Hearing loss has severe emotional, psychological, and social consequences. The early identification of hearing impairment is crucial.
ObjectiveTo evaluate and quantify the knowledge of neonatologists, pediatricians, and residents in pediatrics regarding detection, risk factors, early diagnosis, and referral for rehabilitation of patients with neonatal hearing loss in Jundiaí, state of São Paulo, Brazil.
MethodsThis was a cross-sectional contemporary cohort study including 47 physicians from three hospitals and a questionnaire with 15 items.
ResultsMost of the respondents (83%) had received information about hearing loss in their medical courses, but had no knowledge of techniques for hearing evaluation, and degrees and types of loss. All physicians agreed that in the first six months of life, it is possible to evaluate hearing function and that it is the physician's responsibility to assess the newborn. Regarding the age that the child can receive auditory rehabilitation, the end of the first year and the second year of life predominates.
ConclusionMost respondents know the risk factors for the detection of neonatal hearing impairment, know how to perform procedures, and recognize the importance of diagnosis of hearing loss and the need to refer suspected cases, but most do not know the techniques used to assess hearing in newborns.
A deficiência auditiva acarreta graves consequências emocionais, psicológicas e sociais, sendo imprescindível a identificação precoce de alterações auditivas.
ObjetivoAvaliar e quantificar o conhecimento de médicos neonatologistas, pediatras e residentes em Pediatria, sobre detecção, fatores de risco, diagnóstico precoce e encaminhamento para reabilitação dos pacientes acometidos por deficiência auditiva neonatal no município de Jundiaí, SP.
MétodoEstudo de coorte contemporânea com corte transversal, incluindo 47 médicos de três instituições hospitalares, com aplicação de um questionário de 15 perguntas.
ResultadosGrande parte dos entrevistados (83%) teve informações sobre deficiência auditiva em seus cursos médicos, em sua maioria desconheciam técnicas de avaliação auditiva na infância, graus e tipos de perda. Todos relataram que nos primeiros seis meses de vida já é possível avaliar a audição, sendo dever do médico se preocupar com sua comunicação. Com relação à idade em que a criança pode receber a reabilitação auditiva, predominaram o final do primeiro e o segundo ano de vida.
ConclusãoA maioria dos entrevistados conhece os fatores de risco para a detecção neonatal da deficiência auditiva, realiza procedimentos, reconhece a importância do diagnóstico da deficiência auditiva e a necessidade de efetuar encaminhamento dos casos suspeitos, porém desconhece técnicas de avaliação da audição em neonatos.
Hearing loss has severe consequences for the development of language and communication in children. In addition to emotional, psychological, and social problems, it also affects their families.1 For this reason, the early identification of hearing impairment is essential for early adaptation of hearing aids and auditory stimulation, allowing appropriate development and minimizing the socioeconomic impact of this type of disability. The implementation of the universal newborn hearing screening (UNHS) program allows rapid audiological screening of children for a subsequent further assessment, depending on the need.
In accordance with Resolution 01/99 of the Brazilian Committee on Hearing Loss in Childhood, the UNHS aims to evaluate all newborns,2 and is considered effective if at least 95% of all newborns are evaluated. If there is a failure in the implementation of UNHS, the recommendation is to prioritize newborns at greatest risk of deafness and gradually expand the service to all newborns. The term “screening” refers to the process of applying certain fast and simple measures to a large number of individuals that will identify high probability of disease in the tested function.3 It is not a diagnostic procedure, but rather a method to identify, among asymptomatic individuals, those more likely of presenting the studied disease.3
Thus, it is suggested that UNHS be performed through objective measures (otoacoustic emissions [OAEs]), which can be complemented by the evoked auditory brainstem response (ABR) in the first month of life, after which the diagnosis must be made by three months of age and intervention must be started at six months.3
UNHS is mandatory in accordance with municipal laws in several cities in Brazil,4,5 and it is currently required by Federal Law N° 12,303 of August 2, 2010.6 The law requires that all hospitals and maternity units perform the examination free of charge during the first days of the newborn's life.
The incidence of bilateral hearing loss in healthy newborns is estimated at one to three cases per thousand live births, and from 2% to 4% of children in intensive care units.7 It is estimated that 7–12% of all newborns have at least one risk factor for hearing impairment.8
In recent years, early detection and treatment of hearing loss have gained great importance in pediatric and otorhinolaryngology practice.9 Pediatricians and neonatologists play a key role in interdisciplinary teams that work to prevent hearing loss, as the first professionals who come into contact with newborns. Due to this fact, their evaluation and knowledge about the risk factors for neonatal hearing loss are of utmost importance for the child's audiological follow-up. Teaching (university) hospitals are constantly engaged in the promotion of the theory, research, and practice of interdisciplinarity, but this reality does not always apply to all municipal hospitals.
Therefore, this study aimed to evaluate and quantify, through the use of a questionnaire (Fig. 1), the knowledge of neonatologists, pediatricians, and pediatric residents on risk factors, early diagnosis, and rehabilitation of newborns with hearing impairment in the city of Jundiaí, state of São Paulo, Brazil.
Materials and methodThe study was conducted in three hospitals located in the city of Jundiaí, and the allocation of respondents was randomly performed.
This research was designed as a contemporary cross-sectional cohort study. Data collection consisted of completing a questionnaire, which included eight multiple-choice questions, six yes/no questions, and an essay question. Every time the chosen answer was “yes”, respondents were instructed to expand the answer, describing their conduct.
This questionnaire was the same as that used in the study performed by Colozza and Anastasio,10 with minor changes. Before completing it, respondents were required to sign an informed consent, with the respondent's identification and signature, authorizing participation in the research and use of data. The questionnaires were delivered personally by the author, who witnessed the completion of the questionnaire in order to answer any questions and to ensure that physicians responded immediately. There were no interviews. In each hospital, access to the employees’ shift schedules was obtained in order to approach these professionals in the best manner.
