Atmos – Germany), assessing the amplitude, symmetry, synchronism, and frequency of muco-undulatory movement, as well as the glottal closure and opening stage.
The following parameters were recorded: gender, age, occupation, characteristics, duration and evolution of the vocal symptoms, videolaryngostroboscopy findings, and vocal emission presentation.
The diagnosis of psychogenic functional dysphonia was established in patients who had vocal symptoms accompanied by normal videolaryngoscopy results, displaying only inadequate functional motor dysfunctions used as phonatory adjustments and suspected psycho-emotional disorder associated with the picture of dysphonia,2,3 confirmed in the psychological and speech therapy assessments. Patients with recent reports of respiratory infections or other comorbidities associated with the current picture of dysphonia were assessed and excluded.
After diagnosis was confirmed, the multidisciplinary therapy (psychotherapy and speech therapy) was initiated in all patients; the duration of the therapy varied from three to six months, with remission of dysphonia at varying intervals for each patient, together with greater psycho-emotional stability in the all cases who received psychotherapeutic support. All patients were followed up for four to six months in outpatient clinics after discharge from psychological and speech therapy, and presented no symptom recurrence during this period.
The classification used to characterize the type of vocal emission was that of Behlau2: conversion aphonia, divergent use of register, falsetto voice, intermittent voicing, skeletal muscle tension syndrome, vestibular dysphonia, dysphonia due to fixed basal register, psychogenic spasmodic dysphonia by adduction, and dysphonia due to paradoxical movements of the vocal folds. Patients with organic laryngeal lesions and with doubtful diagnoses were excluded. The project was approved by the Research Ethics Committee of the Universidade Estadual Paulista Júlio de Mesquita Filho (Plataforma Brasil No. 18033313.6.0000.5411).
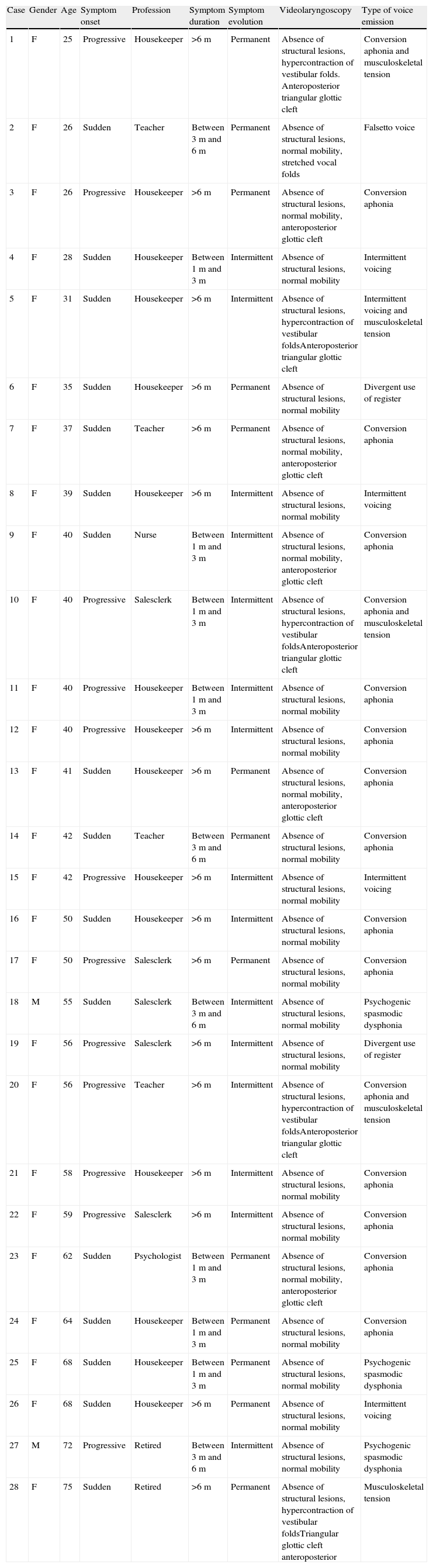
ResultsTable 1 summarizes the parameters assessed in the 28 patients included in the study. Of the 28 patients diagnosed with psychogenic dysphonia, aged 26–78 years, 26 were women and two were men. Sudden symptom onset was reported by a large number of patients (n=16), and symptom duration longer than three months was reported by 21 patients, and intermittent evolution of dysphonia by 15. Regarding occupation, the vast majority of patients were housekeepers (n=18). The most frequent types of vocal presentation were conversion aphonia (n=17), intermittent voicing (n=5), and muscle-skeletal tension (n=5).