The application of 60 questionnaires was planned, each consisting of 15 questions, including: workplace; conditions to acquire knowledge on congenital hearing loss; knowledge of high-risk factors for hearing loss; conduct when treating a child at high risk for hearing loss; minimum age possible for hearing assessment; hearing assessment in children as a routine; specific tests used in hearing assessment in childhood; degrees and types of hearing loss, including age for referral to the otorhinolaryngologist; appropriate age for hearing aid use; age at which the child can undergo speech therapy; and the physician's responsibility in relation to the child's communication capacity. There were also questions aimed to identify the respondent, such as age, year of graduation, and medical specialty (pediatrics, neonatology, pediatric residency).
This study was approved by the Research Ethics Committee of the Institution under protocol N° 146/2011.
Statistical analysis was conducted by the statistician in charge of the Support Center for Research and Teaching (Núcleo de Apoio à Pesquisa e à Docência – NAPED) of the Institution.
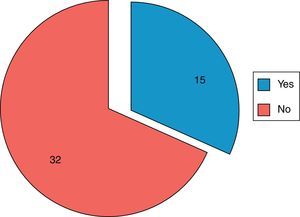
ResultsA total of 47 questionnaires were completed of 60 planned; 13 physicians refused to participate.
The mean age of respondents was 40.58 years and the mean time after graduation was 15.06 years.
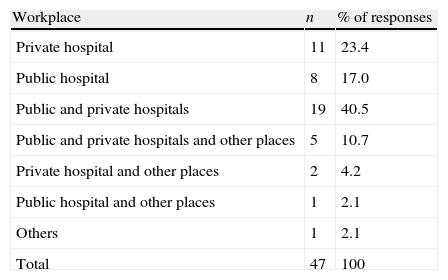
As for the medical specialty of respondents, 26 (55.3%) were pediatricians, 14 (29.8%) were neonatologists, five (10.6%) were residents in pediatrics, and two (4.3%) did not reply to this field. Of the participants, 19 (40.5%) worked in public and private hospitals, 11 (23.4%) only in private hospitals, eight (17%) only in public hospitals, five (10.7%) in private hospitals and other public places (offices and Basic Health Units [BHUs]), two (4.2%) in private hospitals and other places (offices and BHUs), one (2.1%) in a public hospital and elsewhere, and one (2.1%) only elsewhere (Table 1).
Workplace of interviewees (n=47).
| Workplace | n | % of responses |
| Private hospital | 11 | 23.4 |
| Public hospital | 8 | 17.0 |
| Public and private hospitals | 19 | 40.5 |
| Public and private hospitals and other places | 5 | 10.7 |
| Private hospital and other places | 2 | 4.2 |
| Public hospital and other places | 1 | 2.1 |
| Others | 1 | 2.1 |
| Total | 47 | 100 |
Thirty-nine (83%) respondents said they acquired knowledge on congenital hearing loss during the undergraduate course, five (10.6%) said they had taken a specific course, seven (14.9%) had taken other courses, and one (2.7%) did not answer the question, surpassing the total of 100%, considering that three answered “undergraduate course” and “specific course” and two answered “undergraduate course” and “others”. Regarding those who answered “others”, they had to specify their answers and thus, two answered “during residency”, two reported having acquired knowledge through medical literature, and three did not answer.
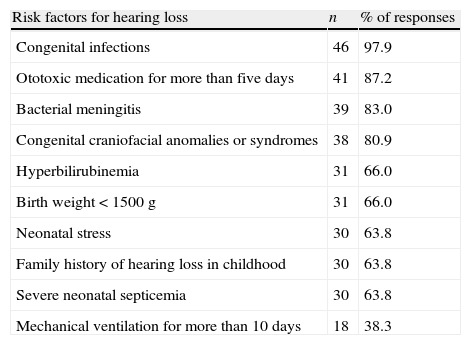
Regarding the question on the presence of “high risk” factors, in descending order and with the possibility of multiple responses, the most often identified were congenital infections (intrauterine or perinatal), identified by 46 (97.9%); ototoxic medication for more than five days, 41 (87.2%); bacterial meningitis, 39 (83%); congenital craniofacial abnormalities or syndromes, 38 (80.9%); hyperbilirubinemia, 31 (66%); birth weight<1500g, 31 (66%); neonatal stress, 30 (63.8%); family history of hearing loss in infancy, 30 (63.8%); severe neonatal sepsis, 30 (63.8%); and mechanical ventilation for more than 10 days, 18 (38.3%) (Table 2).
Risk factors for hearing loss reported by respondents (n=47).
| Risk factors for hearing loss | n | % of responses |
| Congenital infections | 46 | 97.9 |
| Ototoxic medication for more than five days | 41 | 87.2 |
| Bacterial meningitis | 39 | 83.0 |
| Congenital craniofacial anomalies or syndromes | 38 | 80.9 |
| Hyperbilirubinemia | 31 | 66.0 |
| Birth weight<1500g | 31 | 66.0 |
| Neonatal stress | 30 | 63.8 |
| Family history of hearing loss in childhood | 30 | 63.8 |
| Severe neonatal septicemia | 30 | 63.8 |
| Mechanical ventilation for more than 10 days | 18 | 38.3 |
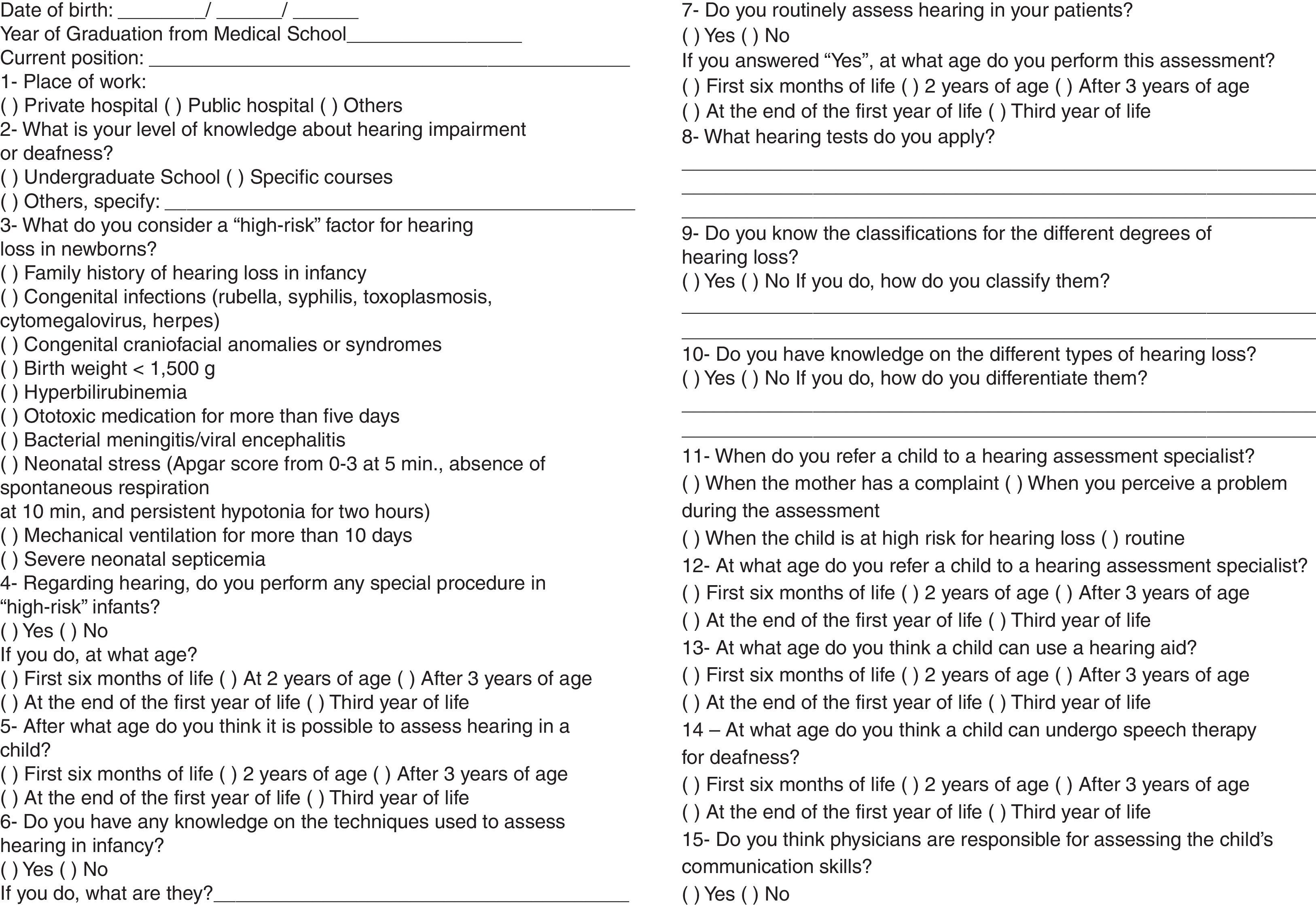
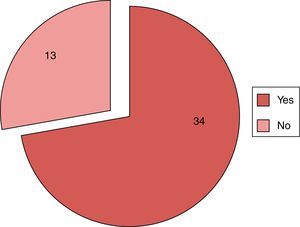
Regarding the question concerning the role of the physician when treating a child at “high risk” for hearing loss, 34 (72.3%) respondents said they performed some type of procedure, while 13 (27.7%) said they did not. Of the affirmative cases, all 34 performed it within the first six months of the child's life (Fig. 2).
Professionals were asked to define at what age hearing could be evaluated in children, and 47 (100%) physicians responded that it is possible to do it within the first six months of a child's life.
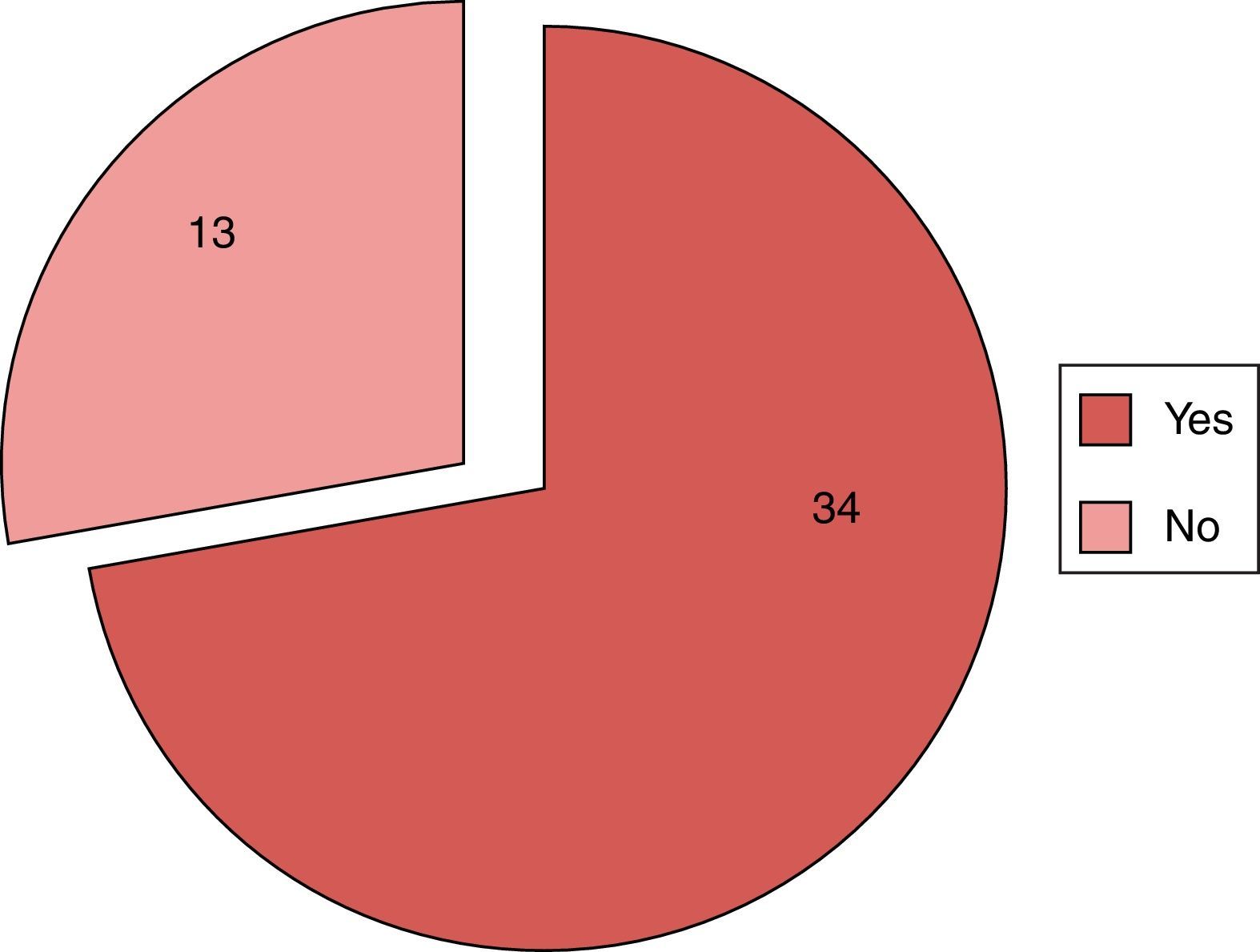
Fifteen (31.9%) reported having knowledge about specific tests to assess hearing in children, and 32 (68.1%) answered no to that question (Fig. 3). Of the affirmative cases, five physicians (33.3%) said they knew of the OAE test, five (33.3%) reported having knowledge of OAE and ABR, two (13.3%) only of ABR, and three (20.1%) did not answer the question.