Clinical features, videolaryngoscopic findings, and type of voice emission in patients with psychogenic dysphonia.
| Case | Gender | Age | Symptom onset | Profession | Symptom duration | Symptom evolution | Videolaryngoscopy | Type of voice emission |
| 1 | F | 25 | Progressive | Housekeeper | >6m | Permanent | Absence of structural lesions, hypercontraction of vestibular folds. Anteroposterior triangular glottic cleft | Conversion aphonia and musculoskeletal tension |
| 2 | F | 26 | Sudden | Teacher | Between 3m and 6m | Permanent | Absence of structural lesions, normal mobility, stretched vocal folds | Falsetto voice |
| 3 | F | 26 | Progressive | Housekeeper | >6m | Permanent | Absence of structural lesions, normal mobility, anteroposterior glottic cleft | Conversion aphonia |
| 4 | F | 28 | Sudden | Housekeeper | Between 1m and 3m | Intermittent | Absence of structural lesions, normal mobility | Intermittent voicing |
| 5 | F | 31 | Sudden | Housekeeper | >6m | Intermittent | Absence of structural lesions, hypercontraction of vestibular foldsAnteroposterior triangular glottic cleft | Intermittent voicing and musculoskeletal tension |
| 6 | F | 35 | Sudden | Housekeeper | >6m | Permanent | Absence of structural lesions, normal mobility | Divergent use of register |
| 7 | F | 37 | Sudden | Teacher | >6m | Permanent | Absence of structural lesions, normal mobility, anteroposterior glottic cleft | Conversion aphonia |
| 8 | F | 39 | Sudden | Housekeeper | >6m | Intermittent | Absence of structural lesions, normal mobility | Intermittent voicing |
| 9 | F | 40 | Sudden | Nurse | Between 1m and 3m | Intermittent | Absence of structural lesions, normal mobility, anteroposterior glottic cleft | Conversion aphonia |
| 10 | F | 40 | Progressive | Salesclerk | Between 1m and 3m | Intermittent | Absence of structural lesions, hypercontraction of vestibular foldsAnteroposterior triangular glottic cleft | Conversion aphonia and musculoskeletal tension |
| 11 | F | 40 | Progressive | Housekeeper | Between 1m and 3m | Intermittent | Absence of structural lesions, normal mobility | Conversion aphonia |
| 12 | F | 40 | Progressive | Housekeeper | >6m | Intermittent | Absence of structural lesions, normal mobility | Conversion aphonia |
| 13 | F | 41 | Sudden | Housekeeper | >6m | Permanent | Absence of structural lesions, normal mobility, anteroposterior glottic cleft | Conversion aphonia |
| 14 | F | 42 | Sudden | Teacher | Between 3m and 6m | Permanent | Absence of structural lesions, normal mobility | Conversion aphonia |
| 15 | F | 42 | Progressive | Housekeeper | >6m | Intermittent | Absence of structural lesions, normal mobility | Intermittent voicing |
| 16 | F | 50 | Sudden | Housekeeper | >6m | Intermittent | Absence of structural lesions, normal mobility | Conversion aphonia |
| 17 | F | 50 | Progressive | Salesclerk | >6m | Permanent | Absence of structural lesions, normal mobility | Conversion aphonia |
| 18 | M | 55 | Sudden | Salesclerk | Between 3m and 6m | Intermittent | Absence of structural lesions, normal mobility | Psychogenic spasmodic dysphonia |
| 19 | F | 56 | Progressive | Salesclerk | >6m | Intermittent | Absence of structural lesions, normal mobility | Divergent use of register |
| 20 | F | 56 | Progressive | Teacher | >6m | Intermittent | Absence of structural lesions, hypercontraction of vestibular foldsAnteroposterior triangular glottic cleft | Conversion aphonia and musculoskeletal tension |
| 21 | F | 58 | Progressive | Housekeeper | >6m | Intermittent | Absence of structural lesions, normal mobility | Conversion aphonia |
| 22 | F | 59 | Progressive | Salesclerk | >6m | Intermittent | Absence of structural lesions, normal mobility | Conversion aphonia |
| 23 | F | 62 | Sudden | Psychologist | Between 1m and 3m | Permanent | Absence of structural lesions, normal mobility, anteroposterior glottic cleft | Conversion aphonia |
| 24 | F | 64 | Sudden | Housekeeper | Between 1m and 3m | Permanent | Absence of structural lesions, normal mobility | Conversion aphonia |
| 25 | F | 68 | Sudden | Housekeeper | Between 1m and 3m | Permanent | Absence of structural lesions, normal mobility | Psychogenic spasmodic dysphonia |
| 26 | F | 68 | Sudden | Housekeeper | >6m | Permanent | Absence of structural lesions, normal mobility | Intermittent voicing |
| 27 | M | 72 | Progressive | Retired | Between 3m and 6m | Intermittent | Absence of structural lesions, normal mobility | Psychogenic spasmodic dysphonia |
| 28 | F | 75 | Sudden | Retired | >6m | Permanent | Absence of structural lesions, hypercontraction of vestibular foldsTriangular glottic cleft anteroposterior | Musculoskeletal tension |
At the videolaryngostroboscopy assessment, all patients had normal vocal folds, with no structural lesions or mobility alterations. Vestibular fold hyperconstriction was identified in five patients during phonation and anteroposterior triangular glottic cleft. Among patients with conversion aphonia, five had anteroposterior glottic cleft. All patients showed remission of vocal symptoms and better psycho-emotional control after speech therapy and psychological treatment. No patient showed symptom recurrence during the follow-up period.