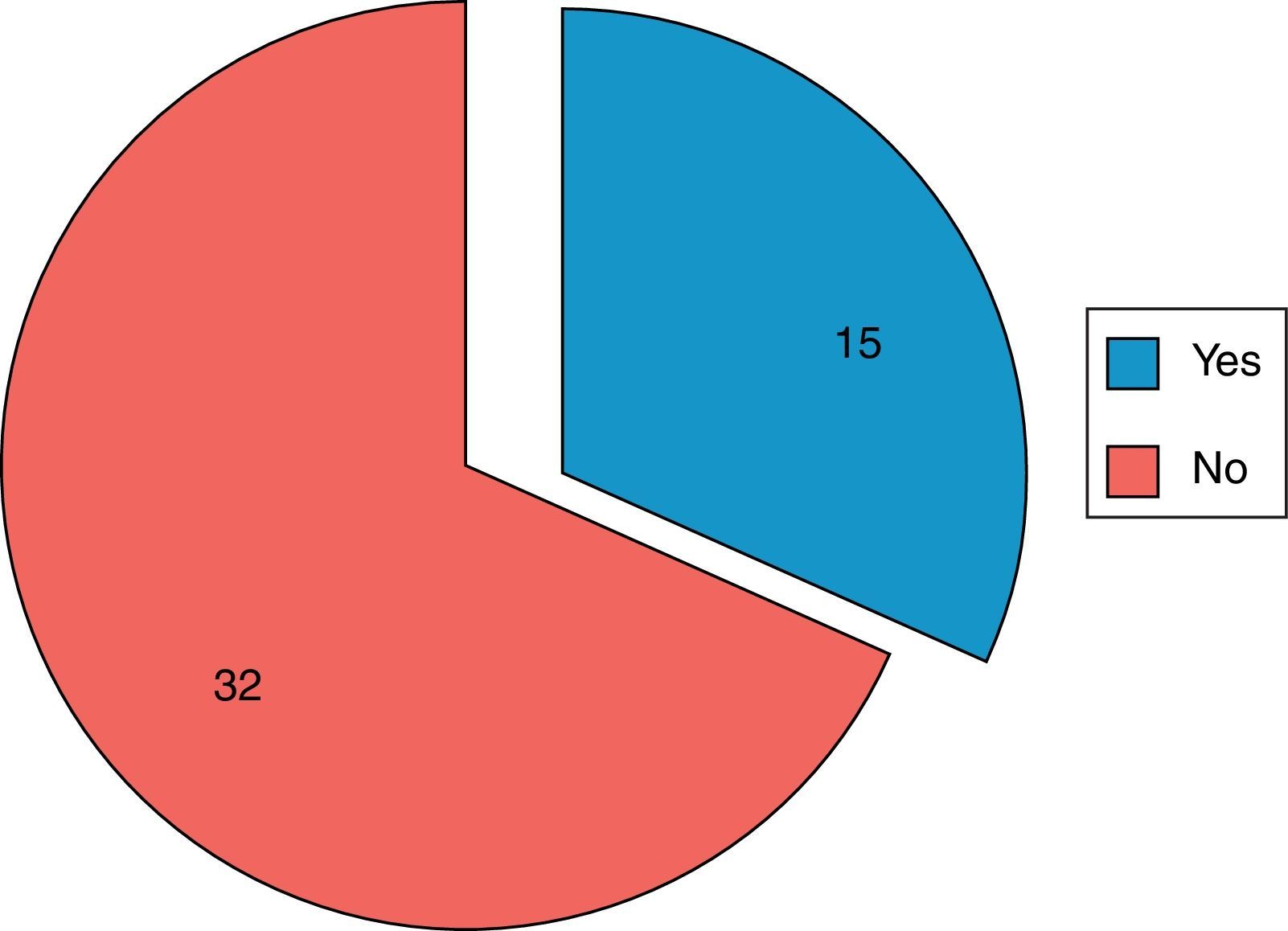
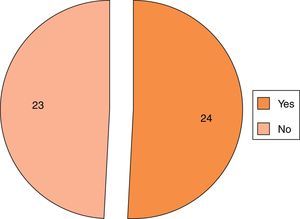
Twenty-four physicians (51.1%) confirmed that they routinely check hearing in their patients, while 23 (48.9%) said they did not check (Fig. 4). Of the 24 who stated that they assess hearing, 22 (91.7%) do so in the first six months of life, one (4.2%) performs the test at the end of the first year, and one (4.2%) did not respond.
Using an open question, respondents were asked which hearing test is applied in the routine care; the responses were diverse. Ten (41.6%) answered that they applied coarse examinations (such as sound stimuli, clapping, rattles, buzzers), eight (33.3%) applied the OAE test, two (8.3%) referred the patients to the audiologist, one (4.1%) performed the ABR (auditory brainstem response) test, one (4.1%) performed the OAE and ABR tests, one (4.1%) performed audiometry, and one (4.1%) did not respond.
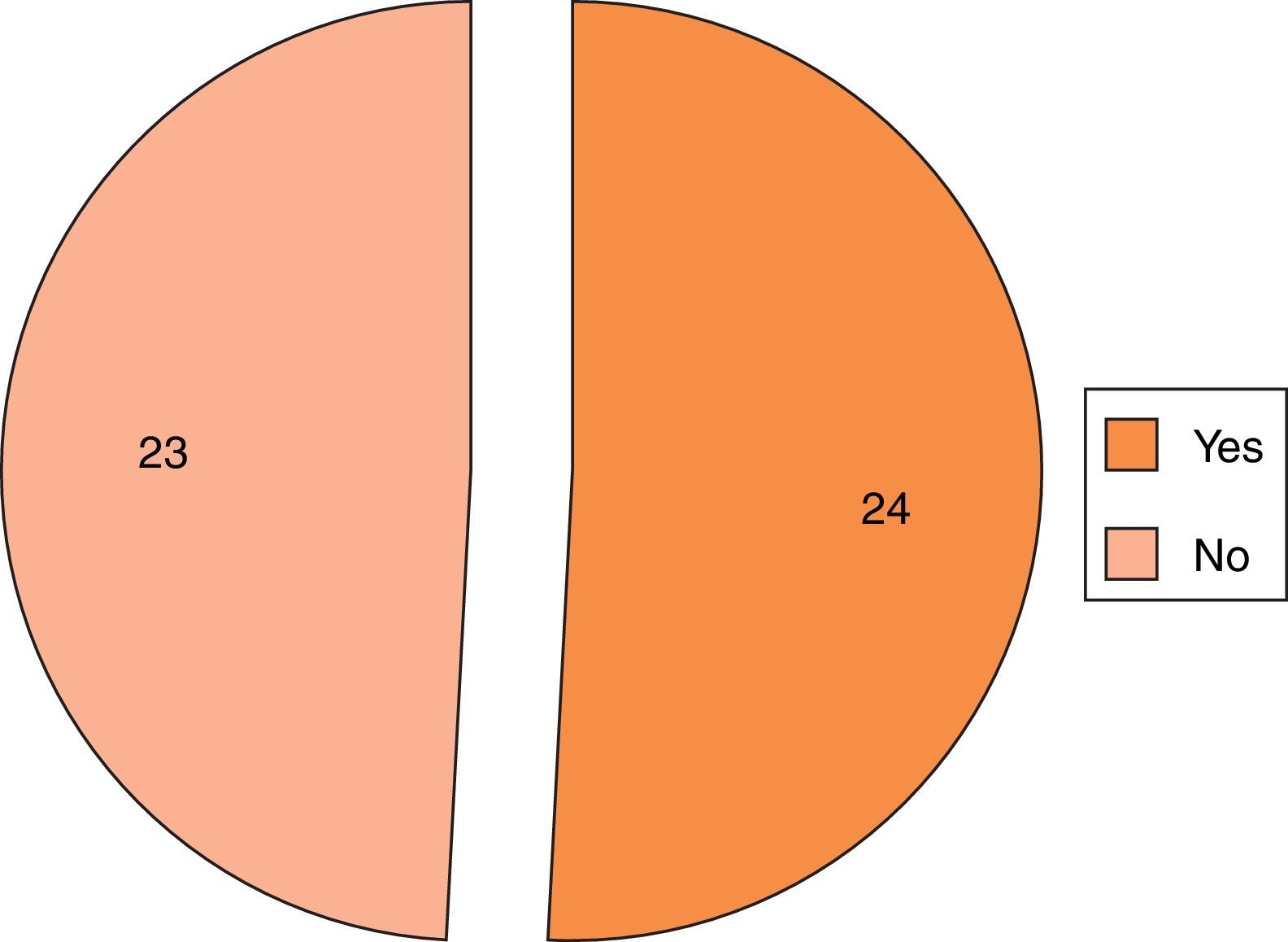
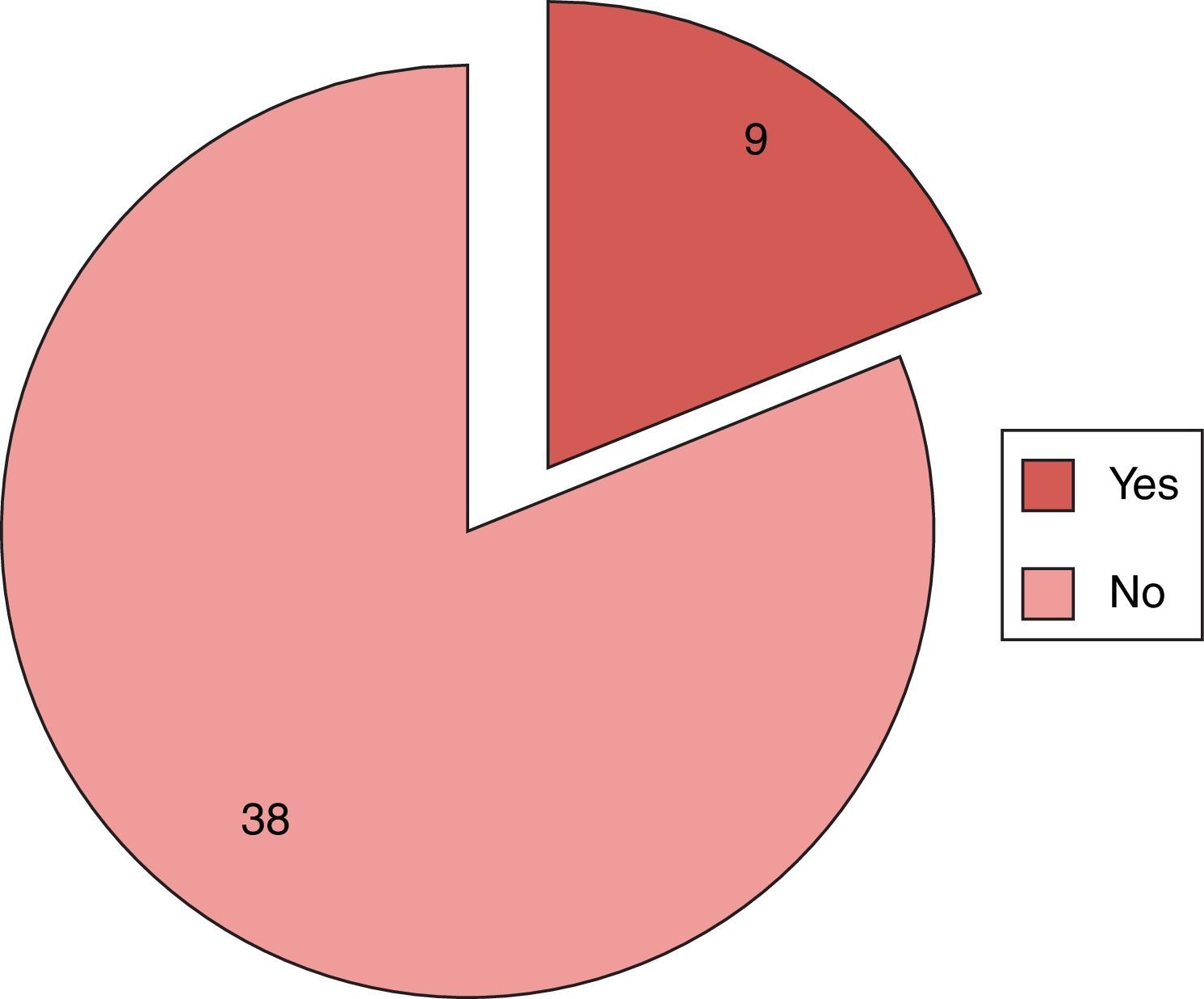
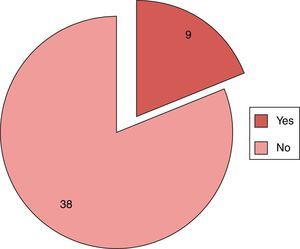
Regarding the knowledge of a classification for different degrees of hearing loss, only nine (19.1%) reported having this knowledge, while 38 (80.9%) said they did not know about it (Fig. 5). Of the affirmative responses, three respondents (33.3%) classified hearing loss as mild, moderate, and severe, one (11.1%) classified it as mild, moderate, severe, and profound, and one (11.1%) classified it as congenital or acquired. Four (44.4%) did not answer the question.