DiscussionPsychogenic dysphonia is considered a functional voice disorder, as there are no structural laryngeal lesions or neurological alterations directly related to the evident vocal symptoms.2,3,6 Psychogenic dysphonia has been noted to be highly predominant in women,2–5 as we found in this study (26:2). Especially today, with the significant contribution of women to household budgets, the stress and demands of both domestic and professional tasks can be partially responsible for the increased utilization of psychologic and psychiatric consultations among women.5
In this study, most patients were housekeepers and only four patients were teachers. Many authors, however, have emphasized the high incidence of psychogenic dysphonia in teachers, often related to professional overload, as many of them often work two shifts.7
In psychogenic dysphonia, psycho-emotional and psychosocial disorders are usually identified, including anxiety, distress, depression, conversion reaction (including dysphonia), personality disorders, and interpersonal conflicts in the family or professional environment.2,3,8 The predominant age group is between 30 and 50 years of age, the period of professional activity of highest intensity, as we observed in this study. Psychogenic dysphonia is rare in children and adolescents, and when it occurs, it is usually related to the trauma of sexual abuse or death of a close relative.9
Videolaryngoscopic examinations in psychogenic dysphonia do not identify organic laryngeal lesions; however, functional disorders are usually present during phonation, such as tremors, vocal fold adduction in tension, ventricular phonation with hypercontraction and constriction, glottic cleft, and paradoxical movements of the vocal folds. Thus, the videolaryngoscopic assessment is not always capable of differentiating psychogenic dysphonia from other functional dysphonias and stroboscopic, electromyography evaluations, as well as acoustic vocal and auditory-perceptual measures, become important.10–12
The auditory-perceptual and vocal analyses disclose difficulty in maintaining the stability of phonation due to lack of control of the laryngeal muscles. Other findings are varying degrees of musculoskeletal tension and breathiness. The latter is often observed in phonation with glottic insufficiency, and constitutes a valuable resource to minimize the glottic cleft; however, it has also been observed in psychogenic dysphonia and may result in ventricular phonation.
The series of cases depicted in Table 1 shows a prevalence of conversion aphonia, intermittent voicing, and muscle-skeletal tension. Conversion aphonia has been highlighted by several authors as the primary form of psychogenic dysphonia, corroborating the present findings.1,2,4 However, Schalén et al.3 emphasized that this vocal pattern can also be found in inflammatory acute laryngitis and vocal fold paralysis, thus not exclusively associated with emotional disorders, confirming the importance of including such information in the clinical history. These authors conducted a study of 40 patients diagnosed with psychogenic dysphonia and a group of patients with acute infectious laryngitis and found no difference in the pattern of vocal emission between the groups, demonstrating the need to take into account the clinical history and physical examination.
Bader and Schick13 emphasize the frequent delay in the diagnosis of patients with psychogenic dysphonia, culminating in misdiagnosis and mistreatment including unnecessary drugs, such as antibiotics. Reiter et al.14 emphasized the importance of a multidisciplinary approach in the treatment of these patients. Those authors studied 40 patients with psychogenic dysphonia and the treatment benefits (speech therapy and/or psychotherapy therapy) were assessed through the voice handicap index (VHI) protocols. In this group of patients, 70% reported improvement or resolution of vocal symptoms; however, only 37.5% accepted and underwent psychotherapy.
When speech therapy was used alone, only 12.5% of the patients reported vocal symptom improvement. In the present study, the multidisciplinary approach is believed to have been the key to success and good evolution in all patients. Treatment is difficult, strenuous, and protracted in patients resistant to psychotherapy, requiring effort, discipline, and determination by both patient and therapist.2 Sudhir et al.15 and Baker16 reinforced the importance of a multidisciplinary approach in psychogenic dysphonia, emphasizing that it is important to understand the complex association between neuropsychological, intrapsychological, and interpersonal behaviors that affect these patients.
ConclusionIn this case series of patients diagnosed with psychogenic dysphonia, the most frequent form of clinical presentation was conversion aphonia, followed by musculoskeletal tension and intermittent voicing. Considering the diversity in clinical and vocal presentation of patients with psychogenic dysphonia, a multidisciplinary approach (otorhinolaryngologic and psychologic, combined with speech therapy) is crucial to achieve a good outcome in these patients.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Martins RH, Tavares EL, Ranalli PF, Branco A, Pessin AB. Psychogenic dysphonia: diversity of clinical and vocal manifestations in a case series. Braz J Otorhinolaryngol. 2014;80:497–502.
Institution: Universidade Estadual Paulista Júlio de Mesquita Filho (UNESP), Botucatu, SP, Brazil.