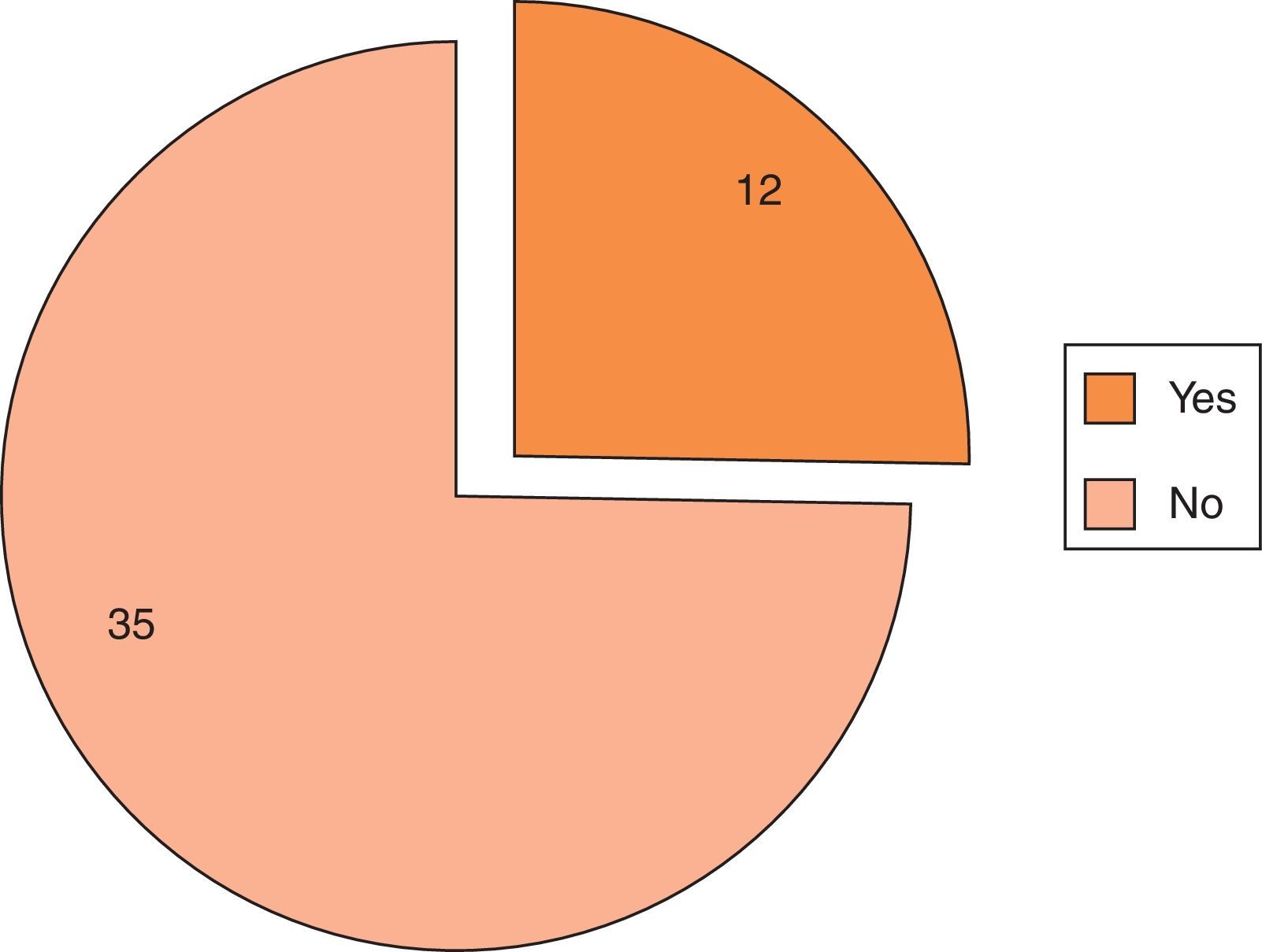
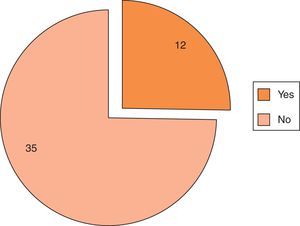
Regarding the question on having knowledge of the different types of hearing loss, 12 (25.5%) answered “yes” and 35 (74.5%) answered “no” (Fig. 6). Participants who answered yes (n=12) had to specify how they differentiated hearing loss: three (25%) answered as “peripheral/central”, three (25%) as “conductive/sensorineural”, and six (50%) did not answer.
Respondents were asked a multiple-choice question with four alternatives, regarding the situation in which the respondent would send a child to a hearing specialist. In descending order, the answers were when you notice something during your assessment, 34 (72.3%); when the mother has a complaint, 29 (61.7%); when the child is at high risk for hearing loss, 28 (59.6%); and as a routine, 15 (31.9%). Seven respondents (14.9%) gave two answers, 20 (42.5%) gave three answers, and four (8.5%) gave four answers.
Regarding the age at which the child should be referred to a specialist, the responses were: 39 (83%) in the first 6 months of age, four (8.5%) at the end of the first year, two (4.2%) in the second year of life and two (4.3%) in the third year of life.
Regarding the age at which the child can wear a hearing aid, 18 (38.3%) said it was possible to use them within the first six months of life, 13 (27.6%) at the end of the first year, eight (17%) in the second year of life, two (4.2%) after 3 years of age, and three (4.2%) in the third year of life. Four respondents (8.5%) did not answer this question.
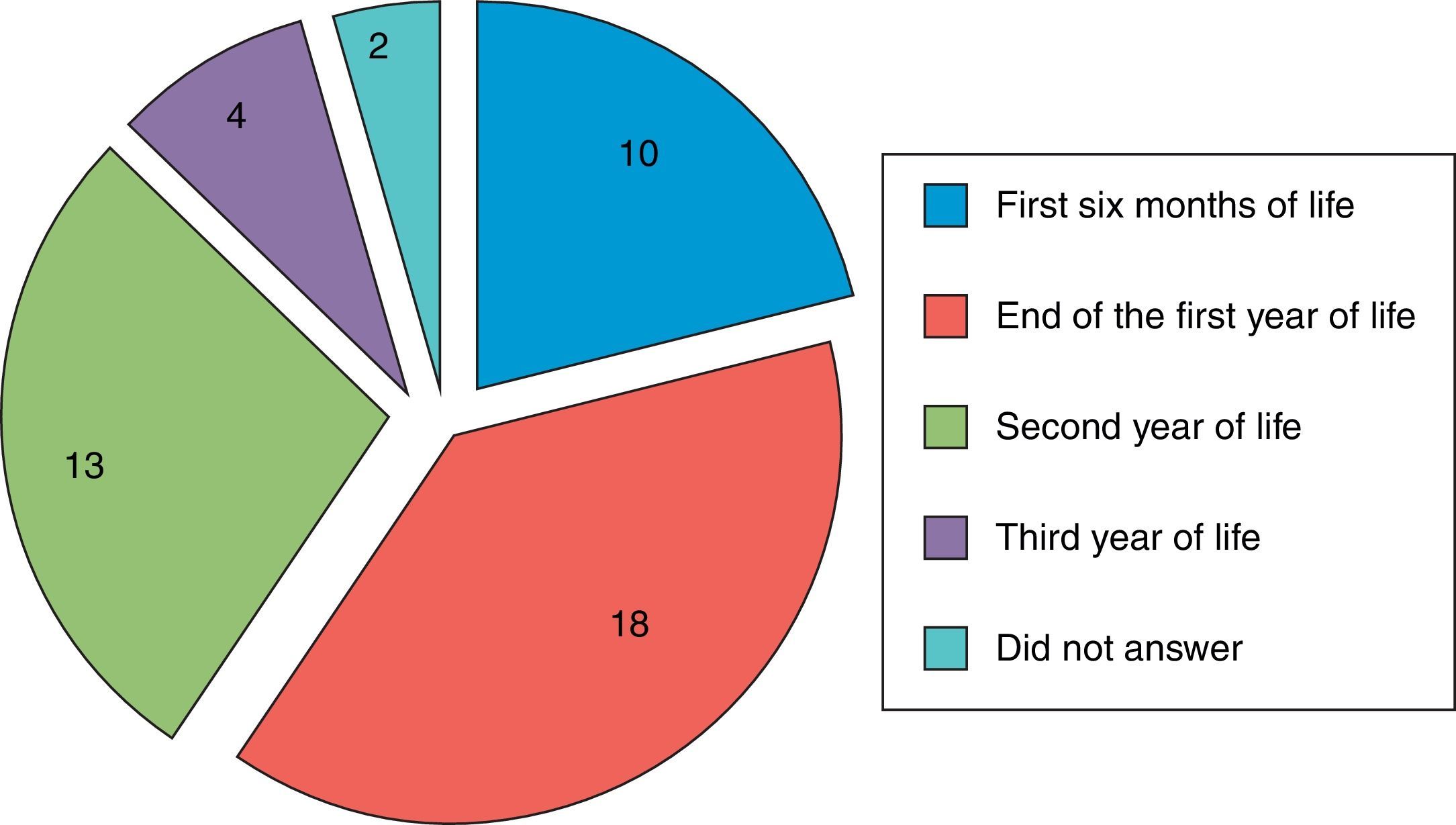
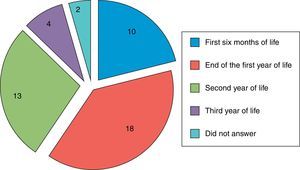
Regarding the question, “at what age the respondent considers that the child can undergo speech therapy for deafness?”, 18 (38.2%) said at the end of the first year of life, 13 (27.7%) in second year, 10 (21.2%) answered within the first six months, four (8.5%) after 3 years of age, and two respondents (4.2%) did not answer this question (Fig. 7).
All participants believe that physicians have the responsibility to assess the child's communication capacity.
DiscussionThe mean age and the time since graduation of the physicians who participated in this study were high, in agreement with the literature,3,11 but different from the study by Colozza and Anastasio,10 in which most of the participants were residents, with a mean age of 34.4 years and time since graduation of 9.9 years. In that study, it can be considered that at the time of graduation and residence of respondents, the UNHS and hearing loss had their dissemination restricted to otorhinolaryngologists and audiologists.
Most participants in the present study were pediatricians (55.3%), whereas the others were neonatologists and medical residents in pediatrics. Colozza and Anastasio10 showed that most respondents were residents (61.1%); two other studies8,12 included pediatricians only, and one study assessed only neonatologists.3 The study sample population represented approximately 15% of pediatricians in the city of Jundiaí, and it was verified that some participants worked in more than one of the selected hospitals, resulting in a more restricted sample.
This study showed a predominance of participants that worked in both private and public hospitals (40.4%). Regarding those working in only one type of hospital, private hospitals predominated. A previously published study10 did not specify the type of hospital where the respondents worked, but most worked in hospitals, and a minority in private clinics and other places.
It can be observed that most of the respondents (83%) reported having obtained information about hearing impairment during medical school, similar to the results found by other studies.3,8,10 In this study, the majority (68.1%) of respondents said they had no knowledge of techniques to assess children's hearing, a finding similar to that in literature.3,8,10 This result may demonstrate that the federal requirement of performing the OAE test did not lead these experts to seek further information on the subject and/or there were no programs that reported the importance of the UNHS, which hampers early diagnosis and treatment.
The present study included 10 risk factors for deafness, considering that the respondents had the possibility of multiple-choice answers for these factors, with 71% positive responses, indicating good knowledge of pediatric and neonatal clinical practice on the subject (Table 2). This result was similar to that found in the literature.3,8,10 The seven criteria of high-risk factors for hearing loss from the Joint Committee on Infant Hearing were mentioned in the literature: family history, intrauterine or perinatal infections, malformations involving the head and neck, neonates weighing less than 1500g at birth, severe neonatal hyperbilirubinemia, bacterial meningitis, and severe hypoxia at birth. Three additional risk factors were included in this study: ototoxic medications, mechanical ventilation, and neonatal septicemia, following the example of another study in the literature.10
All physicians in this study agreed that it is possible to evaluate the child's hearing within the first six months of life, which is in agreement with the literature.10,12 This result shows that physicians are concerned with an early diagnosis of children with risk factors for deafness, thus allowing early treatment and preventing major problems during their development. The Brazilian Committee on Hearing Loss in Childhood (Comitê Brasileiro sobre Perdas Auditivas na Infância – CBPAI) recommends that the UNHS be performed in the first three months of life, and that the educational intervention be performed in the first six months of life.2 There is loss in the overall development of the child if the hearing loss is not detected and treated in a timely manner, with emotional, educational, and social consequences.
With regard to high-risk children, most respondents (72.3%) replied that they perform hearing assessment within the first six months of life, and the majority (68.1%) have no knowledge of techniques to evaluate the child's hearing. In another study,10 75% chose to assess high-risk children in the first six months, and 52.7% of respondents had no knowledge on assessment techniques. Table 2 shows that the respondents have knowledge about the causes of hearing impairment.
Regarding the routine hearing assessment of newborns by the participants, there was a balance between “yes” and “no” responses, consistent with the literature,10 except in one publication,8 which had more positive responses. Regarding the applied tests spontaneously reported by respondents, the OAE, the ABR, and other coarser tests were mentioned, similar to the literature.10 The reported methods are fast, noninvasive, and easily applied.
According to the Bureau International d’Audiophonologie (BIAP),13 hearing loss is classified as mild, moderate, severe, and profound. In the present study, only one physician was able to correctly classify hearing loss. Regarding the types of hearing loss, according to the topographical location, it is classified as: conductive, sensorineural, and mixed. Only three of the respondents correctly described this response, similar to the literature results.8,12
Most respondents reported that they had no knowledge of hearing assessment techniques and were unable to classify the different types and degrees of hearing loss, which is a source of concern, as it suggests literature and undergraduate medical course deficiencies. Similar discussions were conducted in other studies,8,10 that reported that knowing how to define the type and degree of hearing loss is of utmost importance, so that the doctor can perform an appropriate intervention and make a prediction of residual hearing.
Concerning the referral to a specialist in hearing assessment, there are small differences between the responses of this study and the literature.3,8,10,12 Most physicians evaluated in this study (72.3%) reported they refer the child when there is a suspected problem during assessment, whereas another study10 indicated that 80.5% refer the patient when the child is at high risk of hearing loss, although fewer respondents were included. One study3 reported that most choose to routinely send their patients to specialized evaluation, whereas another12 reported that most choose to refer when the mother has a complaint, and a third8 reported a balance of referrals, considering the suspected clinical history or the physician's own clinical suspicion. However, there is an agreement that the child can be referred to a specialist within the first six months of life.
As for the possibility of using a hearing aid, respondents think that it can be used before the end of the first year of life.8,10,12 The literature shows similar results, once again demonstrating the physician's concern in relation to the proper development of patients.
The physicians assessed in this study had different responses regarding the age at which the child can undergo auditory rehabilitation, with a predominance at the end of the first year and the second year of life, a finding that is not in agreement with the literature,10 in which most physicians said that the child can receive this type of treatment as early as six months of life.
All participants believe that it is the doctor's responsibility to assess the child's communication capacity, a finding consistent with other studies.8,10,12
Conclusion and commentsAccording to the results, it is clear that respondents have inadequate and incomplete medical knowledge regarding UNHS and hearing impairment. Although it may be considered that there are conditions and trends for early diagnosis of neonatal deafness, there is also a need for greater exchange between pediatricians, neonatologists, otorhinolaryngologists, and speech therapists, comprising a multidisciplinary team aiming to share information, resulting in better prognosis for these children.
Conflicts of interestThe authors declare no conflicts of interest.
Institution: Faculdade de Medicina de Jundiaí, Jundiaí, SP, Brazil.
Please cite this article as: de Campos AC, Shirane HY, Takemoto PV, Lourenço EA. Universal newborn hearing screening: knowledge of pediatricians and neonatologists in the city of Jundiaí, São Paulo, Brazil. Braz J Otorhinolaryngol. 2014;80:379–85.